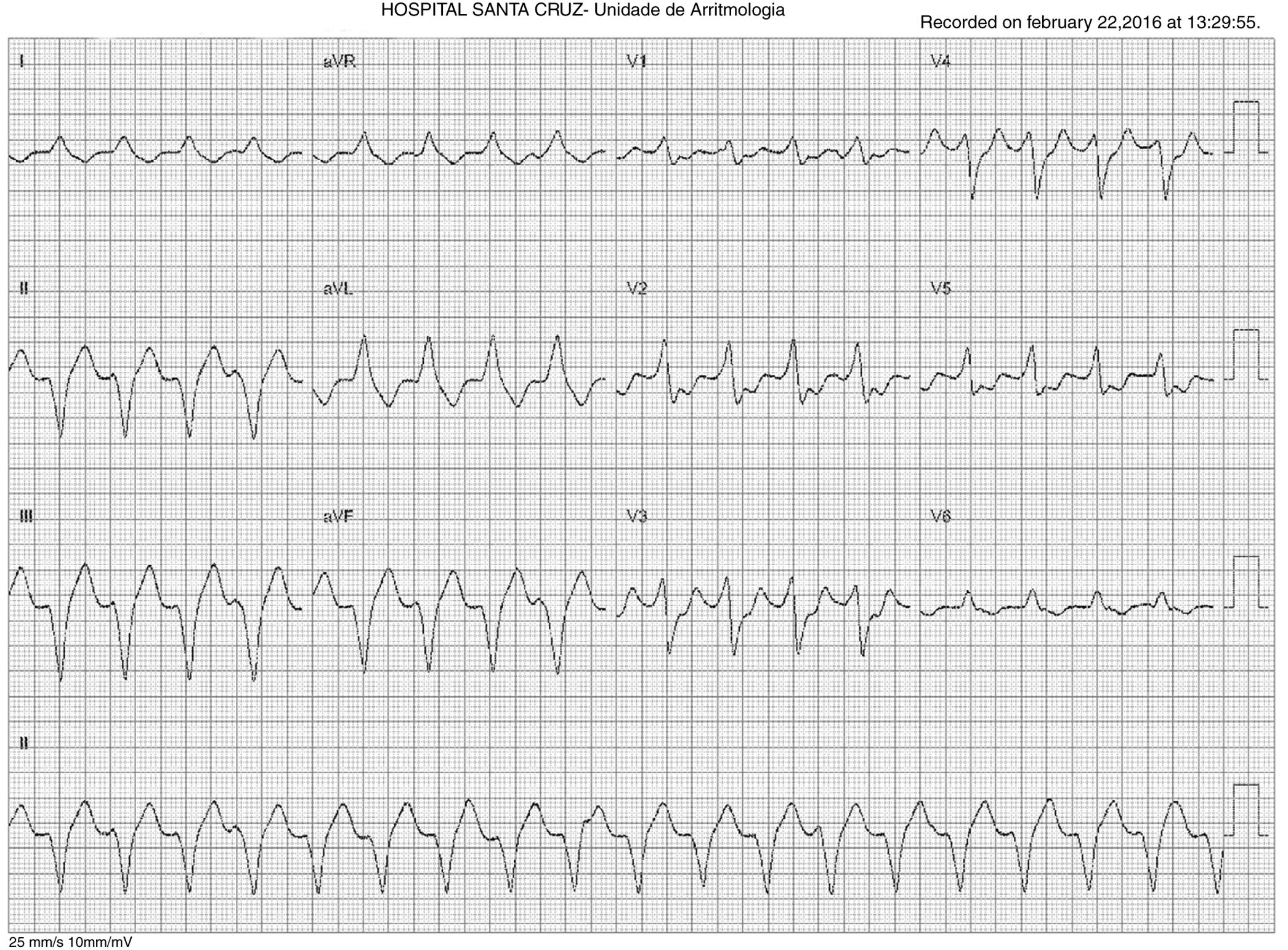
We report the case of a 44-year-old woman who was referred for ablation of recurrent ventricular tachycardia (VT) in the setting of dilated cardiomyopathy secondary to myocarditis. The ECG displayed a right bundle branch block morphology and superior axis in the frontal plane, associated with a pseudo delta wave in the precordial leads that suggested an epicardial origin.
