To analyze the impact of reperfusion by either primary percutaneous coronary intervention (PPCI) or fibrinolysis, and mortality rates of a pre-hospital fast-track network for treating patients with ST-elevation myocardial infarction (STEMI).
Methods and ResultsA pre-hospital network for STEMI patients, designated the Green Lane for Acute Myocardial Infarction (GL-AMI), has been implemented in the southern region of Portugal – the Algarve Project. We performed an observational study based on a prospective registry of 1338 patients admitted to Faro Hospital between 2004 and 2009, classified in two groups according to the method of admission: emergency department group (EDG) and GL-AMI group (GLG). More patients from GLG were reperfused (p<0.0001). PPCI was the preferred method of reperfusion, 73.1% in GLG and 45.3% in EDG. Time delays were significantly shorter in GLG, except for pre-hospital delay: pre-hospital delay (p=0.11); door-to-needle (p<0.0001); door-to-balloon (p<0.0001); and delay between symptoms and reperfusion (p<0.0001). In-hospital mortality (4.3% vs 9.2%, p=0.0007) and 6-month mortality (6.3% vs 13.8%, p<0.0001) were significantly lower in GLG.
ConclusionsThe Algarve Project significantly reduced the time delay between onset of symptoms and reperfusion, significantly increased the rate of reperfusion, and significantly reduced in-hospital and six-month mortality.
Analisar o impacto nas taxas de reperfusão por intervenção coronária percutânea primária (PPCI) ou fibrinólise, e na mortalidade de uma rede pré-hospitalar para o tratamento de doentes com enfarte agudo do miocárdio com elevação do segmento ST.
Métodos e ResultadosA rede pré-hospitalar para doentes com enfarte agudo do miocárdio, designada Via Verde para o Enfarte Agudo do Miocárdio (GW-AMI), tem sido implementada na região sul de Portugal - O Projeto Algarve. Realizamos um estudo observacional, baseado num registo prospetivo de 1338 doentes internados no Hospital de Faro entre 2004 e 2009, classificados em dois grupos de acordo com a forma de admissão: grupo do Serviço de Urgência (EDG) e grupo GW-AMI (GTG). Mais doentes do GTG foram reperfundidos (p<0,0001). PPCI foi o método preferencial de reperfusão, 73,1% no GTG e 45,3% no EDG. Os tempos de demora foram significativamente inferiores no GTG, exceto o atraso pré-hospitalar: Tempo pré-hospitalar (p=0,11); Porta-agulha (p<0,0001); Porta-balão (p<0,0001); Tempo sintomas-reperfusão (p<0,0001). As taxas de mortalidade hospitalar (4,3% versuss 9,2%, p=0,0007) e mortalidade aos 6 meses (6,3% versus 13,8%, p<0,0001) foram significativamente inferiores no GTG.
ConclusõesO Projeto Algarve reduziu significativamente os tempos de demora entre o início dos sintomas e reperfusão, aumentou significativamente a taxa de reperfusão e diminuiu significativamente as taxas de mortalidade hospitalar e aos seis meses.
Reperfusion therapy, by either fibrinolysis or primary percutaneous coronary intervention (PPCI), is the most important treatment for patients with STEMI.1 The timelines of reperfusion therapy are crucial because the benefits of this therapy diminish with delays in treatment.2 However, treatment time delays remain excessively long in the real world, reducing the number of patients who could benefit from this treatment strategy.3
Many efforts have been made to reduce the time between onset of symptoms and reperfusion by shortening pre-hospital and in-hospital delays.4 In the present study we analyze the results of the implementation of a pre-hospital network for STEMI patients in the Algarve, the southern region of Portugal, designated the Green Lane for AMI (GL-AMI). The main objective was to evaluate the impact of this program on pre-hospital and in-hospital (door-to-needle and door-to-balloon) delays in STEMI patients admitted to Faro Hospital, the referral hospital with PPCI facilities in the region, between 2004 and 2009. Additionally, reperfusion therapy rates, with fibrinolysis or PPCI, and in-hospital and 6-month mortality were also compared between patients admitted through the GL-AMI pre-hospital network and those admitted via the conventional emergency department (ED) during the study period.
