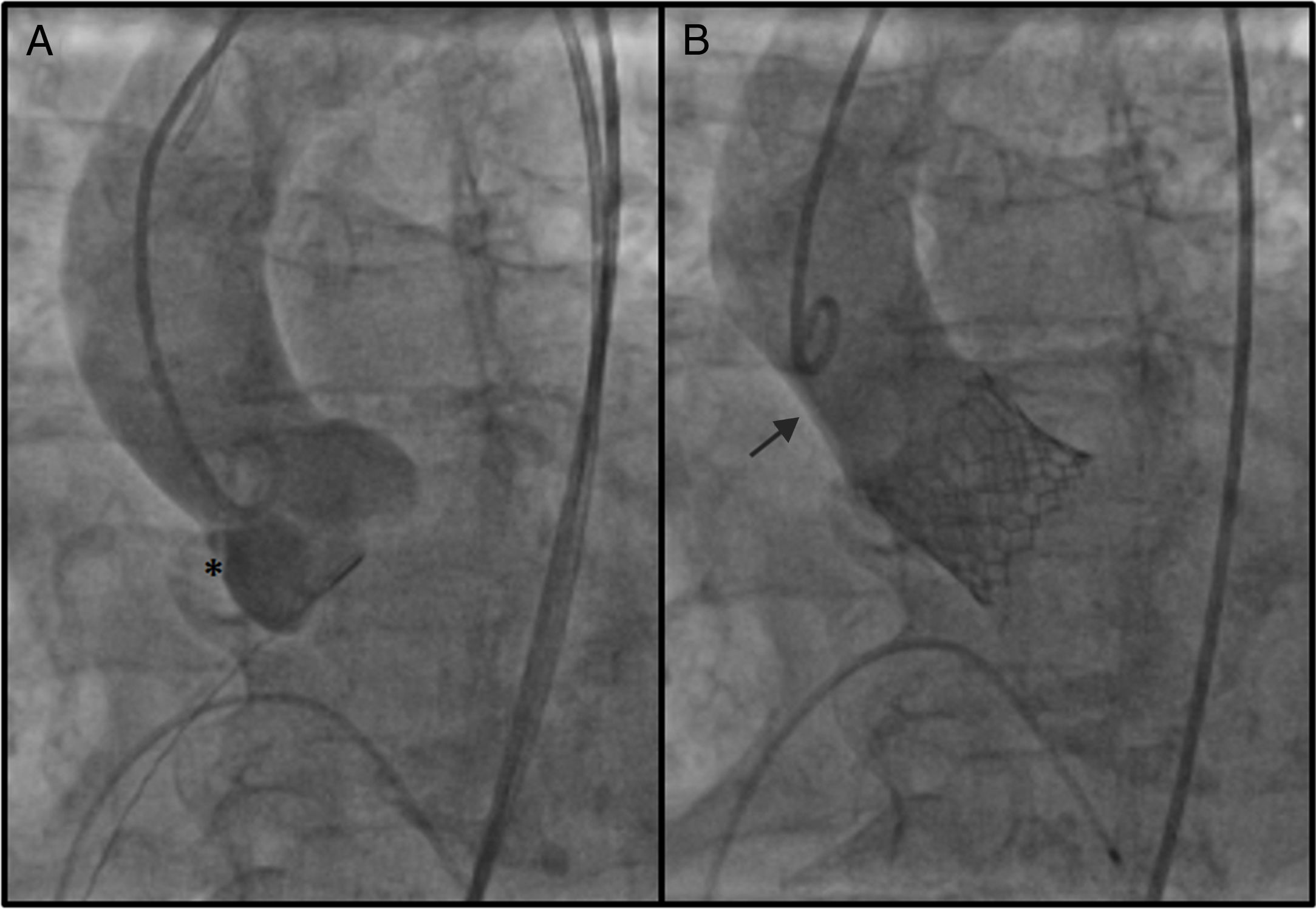
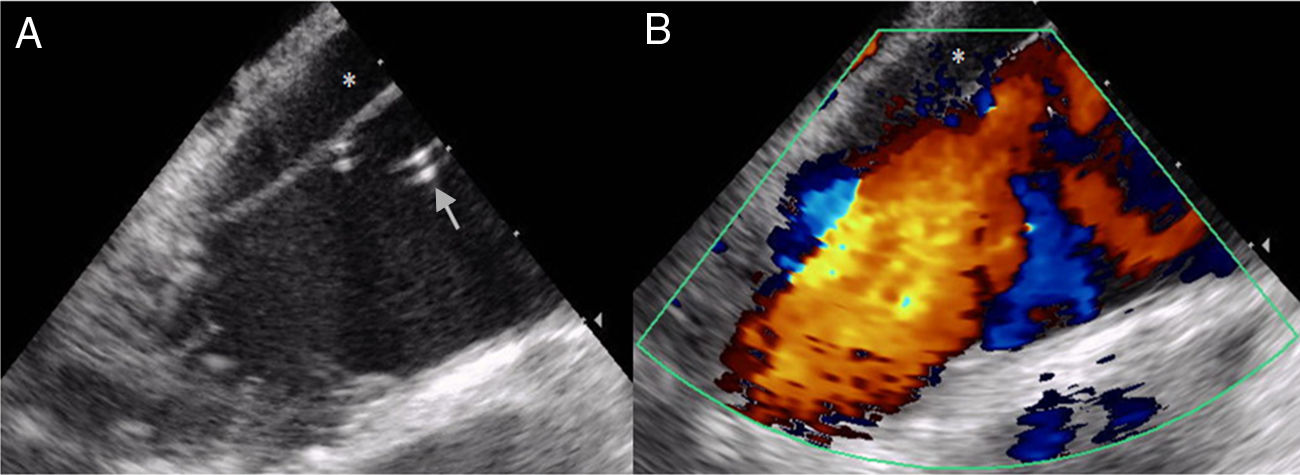
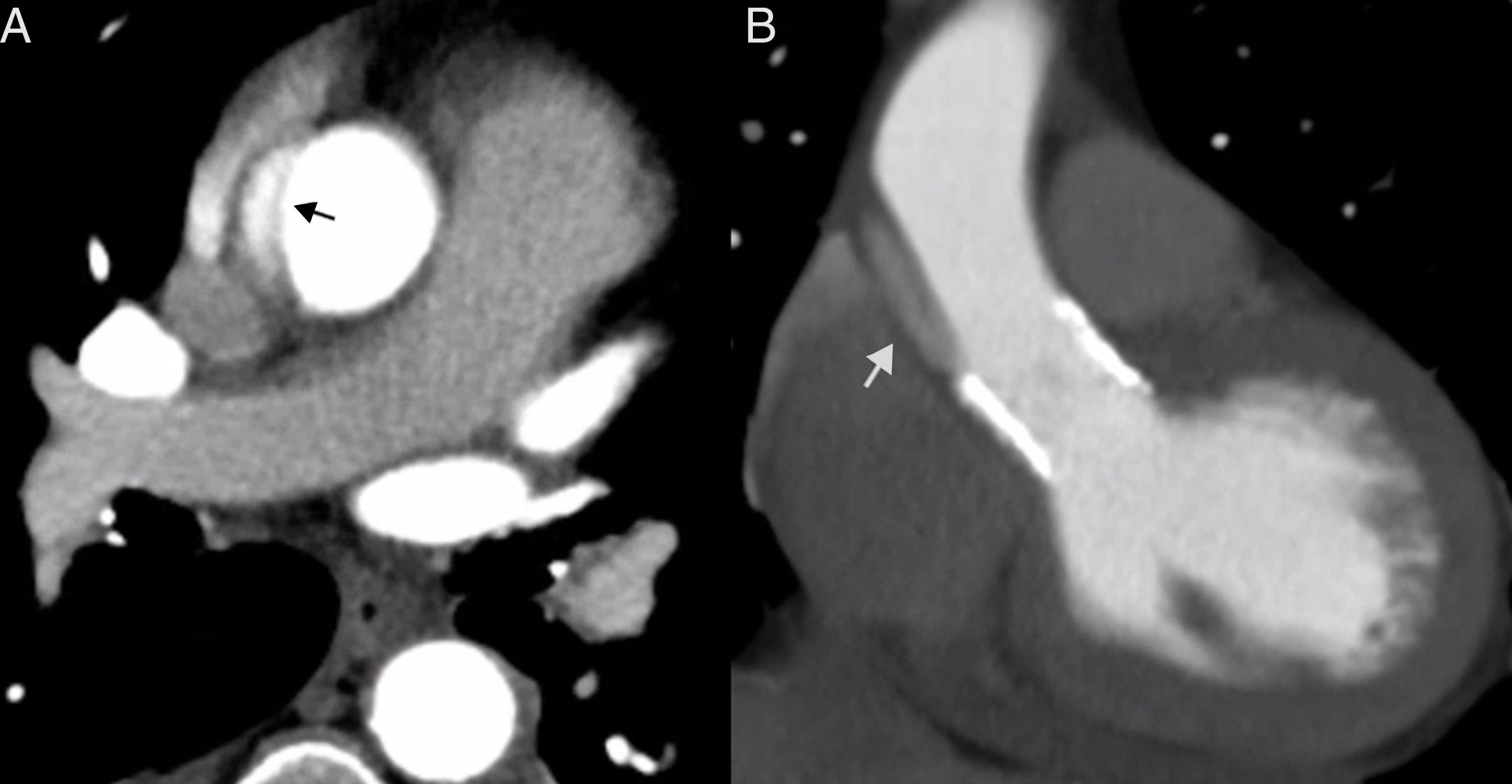
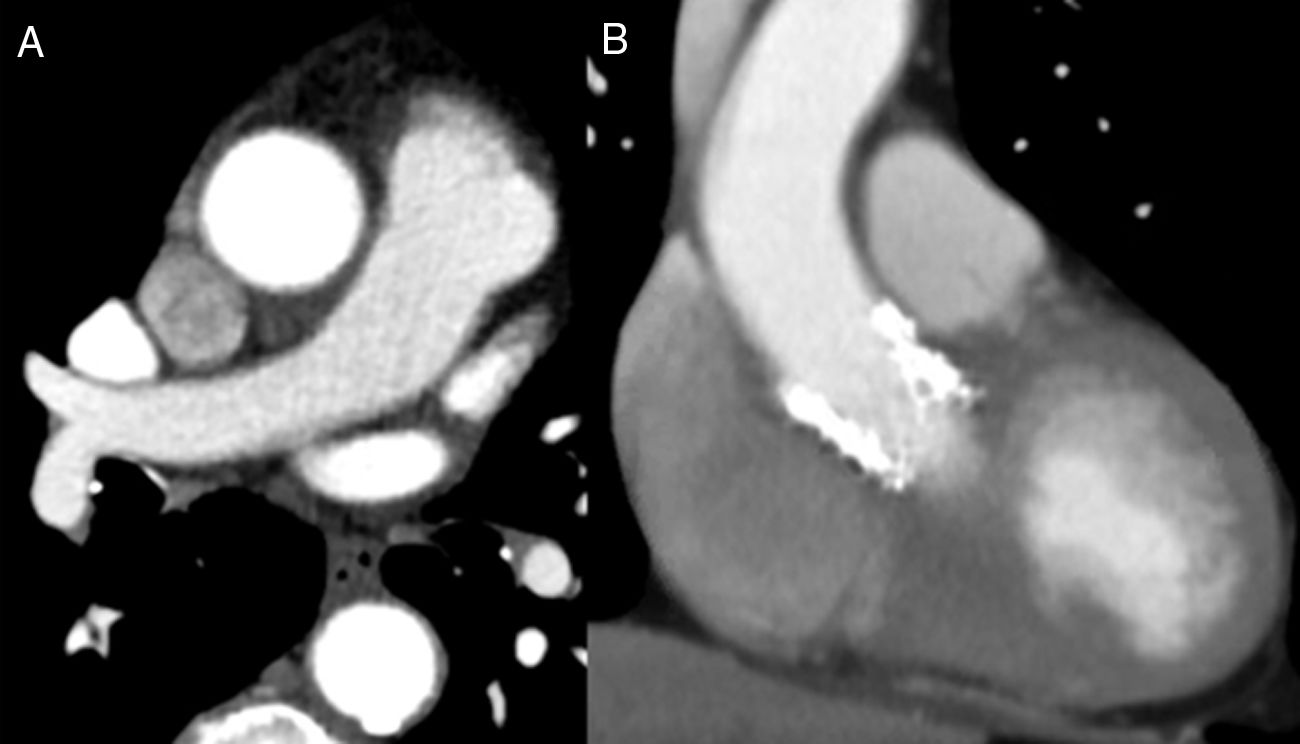
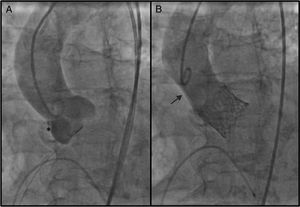
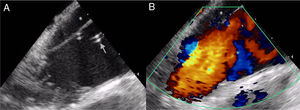
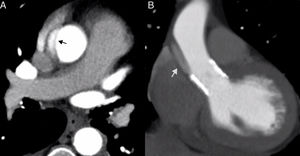
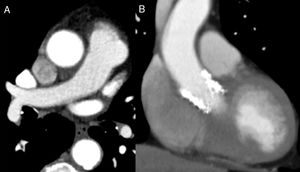
A 90-year-old female with severe symptomatic aortic stenosis was admitted for transcatheter aortic valve implantation (TAVI). A 26-mm Edwards SAPIEN valve was implanted through a transfemoral approach. After the final aortic angiogram a subtraction image was noted from the aortic root just above the right coronary sinus (RCS) to the mid ascending aorta (Figure 1). The intracardiac echocardiogram suggested an aortic dissection, showing an enlarged ascending aorta with