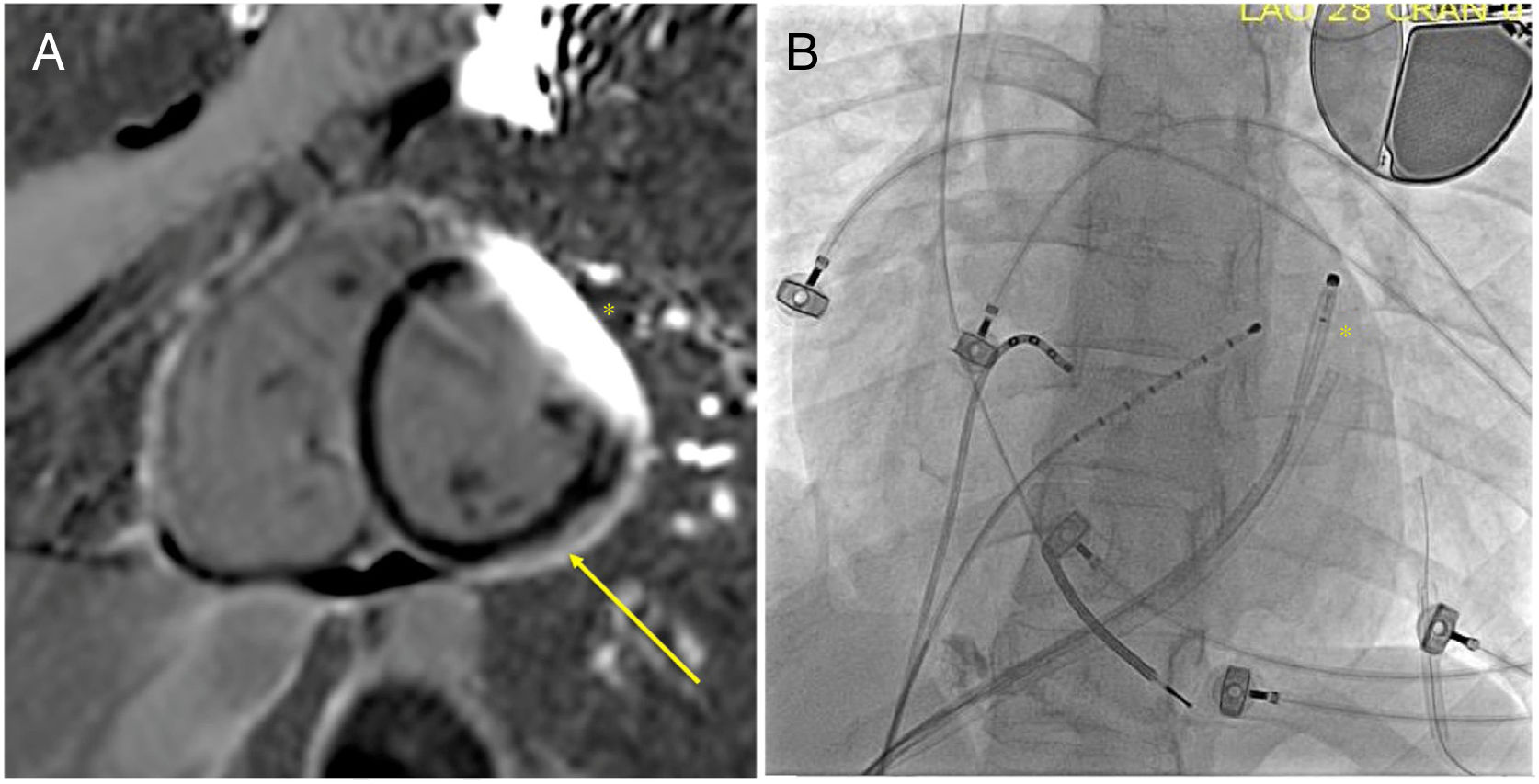
Cardiac magnetic resonance performed prior to the procedure showed late gadolinium enhancement at the lateral wall of the left ventricle (LV) and excluded subendocardial fibrosis in either ventricle. This information was crucial and influenced the ablation strategy, identifying the target area as exclusively epicardial, thus avoiding unnecessary mapping of the endocardial surface of the LV.