MethodsAlgarve Project pre-hospital networkThe Portuguese National Health Plan for 2004–2010 defined reduction of mortality from acute myocardial infarction (AMI) as a major objective in cardiovascular care, and to this end created the GL-AMI network. In this context, an experimental pre-hospital network to improve the treatment of patients with STEMI has been implemented in our region, named the Algarve Project. It was based on the use of pre-hospital ECG and AMI diagnosis and rapid initiation of reperfusion therapy.
The Algarve (Fig. 1) has a population of about 500000 and an area of 4960km2. Faro Hospital has an intensive coronary care unit (ICCU) and a cath lab providing around-the-clock primary angioplasty facilities, which make it the referral center in the region. A second hospital at Portimão without PCI facilities, 60km from Faro, and four health centers with basic EDs, are network points that can provide thrombolytic therapy to STEMI patients. The distance from these health centers to Faro Hospital is between 18 and 80km, connected by motorway. All of these network points have Life-Pack® equipment with facilities for ECG transmission via modem for a second opinion from the cardiologist in charge of the ICCU in Faro Hospital.
In Portugal there is a national emergency system (INEM) for medical transport of emergent patients, covering all medical emergencies. INEM has a network of Emergency Physician Rapid Response Cars (VMER) with physician, nurse and equipment for advanced life support. INEM is activated by the national emergency number (112), and four regional Referral Centers for Emergency Patients (CODU), one in Faro. There are three VMERs, based in Faro, Albufeira (45km) and Portimão (60km). These can report clinical and ECG data to the CODU and to the ICCU in Faro Hospital, activating the cath lab team. When a patient is suspected of having a STEMI, a pre-hospital diagnostic ECG is performed. If STEMI is confirmed, the patient is transferred to Faro Hospital via GL-AMI and admitted directly, bypassing the ED.
Patients arriving directly at the ED of Faro Hospital are triaged with the Manchester system5 and transferred to the Cardiology Department after STEMI diagnosis. Those who arrive at Portimão Hospital ED are transferred to Faro Hospital after STEMI diagnosis.
Study population and clinical parametersThe data were collected from the Registry of Acute Coronary Syndromes of the Portuguese Society of Cardiology and the database of our Cardiology Department. Six-month follow-up data were obtained from clinical visits or by phone.
Between January 1 2004 and December 31 2009 a total of 1496 patients with STEMI were admitted to Faro Hospital. Patients admitted past the acute phase of AMI, or those transferred from other departments of Faro Hospital, totaling 155 patients, were excluded. In three additional cases, no clinical data were available.
A total of 1338 patients were included in the study. They were classified in two groups according to the method of admission: conventional emergency department group (EDG, n=785) and GL-AMI group (GLG, n=553).
The following time parameters were analyzed and compared between the two groups:
- 1.
Pre-hospital delay (PHD): time between onset of symptoms and admission to Faro Hospital;
- 2.
In-hospital delay (IHD): time between admission to Faro Hospital and reperfusion therapy;
- 3.
Total time between onset of symptoms and reperfusion therapy;
- 4.
Door-to-needle time (DNT), defined as the time between admission to Faro or Portimão Hospital and initiation of fibrinolysis;
- 5.
Door-to-balloon time (DBT), defined as the time between admission to Faro Hospital and first balloon inflation;
- 6.
Rates of reperfusion therapy within the timelines recommended in the guidelines (under 30min for DNT, and 90min for DBT).
We analyzed the following clinical cardiovascular events: stroke, recurrent angina, myocardial infarction, major bleeding (according to TIMI bleeding criteria6), arrhythmias, and cardiogenic shock, and in-hospital and 6-month mortality.
Statistical analysisCategorical variables are expressed as number (%) and continuous variables as mean (standard deviation) in the case of normal distribution or otherwise as median (Q1–Q3). Categorical variables were compared with the use of the chi-square test or Fisher's exact test as appropriate. Normally distributed continuous variables were compared with the Student's t test. For variables that did not have a normal distribution, the Wilcoxon test was applied. A univariate analysis was performed to determine predictors of in-hospital and 6-month mortality in the study population. The following variables were included in the univariate analysis: admission group, age, gender, body mass index, smoking history, diabetes, hypertension, dyslipidemia, stroke, angina history, previous myocardial infarction or revascularization, reperfusion therapy, in-hospital drug treatment, blood pressure at admission and maximum Killip class during hospitalization. Variables that were statistically significant in the univariate analysis were included in a multivariate logistic regression model to determine independent predictors of in-hospital and 6-month mortality. In addition, the 6-month survival curve was plotted using the Kaplan–Meier method. Analyses were conducted with the use of SAS software (version 9.1). A p value of 0.05 or less was considered to indicate statistical significance.
