Digital health is broadly defined as the use of information and communication technologies in medicine and plays an increasingly important role in the cardiovascular arena.1 In heart failure (HF), it has been shown to improve care by enhancing patient monitoring, management and therapeutic optimization.2,3
HF is a clinical syndrome with increasing incidence worldwide, affecting at least 1–2% of the overall adult population.4,5 On average, HF patients are hospitalized once a year.6 Due to population growth, aging and the increasing prevalence of comorbidities, the absolute number of hospital admissions for HF is expected to increase by as much as 50% in the next 25 years.7 HF is associated with an increasing cost burden: the annual cost per HF patient in Europe ranges from 5000 to 15000 euros.8
Early detection of worsening HF symptoms and self-care for patients with HF is pivotal and a significant focus of multidisciplinary HF management programs worldwide, yielding better quality of life, lower readmission rates and reduced mortality.4
We used an evidence-based journey with care automation provided by UpHill Health S.A. to remotely monitor and optimize the follow-up of HF patients in an outpatient hospital clinic in Portugal. In this manuscript, we describe the preliminary results of this experience, focusing on short-term outcomes and patient and healthcare workers’ experience with the UpHill program.
Heart failure care journey optimization programThe HF care journey optimization program was implemented in the Heart Center of Hospital da Cruz Vermelha Portuguesa (HCVP), a private hospital in Lisbon, Portugal. This unit specializes in the management of cardiovascular conditions, with dedicated staff and facilities to support a program of cardiovascular health promotion, prevention and early detection of cardiovascular disease, treatment of acute and chronic cardiovascular conditions, and appropriate follow-up and rehabilitation.
The key inclusion criterion was a previous diagnosis of HF with reduced or mildly reduced ejection fraction and at least one on-site cardiology appointment at HCVP in the previous 12 months. The exclusion criteria were no cellphone or internet access and inability to provide a clinical history.
Patients were included after being given a detailed description of the care journey optimization program and providing informed consent. UpHill is General Data Protection Regulation compliant and a certified class I medical device.
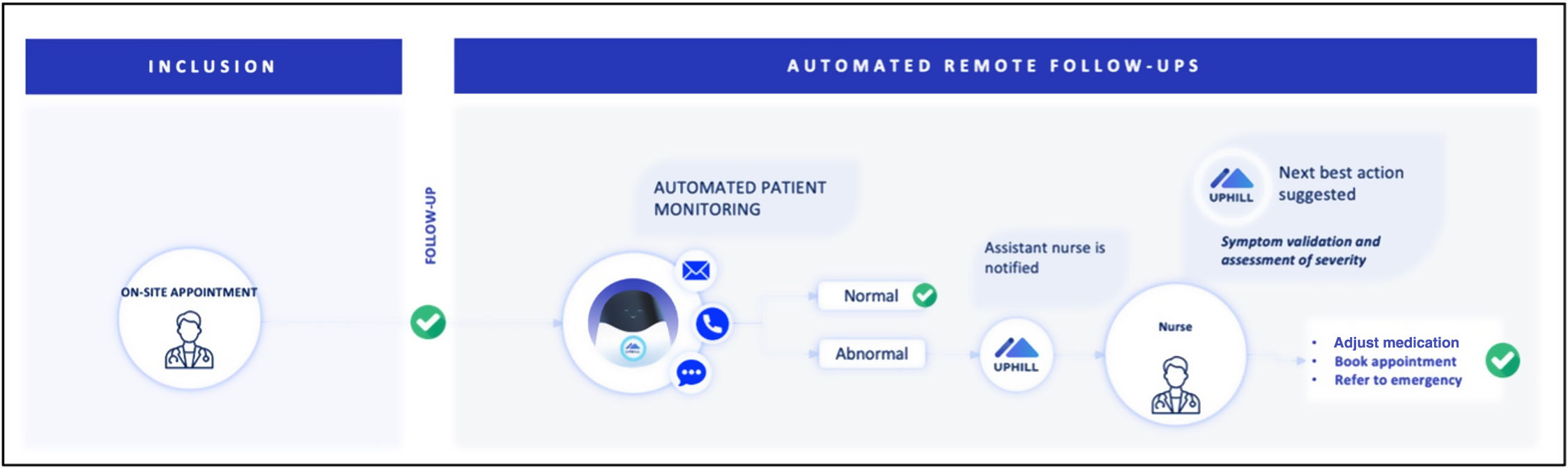
Care journey automation protocolThe implemented care journey aimed to prevent emergency department visits and hospital admission for decompensation by focusing on remote monitoring of HF symptoms and detecting early signs of clinical deterioration.