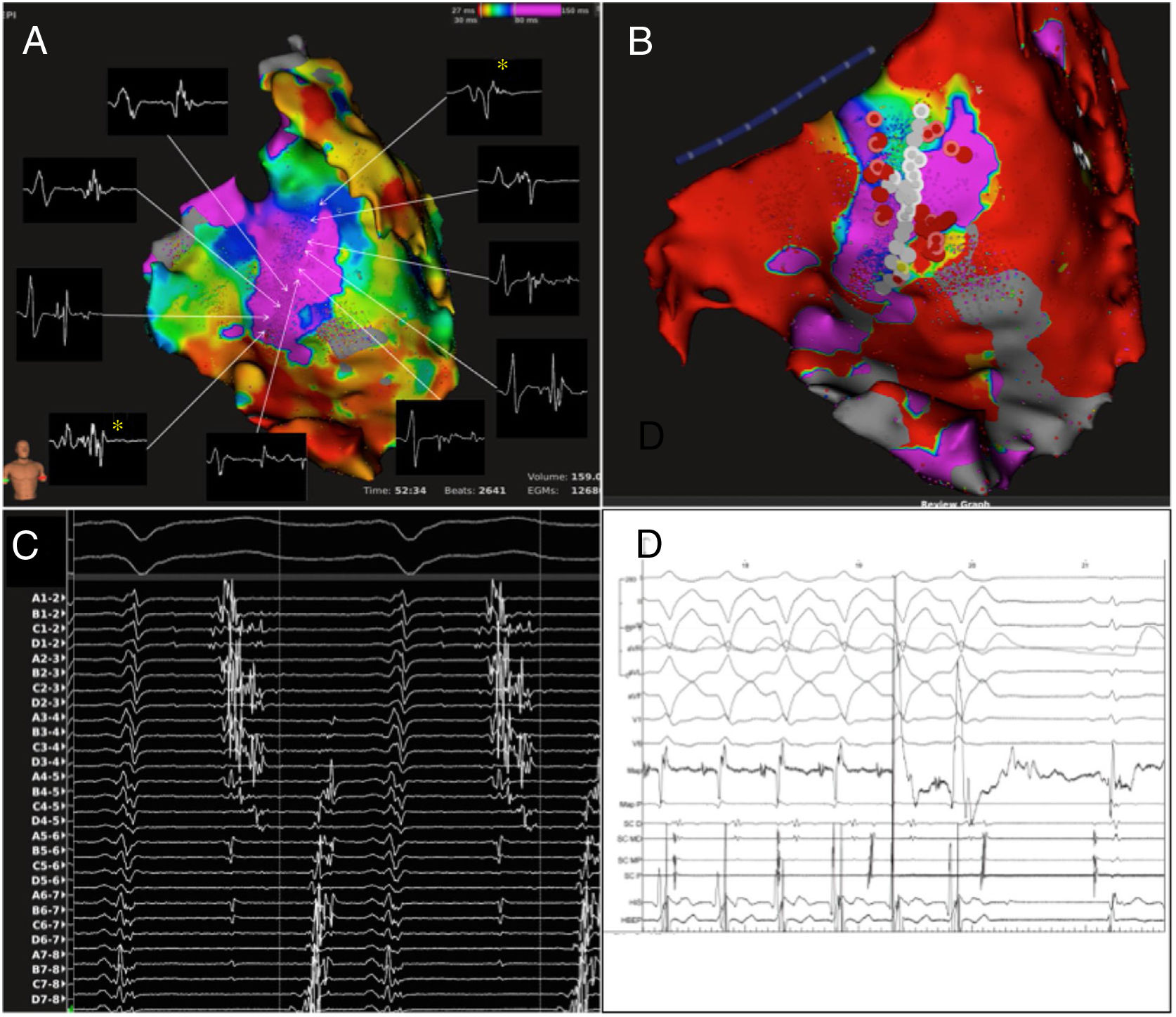
Epicardial activation mapping and ablation during VT were performed using the Orion® high-density catheter (Boston Scientific Inc.) and the Rhythmia® mapping system (Boston Scientific Inc.). Applications near the exit site immediately terminated the tachycardia, which was no longer inducible.