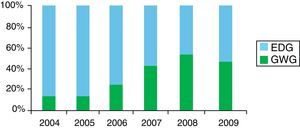
ResultsIn-hospital data were obtained for all patients and the rate of six-month follow-up was 85%. The rate of admission by GL-AMI increased consistently from 2004 (11.6%) to 2009 (60.7%) (Fig. 2). The baseline clinical characteristics of these patients are shown in Table 1. Subjects in EDG were significantly older, less often male and smokers and more often had a history of hypertension, angina and stroke than those in GLG. Subjects in GLG more often had previous PCI.
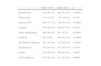
Baseline characteristics of the study population.
| GLG (n=553) | EDG (n=785) | p | |
| Male | 443 (80.1%) | 560 (71.3%) | 0.0003 |
| Age, years | 63 (53–72) | 67 (56–77) | <0.0001 |
| Systolic blood pressure (mmHg) | 138 (118–160) | 140 (120–165) | 0.0341 |
| BMI (kg/m2) | 26.3 (24.2–28.7) | 26 (23.8–28.7) | 0.0947 |
| Diabetes | 99 (17.9%) | 173 (22%) | 0.0642 |
| Hypertension | 271 (49%) | 437 (55.7%) | 0.0162 |
| Dyslipidemia | 214 (38.7%) | 291 (37.1%) | 0.5452 |
| Smoking | 224 (40.5%) | 239 (30.4%) | 0.0001 |
| Previous stroke | 22 (4%) | 55 (7%) | 0.0192 |
| Angina | 118 (21.3%) | 254 (32.4%) | <0.0001 |
| Previous myocardial infarction | 75 (13.6%) | 102 (13%) | 0.7624 |
| Previous PCI | 56 (10.1%) | 53 (6.7%) | 0.0263 |
| Previous CABG | 5 (0.9%) | 16 (2%) | 0.1003 |
| Treatment before admission | |||
| Aspirin | 73 (13.2%) | 117 (14.9%) | 0.3793 |
| Beta-blockers | 48 (8.7%) | 83 (10.6%) | 0.2512 |
| ACE inhibitors | 61 (11%) | 110 (14%) | 0.1077 |
| Statins | 89 (16.1%) | 128 (16.3%) | 0.9176 |
Values are expressed as n (%) or as median (Q1–Q3). ACE: angiotensin-converting enzyme; BMI: body mass index; CABG: coronary artery bypass grafting; EDG: emergency department group; GLG: Green Lane group; PCI: percutaneous coronary intervention.
Table 2 summarizes the angiographic findings in both groups. There were significantly more patients in EDG with three-vessel disease (21.5% vs 13.1% in GLG, p=0.0001).
Overall angiographic findings (independently of culprit lesion).
| GLG (n=533) | EDG (n=688) | p | |
| Normal | 21 (3.9%) | 28 (4.1%) | 0.9087 |
| LMCA | 10 (1.9%) | 16 (2.3%) | 0.5895 |
| 1-vessel disease | 276 (51.8%) | 317 (46.1%) | 0.0478 |
| 2-vessel disease | 166 (31.1%) | 195 (28.3%) | 0.2874 |
| 3-vessel disease | 70 (13.1%) | 148 (21.5%) | 0.0001 |
| Bypass (>50%) | 2 (0.4%) | 8 (1.2%) | 0.1299 |
| LAD (>50%) | 338 (63.4%) | 464 (67.4%) | 0.1416 |
| Cx (>50%) | 188 (35.3%) | 290 (42.1%) | 0.0146 |
| RCA (>50%) | 292 (54.8%) | 397 (57.7%) | 0.3076 |
Values are expressed as n (%). Cx: circumflex; EDG: emergency department group; GLG: Green Lane group; LAD: left anterior descending; LMCA: left main coronary artery; RCA: right coronary artery.
