Left ventricular thrombus commonly occurs as a complication of acute anterior myocardial infarction and nonischemic cardiomyopathies with severe left ventricular systolic dysfunction. Its frequency is still high despite medical advances. Current guidelines recommend the use of vitamin k antagonists as first-line therapy, however, the off-label use of direct oral anticoagulants is becoming more frequent and attractive, given the better pharmacological and clinical profile, with the improvement of the patient's quality of life.
AimTo provide an update on the currently existing evidence regarding the outcomes of efficacy and safety of direct oral anticoagulants (DOACs) as first-line therapy in left ventricular thrombus, in comparison to vitamin K antagonists (VKAs).
MethodsA systematic review and meta-analysis of studies on the effects of direct oral anticoagulants versus vitamin K antagonists on left ventricular thrombi and on the results was performed.
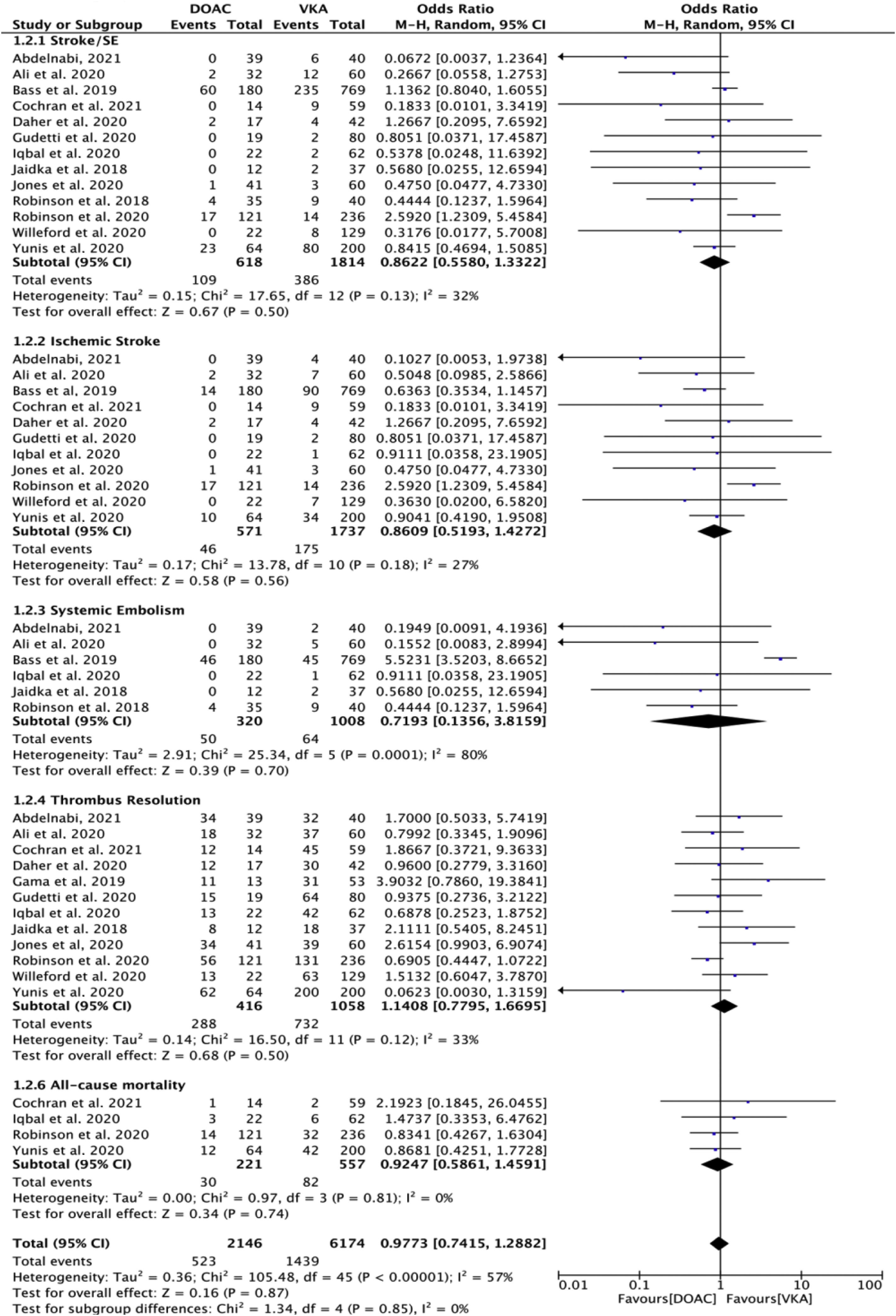
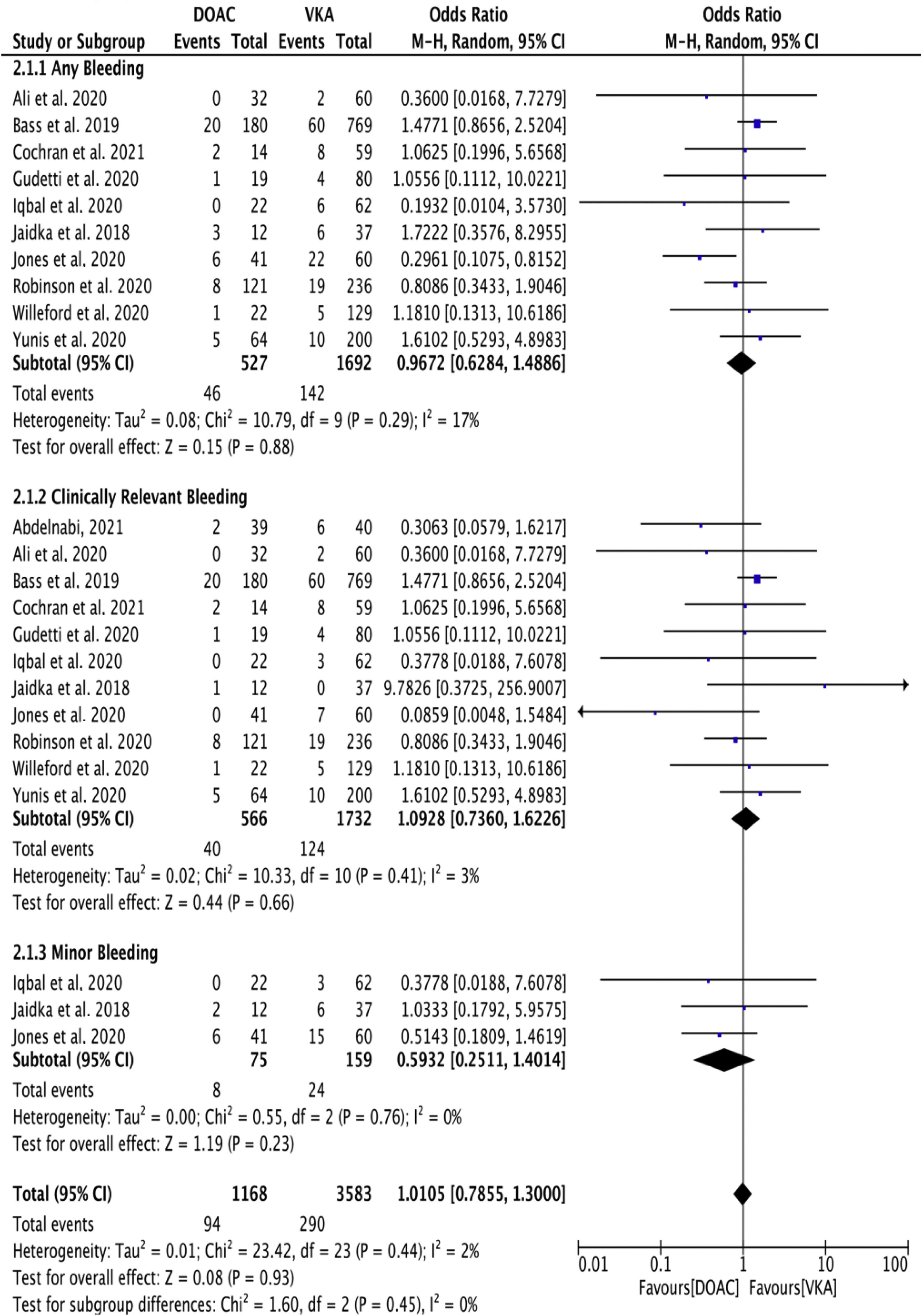
ResultsFourteen studies were included in the meta-analysis, with a total of 2498 patients (n=631 direct oral anticoagulants and n=1867 for VKAs). No significant differences were found in efficacy and safety outcomes (odds ratio (OR) 0.86; 95% confidence interval (CI), 0.55–1.33; p=0.50; I2=32%) and (OR 1.0; 95% CI, 0.78–1.30; p=0.93; I2=2%) respectively. No difference was noted in all-cause mortality (OR 0.92; 95% CI, 0.58–1.45; p=0.74; I2=0%). Thrombus resolution was observed in 288/416 in direct oral anticoagulants vs. 732/1085 patients treated with VKAs (OR 1.14; 95% CI, 0.77–1.66; p=0.50; I2=33%).
ConclusionsThe findings of this meta-analysis suggest the potential utility of DOACs as a first-line strategy in patients with left ventricular thrombus.