an intimal flap without clear flow in the false lumen (Figure 2). The hypothesis of dissection caused by a small tear at the level of the RCS was confirmed by computed tomography (CT) (Figure 3). After heart team discussion it was decided to treat the complication conservatively, since the patient had no symptoms, and she was started on labetalol. A transthoracic echocardiogram was performed that showed good valvular performance without paravalvular leakage. The patient was discharged home after two days. Three months later her exercise capacity had improved and the control CT showed resolution of the dissection (Figure 4).
Contrast thoracic computed tomography images: (A) aortic dissection with the intimal tear dividing the aorta into a true lumen, fully contrasted, and a false lumen, only slightly contrasted (arrow); (B) coronal plane reconstruction similar to the aortography view showing the slightly contrasted false lumen (arrow), corresponding to the subtraction image on aortography (Figure 1B).
We believe this case highlights the importance of proper assessment of angiographic images that can prompt a search for aortic dissection using other diagnostic means.
Iatrogenic acute aortic dissection complicates 0-1.9% of TAVI cases. The best treatment remains controversial, as mortality in patients treated either with surgery (57-80%) or conservatively (58% at 30 days) is very high. Particularly in very elderly patients, a watchful waiting strategy may be reasonable, as in the case presented here.
Conflicts of interestThe authors have no conflicts of interest to declare.