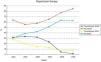
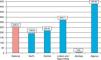
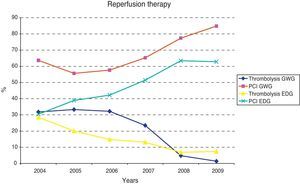
The type and rates of reperfusion therapy are shown in Table 3. More patients in GLG were reperfused (86.3% vs 62.2%; p<0.0001). PPCI was the most frequent method of reperfusion (PPCI 78.8% vs fibrinolysis 21.8%). The percentage of patients undergoing PPCI was higher in GLG (73.1% vs 45.3%, p<0.001). In both groups the number of patients undergoing PPCI increased steadily during the study period (Fig. 3). In most of these patients (63.4%) radial artery access was used.
Type and rates of reperfusion therapy and drug treatment during hospitalization.
| GLG (553) | EDG (785) | p | |
| Reperfusion | 477 (86.3%) | 488 (62.2%) | <0.0001 |
| Fibrinolysis | 73 (13.2%) | 132 (16.8%) | 0.0707 |
| Primary PCI | 404 (73.1%) | 356 (45.3%) | <0.0001 |
| Aspirin | 544 (98.4%) | 766 (97.7%) | 0.3922 |
| Other antiplatelets | 498 (90.2%) | 641 (82%) | <0.0001 |
| LMWH | 430 (78%) | 698 (89.3%) | <0.0001 |
| GP IIb/IIIa inhibitors | 303 (54.9%) | 316 (40.8%) | <0.0001 |
| Betablockers | 355 (64.4%) | 507 (64.7%) | 0.9034 |
| Statins | 523 (94.9%) | 700 (89.7%) | 0.0007 |
| ACE inhibitors | 355 (64.3%) | 511 (65.3%) | 0.6968 |
CABG: coronary artery bypass grafting; EDG: emergency department group; GLG: Green Lane group; GP: glycoprotein; LMWH: low molecular weight heparin; other antiplatelets: mainly clopidogrel; PCI: percutaneous coronary intervention.
Time delays were significantly shorter in GLG, except for PHD, as shown in Table 4. Concerning the rate of patients treated within the appropriate timelines according to current guidelines, there were also significant differences between the groups. DNT of less than 30min was achieved in 71.4% of patients of GLG compared to 14.7% in EDG (p<0.0001). Among patients who underwent PPCI, DBT of less than 90min was achieved in 96.5% of cases in GLG vs 48.6% in EDG (p<0.0001).
Delays from onset of symptoms to hospital admission and reperfusion.
| GLG (min) | EDG (min) | p | |
| PHD | 210 (140–347) | 225 (119–593) | 0.1171 |
| IHD | 20 (15–33) | 86 (56–132) | <0.0001 |
| DNT | 15 (6–30) | 67 (41–119) | <0.0001 |
| DBT | 20 (15–33) | 90 (61–147) | <0.0001 |
| SRT | 225 (160–348) | 285 (180–435) | <0.0001 |
Values are expressed as median (Q1–Q3). DBT: door-to-balloon time; DNT: door-to-needle time; EDG: emergency department group; GLG: Green Lane group; IHD: in-hospital delay; PHD: pre-hospital delay; SRT: total time between onset of symptoms and reperfusion.
Hospital stay (median [Q1–Q3]) was also shorter in GLG (5 days [4–6] vs 6 days [5–8] in EDG, p<0.0001). Median (median [Q1–Q3]) left ventricular ejection fraction was similar in both groups: 62% (51–71) in GLG vs 63% (52–73) in EDG.
Incidence of in-hospital cardiovascular events was lower in GLG, but without statistical significance (15.7% [12.8–19.0] in GLG vs 18.1% [15.5–21] in EDG, p=0.2597) (Table 5). Ischemic events were more common in EDG, whereas incidence of cardiogenic shock was similar in both groups. At hospital discharge, there were no significant differences in the percentage of patients treated with aspirin, statins, beta-blockers or ACE inhibitors.