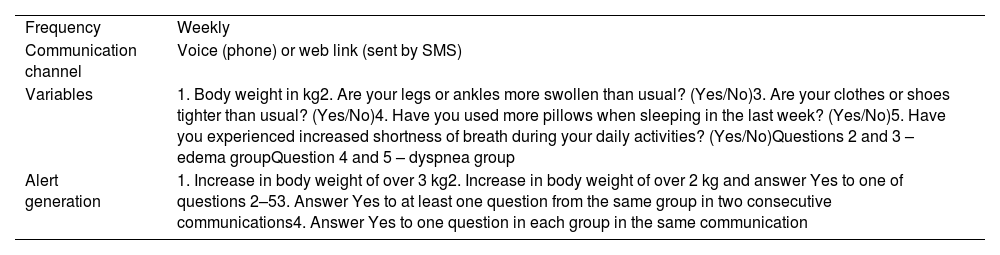
The remote follow-up was performed by a communication assistant, ‘Hilly’, that helped track useful patient parameters, such as weight or red flag HF symptoms (Table 1). The tracking included weekly monitoring for up to six months. Alerts to the healthcare team were triggered according to predefined evidence-based criteria (Table 1).
Automated remote monitoring program protocol.
| Frequency | Weekly |
| Communication channel | Voice (phone) or web link (sent by SMS) |
| Variables | 1. Body weight in kg2. Are your legs or ankles more swollen than usual? (Yes/No)3. Are your clothes or shoes tighter than usual? (Yes/No)4. Have you used more pillows when sleeping in the last week? (Yes/No)5. Have you experienced increased shortness of breath during your daily activities? (Yes/No)Questions 2 and 3 – edema groupQuestion 4 and 5 – dyspnea group |
| Alert generation | 1. Increase in body weight of over 3 kg2. Increase in body weight of over 2 kg and answer Yes to one of questions 2–53. Answer Yes to at least one question from the same group in two consecutive communications4. Answer Yes to one question in each group in the same communication |
When an alert was generated, the healthcare team contacted the patient by phone to validate the clinical alert. If validated, three different actions could be adopted: (1) remote adjustment of diuretic dosing (if the patient was in New York Heart Association [NYHA] functional class I or II); (2) scheduling an in-person appointment for the following days (if in NYHA III); (3) referral to the emergency department (if in NYHA IV). Figure 1 provides a visual overview of the automated remote monitoring program.
During the last two weeks of the protocol, each participant was asked to respond to a satisfaction survey to assess how this care journey program was perceived by HF patients.
ResultsBetween May and October 2022, 51 patients (mean age 74 years; 70% male) were included in the care journey automation protocol.
On average, each patient received 15 automated communications. Most patients (70%) responded to the weekly communication and used the web form rather than the voice phone channel to answer the questionnaire.
The weekly automatic communications generated 69 alerts. After phone contact by the nursing team aiming to assess the specific triggers of the alert and validate or reject it, the overall sensitivity and specificity of the remote monitoring weekly communication were 66% and 62%, respectively.
Of the 22 patients who answered the satisfaction survey, 95% characterized the care program as safe and felt closer to the healthcare team. All patients would recommend it to a friend or relative. In addition, unstructured interviews with healthcare professionals participating in the program demonstrated a general feeling of satisfaction and added value to the standard of care.
DiscussionOverall, implementing this care journey automation program targeting HF patients positively impacted patients, healthcare professionals and the institution.
From the patients’ standpoint, this care journey optimization program fostered confidence and security through regular remote monitoring by the healthcare team. In addition, it provided the patient with awareness and empowerment for managing HF through tracking weight and relevant symptoms. Patients with HF and more effective self-care have a better quality of life and lower mortality and readmission rates than those with lower levels of self-care.4 Overall, this optimization program aimed at prevention and early detection of HF decompensation. As previously demonstrated, telemedicine strategies appear to be associated with reduced short-term cardiovascular-related hospitalization and mortality risk in patients with HF.9,10
Discussing the impact on healthcare professionals and the organization of clinical teams is also interesting. The automation of repetitive monitoring tasks for patients with chronic HF was seen positively, with continuous monitoring of stable patients (while generating alerts for weight increase or congestive symptoms). Healthcare professionals involved in the program, including a strong contingent of the nursing team directly involved in patient contact, perceived greater efficiency of daily routines through automatic prioritization of patients who should be contacted first. Interestingly, when we compared the estimated amount of time that would be spent by healthcare staff for weekly follow-up by phone of every HF patient with performing only the alert-triggered follow-ups using the care journey automation program, we estimated that the inclusion of this evidence-based journey with care automation could safely save 60 hours of clinical workload.
Finally, healthcare institutions might benefit from care journey optimization programs like the one described herein. This type of program can provide a thorough mapping of the care journey of HF patients, improving the allocation of resources to actual needs and, in this way, delivering value-based healthcare by improving health outcomes and minimizing costs.
To sum up, this pilot project with an automated monitoring protocol targeting the care journey of outpatient HF patients was able to streamline medical contact and optimize human resources (potentially reducing costs for institutions and society) while delivering a safe digital health solution that elicited a strong positive feeling in patients and healthcare staff.
Conflicts of interestThe authors have no conflicts of interest to declare.