One year after the procedure the patient was still in sinus rhythm with no episodes of VT or non-sustained VT recorded by continuous monitoring via an implanted cardioverter-defibrillator.
Reportamos o caso de uma doente referenciada para ablação de taquicardia ventricular (TV) recorrente em contexto de miocardiopatia dilatada, secundária a miocardite. O ECG apresentava bloqueio de ramo direito e eixo superior no plano frontal, associado a uma pseudo onda delta nas derivações precordiais, sugerindo origem epicárdica.
Previamente ao estudo eletrofisiológico, foi realizada ressonância magnética que revelou realce tardio (gadolínio) da parede lateral do ventrículo esquerdo (VE), permitindo também excluir fibrose subendocárdica em ambos os ventrículos. Esta informação foi crucial na decisão da melhor estratégia terapêutica, identificando a área alvo da ablação como exclusivamente epicárdica, evitando o mapeamento desnecessário da superfície endocárdica do VE.
O mapa de ativação epicárdica e ablação em TV foram realizados utilizando o cateter de alta densidade Orion® (Boston Scientific® Inc) e o sistema de mapeamento Rhythmia® (Boston Scientific® Inc). Aplicações de energia de radiofrequência junto ao local de saída terminaram a taquicardia, que sob estimulação ventricular programada não voltou a ser induzida.
Um ano após o procedimento, a doente mantém-se em ritmo sinusal, sem novos episódios de taquicardia ventricular mantida ou não (monitorização contínua através do cardioversor desfibrilhador implantado).
Data on mapping of epicardial ventricular tachycardia (VT) using rapid high-resolution catheters are scarce.1 We report a case of epicardial activation mapping and ablation during VT using the Orion® high-density catheter (Boston Scientific Inc.) and the Rhythmia® mapping system (Boston Scientific Inc.) and subsequent one-year follow-up results.
Case reportA 44-year-old woman with a history of dilated cardiomyopathy secondary to myocarditis was referred for ablation due to recurrent VT.
The patient first reported fatigue and palpitations in 1998, when an initial transthoracic echocardiogram showed a mildly dilated left ventricle (LV) with borderline ejection fraction (EF) of 50%. Medical therapy was begun with angiotensin-converting enzyme inhibitors and beta-blockers. Over the years, Holter recordings showed increasingly frequent single premature ventricular contractions, and a slow but steady reduction in EF (45% in 2014) was noted on serial echocardiographic assessments.
In 2014 the patient was admitted due to VT (cycle length 330 ms) with right bundle branch block (RBBB) morphology and superior axis in the frontal plane. A pseudo delta wave was noted in the precordial leads, suggesting an epicardial origin. The patient received a single-chamber implantable cardioverter-defibrillator (ICD) and was started on oral amiodarone.
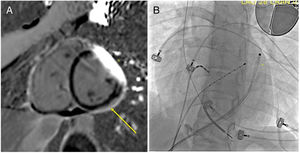
In February 2016, she was admitted following multiple appropriate shocks due to VT, which presented the same morphology and cycle length as before (Figure 1). Cardiac magnetic resonance (CMR) was performed, which showed late gadolinium enhancement at the lateral wall of the LV (Figure 2A). There was no evidence of subendocardial fibrosis in either ventricle. Epicardial VT ablation was planned with the Rhythmia mapping system.
(A) Cardiac magnetic resonance with late gadolinium enhancement of the epicardial surface of the left ventricular lateral wall (arrow: fibrotic tissue); * denotes a visual artifact caused by the cardioverter-defibrillator lead; (B) chest X-ray during the ablation procedure; * indicates the closed Orion catheter in the pericardial space.