Cardiovascular complications during hospitalization.
| GLG | EDG | p | |
| Ischemic | 7 (1.3%) | 34 (4.3%) | 0.0014 |
| Major bleeding | 12 (2.2%) | 9 (1.1%) | 0.1380 |
| Mechanical complications | 9 (1.6%) | 24 (3.1%) | 0.0968 |
| Mechanical ventilation | 24 (4.3%) | 32 (4.1%) | 0.8126 |
| Ischemic stroke | 2 (0.4%) | 6 (0.8%) | 0.3468 |
| Arrhythmias | 57 (10.3%) | 78 (9.9%) | 0.8244 |
| Cardiogenic shock (Killip class IV) | 54 (9.8%) | 95 (12.1%) | 0.1809 |
| Death | 24 (4.3%) | 72 (9.2%) | 0.0007 |
Ischemic complications: include angina and myocardial infarction. Arrhythmias: include ventricular fibrillation, 2nd or 3rd degree atrioventricular block or need for temporary pacemaker. EDG: emergency department group; GLG: Green Lane group.
In-hospital mortality: During hospitalization 24 patients (4.3% [95% CI 2.8–6.4]) died in GLG and 72 (9.2% [7.2–11.4]) in EDG; p=0.0007. In multivariate logistic regression analysis the only factors associated with higher in-hospital mortality were older age and cardiogenic shock (Killip class IV). Admission through GL-AMI and treatment with statins and ACE inhibitors during hospitalization were all associated with lower in-hospital mortality, as shown in Table 6.
In-hospital mortality (univariate and multivariate analysis).
| Variable | Univariate analysis | Multivariate analysis | ||
| p | OR (95% CI) | p | OR (95% CI) | |
| Aspirin | <0.0001 | 0.17 (0.07–0.40) | – | |
| Admission method (GLG vs EDG) | 0.0010 | 0.45 (0.28–0.72) | 0.0152 | 0.43 (0.22–0.85) |
| Age | <0.0001 | 1.09 (1.06–1.11) | <0.0001 | 1.05 (1.03–1.08) |
| Beta-blockers | <0.0001 | 0.11 (0.07–0.19) | – | |
| Heart rate | <0.0001 | 1.02 (1.01–1.03) | – | |
| Diabetes | 0.0065 | 1.88 (1.19–2.96) | – | |
| Diastolic blood pressure | <0.0001 | 0.96 (0.95–0.97) | – | |
| Dyslipidemia | 0.0268 | 0.59 (0.37–0.94) | – | |
| Statins | <0.0001 | 0.06 (0.04–0.10) | <0.0001 | 0.16 (0.08–0.30) |
| LMWH | 0.0106 | 0.52 (0.32–0.86) | – | |
| ACE inhibitors | <0.0001 | 0.21 (0.14–0.34) | <0.0001 | 0.27 (0.15–0.49) |
| Killip class (IV vs I–III) | <0.0001 | 37.12 (22.53–61.16) | <0.0001 | 21.5 (12–38.6) |
| Reperfusion | 0.0002 | 0.45 (0.29–0.68) | – | |
| Male vs female | <0.0001 | 0.3 (0.20–0.46) | – | |
| Systolic blood pressure | <0.0001 | 0.98 (0.97–0.98) | – | |
| GP IIb/IIIa inhibitors | <0.0001 | 0.23 (0.14–0.40) | – | |
| Smoking | <0.0001 | 0.2 (0.10–0.39) | – | |
CI: confidence interval; EDG: emergency department group; GLG: Green Lane group; LMWH: low molecular weight heparin; GP: glycoprotein; OR: odds ratio.
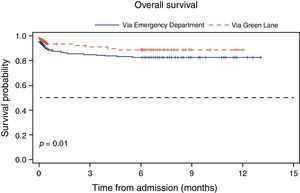
Six-month mortality: Six months after hospitalization the mortality rate remained significantly lower in GLG (6.3% [4.4–8.7] vs 13.8% in EDG [11.4–16.4], p<0.0001). Variables associated with higher 6-month mortality were age and cardiogenic shock (Killip class IV). Admission by GL-AMI and treatment with beta-blockers, statins and ACE inhibitors were all associated with a lower mortality risk (Table 7). Kaplan–Meier survival estimates during follow-up are shown in Fig. 4.
