The work presented by Fragata et al. in this issue of the Journal1 on their initial experience of pulmonary thromboendarterectomy in the cardiothoracic surgery department of Hospital de Santa Marta, Lisbon, shows the various faces of a rare disease. Their presentation of this series of cases illustrates how they organized and prepared to acquire expertise in the entire care process for patients with chronic thromboembolic pulmonary hypertension (CTEPH), enabling them to perform pulmonary thromboendarterectomy with good outcomes. They are thus providing an important service for patients in Portugal that reduces the social and economic costs of this treatment by enabling local access to treatment and postoperative care.
A highlight for the Lisbon group was their decision to seek improvements by working with a highly respected center, the Royal Papworth Hospital in the UK. This exchange of experiences shortened the path toward forming their own CTEPH group. It is recommended that patients with CTEPH should be treated by multidisciplinary teams that include specialists in pulmonary hypertension and cardiology and radiologists experienced in pulmonary hypertension imaging, as well as surgical staff.2 Assessment of operability is crucial, requiring input from all members of the team. It is necessary, for instance, to determine whether thromboembolic material is surgically accessible, and that pulmonary vascular resistance (PVR) is proportional to the thromboembolic burden.3
Patient selection is based on various factors, including symptomatic severity and degree of pulmonary hypertension and right ventricular dysfunction. The results of different imaging methods (including pulmonary arteriography, chest computed tomography angiography and ventilation-perfusion scintigraphy) are important in the assessment of operability of CTEPH patients, in order to determine whether the thrombi are proximal or distal. This information gives the surgical team the ability to perform pulmonary thromboendarterectomy in distal thrombi.
According to the classification proposed by the CTEPH group at the University of California, San Diego (UCSD), there are four levels of thromboembolic disease related to organized thrombus. At levels I and II, thrombi are proximal. At level III, the disease is distal and the thrombotic burden starts in the segmental branches, where the disease is often less evident, making thrombus resection a challenge for the surgeon. At level IV, the disease begins in the subsegmental branches and endarterectomy is thus very difficult, requiring extensive surgical experience to achieve hemodynamic improvement in the postoperative period.4
The surgical protocol presented is essential to the operation, in which the team of surgeons, anesthetists and perfusionists work together in harmony to assure adequate cardioprotection and neuroprotection.5 The pulmonary thromboendarterectomy technique described, which is acknowledged to achieve the best results, was developed by the UCSD CTEPH group. A median sternotomy was performed, together with extracorporeal circulation and body temperature reduction to enable safe circulatory arrest, and a clean operative field was ensured.6 Neuroprotective protocols were followed to prevent neurological sequelae due to deep hypothermic circulatory arrest.
The present paper describes two complications: pulmonary artery rupture and postoperative hemoptysis. This information will help teams beginning to operate on CPHT patients to focus attention on the details of successful pulmonary thromboendarterectomy. In view of the risk of bleeding at the pulmonary artery suture line, the UCSD surgical group advises that the arteriotomy should be repaired with a continuous 6-0 polypropylene suture. Another important step when dissecting the thrombus most distal from the edge of the arteriotomy is to preserve the full thickness of the pulmonary artery and thus protect the closure.7 In postoperative management, it is important to avoid hypervolemia and reperfusion syndrome and the excessive use of vasoactive drugs.
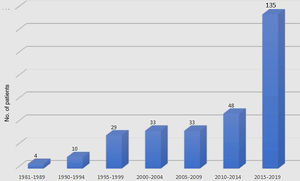
The history of pulmonary thromboendarterectomy at the Heart Institute at Hospital das Clinicas, Faculty of Medicine, University of São Paulo (InCor), began with the pioneering spirit of Dr. Bittencourt in 1981, at a time when everyone was seeking the best technique to perform the operation.8 The UCSD group published a series of cases between 1984 and 1989 with the technique we eventually used.9 In the 1980s, only four operations for CTEPH were performed at InCor. Prof. Fabio Jatene, enthusiastic about the surgical treatment of CTEPH, sought to improve his surgical technique in San Diego with Prof. Stuart Jamieson. After returning to Brazil, he was supported by Prof. Mario Terra Filho, a pulmonologist, and both dedicated themselves to this disease and surgical procedure. During the 1990s, 39 operations10 were performed, with 33 cases being treated in the next five years. In 2013, as there was a backlog of patients with CTEPH awaiting pulmonary thromboendarterectomy, the teams were mobilized, and in that year 24 procedures were performed. In 2014, the CTEPH Group was created and the Pulmonary Circulation team joined it. Since then, between 25 and 30 cases have been performed at InCor each year. Our unit had treated a total of 296 cases up to February 2020, almost half of them in the last five years (Figure 1).
In the last decade, a series of improvements have been made, including formation of the CTEPH Group, a dedicated team overseeing the whole process and the management of the procedure, to discuss operability and other therapeutic options; development of anesthetic and perfusion protocols; improvements in the surgical technique enabling the dissection of distal thrombi; and the creation of a database for the analysis of surgical outcomes.
A recent doctoral thesis compared clinical and surgical outcomes during this period of improvement with the subsequent consolidation phase, from August 2018 to December 2019.11 The comparison showed that postoperative intubation time decreased from 92 to 51 hours, postoperative intensive care unit length of stay from 15 to nine days, mortality from 17.5% to 2.8%, surgery to treat rebleeding from 24.4% to 0%, postoperative pericardial effusion from 11.2% to 8.5%, stroke from 3.0% to 0%, and postoperative acute renal failure (Acute Kidney Injury Network grade 3) from 13.2% to 8.5%. Resections of distal thrombi on the right side increased to 40% and on the left side to 77%. These unpublished data show the importance of a dedicated team in a specialized center.
We would like once again to emphasize the importance of the present paper and to congratulate Professor Fragata and his team.
Conflicts of interestThe authors have no conflicts of interest to declare.