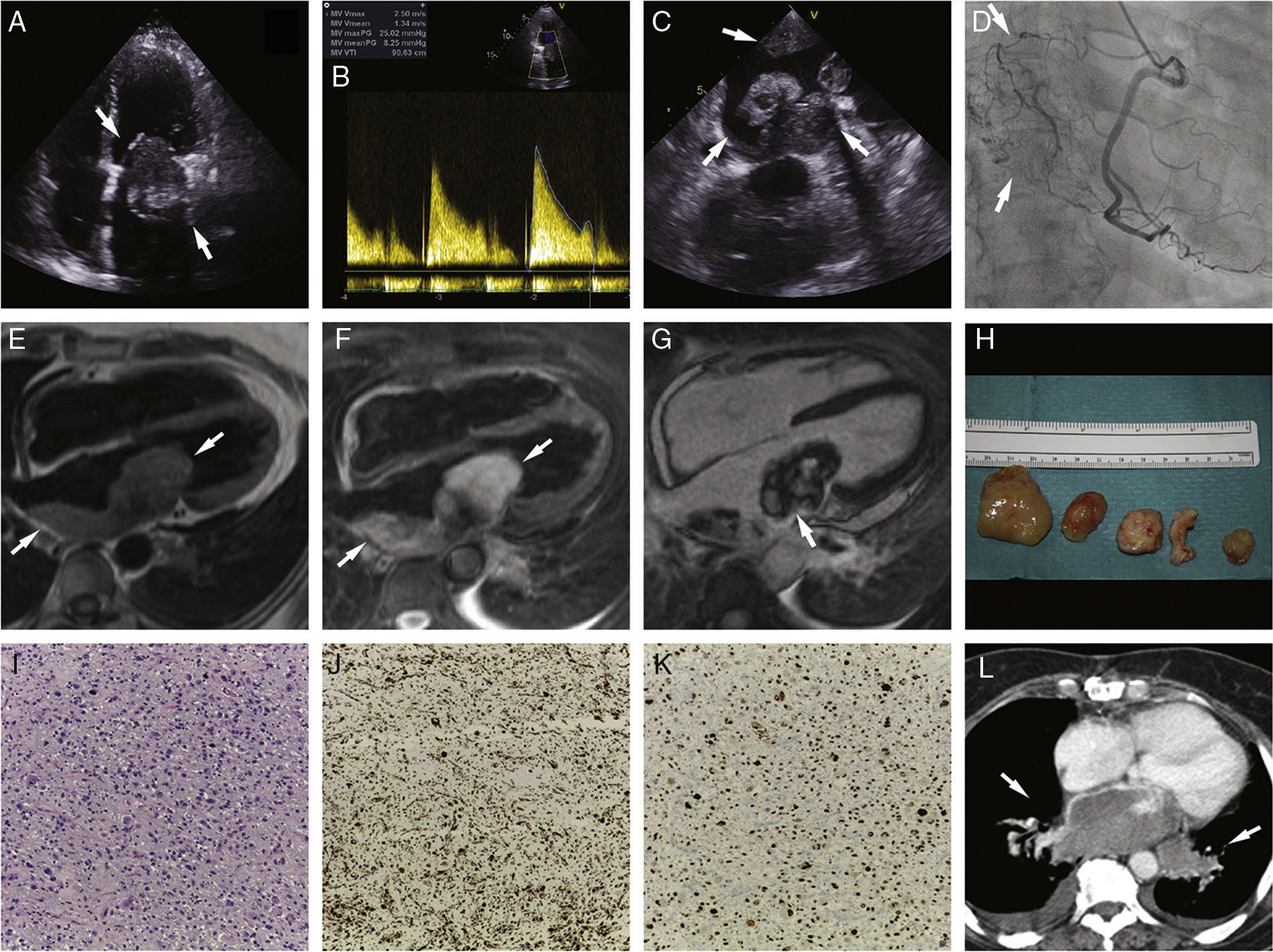
A 70-year-old woman was referred to the emergency department due to mild effort dyspnea, weight loss and night sweats. Transthoracic and transesophageal echocardiography revealed dilated left atrium with an extensive multilobulated mass infiltrating the left atrial posterolateral wall. It prolapsed through the mitral valve during diastole, resulting in elevated mean and peak pressure gradients (8 mmHg and 25 mmHg, respectively [Panels A-C]). Coronary angiography revealed a highly vascularized mass (Panel D, Video 1). Cardiac magnetic resonance (CMR) evidenced the full extension of the mass – measuring 10 cm – in relation to the left atrial posterolateral wall. It extended to both inferior pulmonary veins and revealed tissue characteristics in T1- (isointense) and T2-weighted (hyperintense) images. No contrast uptake was found during first-pass perfusion, but progressive and heterogeneous uptake was observed in the early and late gadolinium enhancement (LGE) images, with a low signal intensity central area (Panels E-G, Video 2 and 3). Computed tomography (CT) staging was negative for metastases. The patient was referred for surgery, but only partial resection was possible (Panel H). Histopathology revealed a malignant neoplasm, with high cellularity, which was predominantly undifferentiated and pleomorphic, with fusiform and epithelioid cells; necrosis areas and a high mitotic index (Panel I); vimentin (Panel J) and nuclear multifocal MDM2 expression (Panel K). These findings are consistent with intimal sarcoma. The patient was not considered to be a candidate for chemotherapy due to the tumor characteristics. One month later, congestive symptoms relapsed. A CT scan confirmed mass growth and pulmonary vein invasion (Panel L). The patient died within a month (Figure 1).