6-month mortality (univariate and multivariate analysis).
| Variable | Univariate analysis | Multivariate analysis | ||
| p | OR (95% CI) | p | OR (95% CI) | |
| Aspirin (in hospital) | <0.0001 | 0.16 (0.07–0.36) | – | |
| Admission method (GLG vs EDG) | <0.0001 | 0.42 (0.28–0.63) | 0.0200 | 0.53 (0.31–0.90) |
| Age | <0.0001 | 1.08 (1.07–1.10) | <0.0001 | 1.05 (1.03–1.07) |
| Previous angina | 0.0163 | 1.56 (1.09–2.25) | – | |
| Beta-blockers (in hospital) | <0.0001 | 0.19 (0.13–0.28) | 0.0119 | 0.53 (0.32–0.87) |
| Heart rate | <0.0001 | 1.02 (1.02–1.03) | – | |
| Diabetes | 0.0012 | 1.88 (1.28–2.77) | – | |
| Dyslipidemia | 0.0022 | 0.54 (0.37–0.80) | – | |
| Statins (in hospital) | <0.0001 | 0.08 (0.05–0.12) | <0.0001 | 0.22 (0.12–0.40) |
| ACE inhibitors (in hospital) | <0.0001 | 0.39 (0.28–0.56) | 0.0053 | 0.51 (0.31–0.82) |
| Killip class (IV vs I–III) | <0.0001 | 20.7 (13.70–31.20) | <0.0001 | 10.8 (6.5–18) |
| Reperfusion | <0.0001 | 0.37 (0.26–0.52) | – | |
| Male vs female | <0.0001 | 0.32 (0.22–0.45) | – | |
| Systolic blood pressure | <0.0001 | 0.98 (0.98–0.99) | – | |
| Previous stroke | 0.0012 | 2.55 (1.44–4.51) | – | |
| GP IIb/IIIa inhibitors | <0.0001 | 0.24 (0.16–0.37) | – | |
| Smoking | <0.0001 | 0.28 (0.17–0.45) | – | |
CI: confidence interval; EDG: emergency department group; GLG: Green Lane group; LMWH: low molecular weight heparin; GP: glycoprotein; OR: odds ratio.
Reperfusion therapy administered to eligible STEMI patients reduces the risk of death from all causes.1 However, the efficacy of this therapy decreases with delays in treatment. Time to reperfusion has emerged as an indicator of quality of care for patients with STEMI.7 Timely reperfusion for STEMI, defined in current guidelines as the provision of fibrinolysis or PCI within 30 and 90min after first medical contact, respectively, has been incorporated in the guidelines as a Class I recommendation. Primary PCI is becoming the reperfusion strategy of choice in most centers equipped with catheterization facilities.8,9 In order to reduce treatment delays, strategies are needed to enable earlier diagnosis of patients with STEMI and rapid transfer to those centers. Several non-randomized observational reports and randomized trials have confirmed the feasibility and safety of transporting patients with acute myocardial infarction to tertiary centers for primary coronary angioplasty.10–13
In Portugal, EDs in most National Health System hospitals are overloaded, due to patients’ lack of rapid access to primary care. This is an important issue, which has led us to bypass the ED and admit patients directly to the cath lab or ICCU. For patients who go to the ED by their own means, measures have been taken to reduce delays, including ECG in the first 10min on the Manchester triage system, in suspected AMI patients.5
The results of the Algarve Project study show that the implementation of a pre-hospital network to improve treatment of STEMI patients is feasible and safe. Furthermore, the use of pre-hospital ECG combined with ED bypass and direct transfer to the cath lab has reduced the total time between onset of symptoms and reperfusion therapy by 60min, in a real-world setting. Previous studies have shown similar results with average reductions of about 45min compared with the conventional ED route.12 In STEMI patients, a close relationship between 1-year mortality rates and time from onset of symptoms to reperfusion has been reported.14,15 Transferring patients from a hospital without PCI facilities can prolong time to primary PCI. In the current era, total DBT for these transferred patients is less than 2h in a little more than a quarter of cases, and 4h or more in about 20%.3,16 Regarding thrombolysis, even in urban areas and under optimal conditions, pre-hospital thrombolysis may not be initiated until a median of 40–50min after the ambulance call, and even longer in cases of in-hospital fibrinolysis.17 In the present study, comparing the two groups (GLG vs EDG), in the former DBT was reduced by 70min and DNT by 52min. As a consequence, a higher percentage of patients achieved in-time reperfusion therapy in accordance with the guidelines in GLG than in EDG (71.4% vs 14.7% in patients undergoing thrombolysis and 96.5% vs 48.6% in those undergoing PCI). In our opinion, the factors that help reduce delay from onset of symptoms to reperfusion therapy are training of health professionals at all network check-points, pre-hospital ECG diagnosis, a high rate of ECG transmission to the referral center, medicalized transport of patients, AMI kits for diagnosis and treatment at all check-points of the network, pre-hospital activation of the cath lab, and bypass of the conventional ED. In addition, public campaigns could also explain why GL-AMI use has increased over time (Fig. 2).