The system has been described elsewhere.2 Briefly, it consists of a bidirectional deflectable mapping catheter with an 8F shaft and a mini-basket array of 64 electrodes on eight splines (IntellaMap Orion®, Boston Scientific, Natick, MA). The location of each of the 64 basket electrodes is identified by a combination of a magnetic sensor in the distal region of the catheter and impedance sensing on each electrode. The system includes an electronic patient interface unit and a computer workstation. Individual cardiac beats are acquired automatically. The electrograms are automatically collected and recorded, enabling the map to be created in real time by continuous movement of the catheter with minimal manual annotation. The surface geometry of the chamber is continuously generated by the outermost electrode locations associated with accepted beats. Activation and voltage maps can be constructed quickly with high resolution, due to the automatic nature of annotation.
Epicardial ventricular tachycardia ablation procedureThe patient presented to the electrophysiology laboratory in sinus rhythm (SR). Percutaneous pericardial access was obtained using a Tuohoy needle as previously described.3
The Rhythmia mapping system and Orion catheter were used to rapidly obtain a high-density voltage map of the epicardial surface of the LV during SR. Due to the risk of cardiac trauma it was decided to use the catheter without fully deploying the basket (Figure 2B). Guided by the CMR data, the lateral wall of the LV was targeted and a wide area with low amplitude and delayed signals (consistent with scar) was recorded. The system was able to identify activation from these areas in the upper and lower segments of the scar tissue, which then collided inside it (during SR).
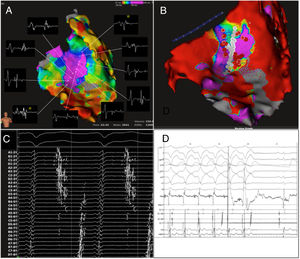
Monomorphic VT with RBBB and superior axis in the frontal plane was reproducibly induced with S1=500 ms and a single premature ventricular contraction from the right ventricle. Entrainment mapping was not feasible due to inconsistent capture within the scar. Activation mapping obtained with the Orion catheter in this area documented a typical figure-of-eight tachycardia with an isthmus (already suggested in SR) and two outer loops (Supplementary Video 1). The electrograms obtained with the mapping catheter inside the scar area showed potentials that spanned more than 50% of the electrical diastole (Figure 3).
(A) Mapping of late potentials during sinus rhythm; a wide area of late potentials can be seen on the left ventricular lateral wall, delineating a channel. The two asterisks (*) identify points where the distance of the R wave to the late potential is shorter (likely entry sites to the channel); (B) white dots correspond to the potential channel and red dots to the radiofrequency (RF) application areas, respectively; (C) electrograms recorded in ventricular tachycardia (VT) with the Orion catheter in the late potential area; activation covers most of diastole and spans more than 75% of the VT cycle length; (D) termination of VT during RF application.
The catheter was then changed to an irrigated-tip ablation catheter. A coronary angiogram of the left coronary artery was obtained. Prior to each application, high-output pacing was used to ensure that there was no phrenic nerve capture. Application of radiofrequency energy to the distal part of the isthmus near the exit site immediately terminated the tachycardia. Further applications were delivered in the previously tagged areas of late potentials. At the end of the procedure, VT was no longer inducible.
One year later, the patient was still in SR, with no recorded episode of VT or non-sustained VT (either clinical or documented by the ICD) and with significant improvement in her quality of life.
DiscussionTo the best of our knowledge this is the first long-term assessment of VT ablation outcomes using the Rhythmia mapping system on the epicardium. The Rhythmia mapping system and Orion catheter rapidly produce accurate high-density maps of areas of interest (2641 [SR] and 1885 [VT] points were recorded in the initial 15 minutes of mapping, respectively), which is of crucial importance in VT ablation procedures. The catheter was used in its closed state, in order to avoid injuring the heart.
Performing CMR prior to the ablation enabled us to identify the target area as exclusively epicardial, thus avoiding unnecessary mapping of the endocardial surface of the LV.
ConclusionThe Rhythmia mapping system is a promising tool for epicardial ablation of ventricular tachycardia.
Supplementary video 1Activation map during ventricular tachycardia, showing a figure-of-eight activation involving the potential channel area.
Conflicts of interestThe authors have no conflicts of interest to declare.