Panel A: Apical four-chamber view showing a dilated left atrium with a large left atrial mass. Panel B: Transmitral gradient recorded from apical approach using continuous wave Doppler across the mitral valve. A mean value of 8 mmHg and a peak of 25 mmHg were observed. Panel C: Off-axis transesophageal image showing multilobulated mass attached to left atrial posterolateral wall. Panel D: 12° Right Anterior Oblique, 15° caudal projection showing high vascularization of the tumor through all three major vascular beds. Panel E: 4-chamber MRI T1-weighted image showing mass isointensity. Panel F: 4-chamber MRI T2-weighted image depicting mass hyperintensity. Panel G: 4-chamber MRI contrast enhanced image revealing heterogeneous uptake after gadolinium contrast administration, with low signal intensity in a central area. Panel H: Macroscopic view of the excised tumor. Panel I: Histopathology: (H&E, ×100) malignant neoplasm, predominantly undifferentiated, with prominent pleomorphism, with fusiform and epithelioid cells; mitotic activity and necrosis that was easy to find. Panel J: (vimentin, ×100) – expression of vimentin in malignant cells (fusiform and epithelioid). Panel K: (MDM2, ×100) – nuclear multifocal expression of MDM2 in malignant cells; all other markers negative (SMA, desmin, CD31, CD34, S100, FVIII, CK8/18, HMB45). Panel L: Post-operative CT showing tumor relapse, with extensive growth into left atrium and pulmonary vein invasion.
CT: computed tomography; MRI: magnetic resonance imaging.
Primary cardiac tumors are rare (incidence <0.03%) and only one quarter is malignant. Intimal sarcomas are mesenchymal tumors and are more commonly encountered in great vessels, so the heart is rarely involved. To our knowledge, only eight cases have been reported to date. These tumors are locally aggressive and proliferate rapidly. Although surgical excision with tumor-free margins is the main treatment, complete surgical excision may often not be possible. The overall prognosis is poor, with a median survival of 3 to 12 months. The effectiveness of chemotherapy and radiotherapy is the subject of debate. In most cases, the cause of death is local tumor enlargement and recurrence.
Echocardiography is the screening method of choice for cardiac tumors (sensitivity 93.3-96%) and is useful for differentiating malignant neoplasms from benign ones. However, due to a limited field of view, the tumor burden may remain underdiagnosed. CMR, which offers multiplanar imaging without restrictions on the field of view, enables the tumor to be accurately located, the extent of involvement to be assessed and the functional impact of the lesion and tissue characterization to be evaluated. In this case, pulmonary vein involvement, broad-based attachment, size greater than 5 cm, ill-defined margins, heterogeneous signal on T1-and T2-weighted images and heterogeneous LGE all led to suspicion of malignancy. However, CMR features are non-specific, with intermediate T1 and high T2 signal intensities and varying amounts of first-pass uptake and LGE. An accurate diagnosis could only be made by histopathology.
In this rare case of mitral valve obstruction, multimodality imaging was crucial to guide diagnosis and treatment.
Conflicts of interestThe authors have no conflicts of interest to declare.