Previous studies have not demonstrated an effect of referral route on early mortality.12 An association between treatment delay and mortality has emerged in other studies only after one year of follow-up and especially in high-risk patients.2 We found significantly lower in-hospital and 6-month mortality in GLG. It should be pointed out that differences in the baseline clinical characteristics of the two groups may act as confounding factors. A higher prevalence of risk factors was apparent in patients from EDG (older, more often female, and with higher rates of history of angina and stroke, among others). Nevertheless, hospital admission by GL-AMI remained as an independent predictor of lower in-hospital and 6-month mortality. Cardiogenic shock was also associated with higher in-hospital and 6-month mortality but its incidence was similar in both groups. The factors that can explain the lower mortality risk in GLG are: (a) in GLG a higher number of patients underwent PPCI, which is known to improve survival compared to fibrinolysis; (b) in GLG patients were processed quickly, with shorter DBT and DNT; (c) PPCI was performed in a high-volume center, which has been related to lower mortality18; (d) during hospitalization there were more ischemic events (angina and reinfarction) in EDG, contributing to higher mortality; and (e) more patients in GLG were treated with aspirin and clopidogrel, probably due to the higher rate of PPCI.
The rate of major bleeding was similar in both groups, but lower compared to other trials,19 probably influenced by the high rates of radial artery access in our center. The radial artery access strategy had no influence on DBT.
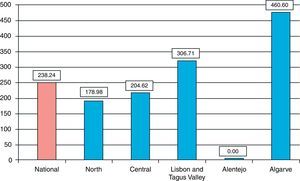
A broader implementation of a pre-hospital network like GL-AMI should take into account not only geographic and logistic issues, but also patient behavior patterns that could limit the overall effectiveness of this strategy. Although treatment of STEMI has improved significantly in recent years, we should not forget that a significant percentage of patients still die before reaching the hospital.20 Previous studies have shown that most STEMI patients use the emergency numbers (such as 112) too late, and only a minority choose to contact the ambulance service.21 In our study the reduction in treatment delay was mainly due to a shorter in-hospital delay in GLG, through ED bypass and direct admission to the cath lab, following activation of the emergency phone number, and clinical evaluation by the pre-hospital emergency team. Pre-hospital ECG diagnosis is one of the cornerstones of such networks, resulting in effective decreases in treatment delays. ECG transmission to the ICCU can further improve diagnostic accuracy and early activation of the cath lab team.22 Such strategies have helped to achieve a rate of 460.6 PPCI per million population in the Algarve region in 200823 (Fig. 5).
LimitationsThis was an observational, non-randomized study, based on a prospective registry. However, its results may be influenced by several referral biases. There were significant differences in baseline clinical characteristics between the groups. Although we have taken into account these possible confounding factors in the statistical models by multivariate analysis, there may have been other variables which could have affected the results. This is a real-world study, without exclusion criteria for admission, including patients in shock or after successful pre-hospital resuscitation. The mortality rates are markedly lower than in several randomized trials and with an improving trend in the last years of the study. There is likely to be an association between lower mortality and the growth of the GL-AMI pre-hospital network. International multicenter studies and meta-analyses with greater statistical power would be needed to corroborate the reductions in in-hospital and long-term mortality of similar clinical networks, although we recognize the serious difficulties in performing randomized trials in this field.24
ConclusionsThe Algarve Project is a regionally organized clinical network, based on pre-hospital AMI diagnosis and direct transport to a referral hospital with PCI facilities in a real-world scenario. It is associated with a significant reduction in treatment delay, a significant increase in reperfusion rates of STEMI patients and higher rates of PPCI per million population. Hospital admission via GL-AMI is also associated with a significant reduction in mortality (in-hospital and at 6 months). These results encourage us to recommend the implementation of a network like GL-AMI in other regions of Portugal and other countries.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are grateful to all the staff of the Cardiology Department of Faro Hospital, the health centers and INEM Algarve.