Trombos no ventrículo esquerdo ocorrem geralmente como complicação do enfarte agudo do miocárdio anterior e de cardiomiopatias não isquémicas com disfunção sistólica ventricular esquerda grave. A sua frequência ainda é alta, apesar dos avanços médicos. As orientações atuais recomendam o uso de antagonistas da vitamina K como tratamento de primeira linha. No entanto, a utilização de anticoagulantes orais diretos está a tornar-se mais frequente, dado o melhor perfil farmacológico e clínico, com melhoria da qualidade de vida do doente.
ObjetivoAtualizar a evidência existente relativamente à eficácia e segurança dos anticoagulantes orais diretos como tratamento de primeira linha no TVE, em comparação com os antagonistas da vitamina K.
MétodosFoi realizada uma revisão sistemática e uma meta-análise de estudos sobre os efeitos dos anticoagulantes orais diretos versus os antagonistas da vitamina K nos trombos ventriculares esquerdos e sobre os resultados.
ResultadosNa presente revisão sistemática e metanálise foram incluídos 14 estudos, com 2498 doentes (n=631 tratados com anticoagulantes orais diretos e n=1867 com antagonistas da vitamina K). Não se registaram diferenças significativas nos resultados de eficácia e segurança (OR 0,86; 95% CI, 0,55-1,33; p=0,50; I2=32%) e (OR 1,0; 95% CI, 0,78-1,30; p=0,93; I2=2%) respetivamente. Não se verificou qualquer diferença na mortalidade por todas as causas (OR 0,92; 95% CI, 0,58-1,45; p=0,74; I2=0%). A resolução do trombo foi observada em 288/416 no grupo dos doentes tratados com anticoagulantes orais diretos versus 732/1085 no grupo dos doentes tratados com antagonistas da vitamina K (OR 1,14; 95% CI, 0,77-1,66; p=0,50; I2=33%).
ConclusãoOs resultados desta metanálise sugerem a utilidade dos anticoagulantes orais diretos como estratégia de primeira linha em doentes com trombo do ventrículo esquerdo.
Left ventricular thrombus (LVT) commonly occurs as a complication of acute anterior myocardial infarction (MI) and dilated cardiomyopathy (DCM) with severe left ventricular (LV) systolic dysfunction.1 Less commonly, it is present in midcavity phenotype hypertrophic cardiomyopathy.2
Despite advances in the management of acute MI, with prompt percutaneous intervention (PCI), the incidence reported is still high. Some studies report incidence between 15 and 35% in patients with acute MI, and about 10–30% in non-ischemic DCM.3,4 However, the real incidence of LVT is highly dependent on the imaging technique used to establish the diagnosis.5,6
Patients with LVT are at higher risk of cardioembolic stroke (odds ratio 5.5, 95% CI 3.0–9.8), with most events occurring within the first four months post-MI.7,8 Anticoagulation is indicated for stroke prevention, however, its benefits must be weighed against bleeding risk, especially in patients who are on single or dual antiplatelet therapy.
In patients with no specific indication for vitamin K antagonists (VKAs) (e.g., mechanical heart valve), direct oral anticoagulants (DOAC) may be an option. However, there are no large prospective or head-to-head comparison data for DOACs vs. VKAs, which assess efficacy and safety.
Therefore, we performed a meta-analysis of observational studies comparing the effectiveness and safety of DOACs vs. VKAs.
MethodsOverviewWe conducted a systematic review and meta-analysis of studies on the effects of DOACs on LVT and outcomes in comparison with VKAs. The review was registered with PROSPERO (CRD42021248170) and reported according to PRISMA guidelines.
Search strategy, selection criteria, and data extractionWe electronically searched the PUBMED databases with no starting date through March 31, 2021. The search included MeSH terms [‘oral anticoagulation’ and ‘ventricular thrombus’] according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement, PRISMA. No language restrictions were applied.
Abstracts and potentially relevant full texts were reviewed independently by three authors (HM, HF, and JA) with any conflicts resolved by consensus. Case-control studies, cohort studies, and brief reports were eligible for inclusion. Case reports, studies without comparison groups, narrative or systematic literature reviews, preprint papers, and studies reporting on overlapping populations were excluded. The following data were extracted: author's name, publication date, study design, study population, follow-up period.
Outcomes of interest included efficacy outcomes (ischemic stroke, systemic embolism, thrombus resolution, all-cause mortality) and safety outcomes (any bleeding, clinically relevant bleeding, and minor bleeding). We planned to record any additional patients’ outcomes which were identified. Where papers described service configuration or resource-use changes without clinical outcomes, we excluded them from the analysis.
Quality appraisalThe quality appraisal was established according to Le Floch et al. criteria, by two independent assessors (HF and JA).9 This tool appraises the quality of the study based on the following questions: Did this article give an answer to the research question? Did the article focus clearly on the research question? Was the methodology appropriate? Do you believe the results? (Can it be due to chance, bias, or confounding?). To be included, the article had to score “yes” on every question.
Statistical analysisQuantitative meta-analysis was performed for an outcome when more than one study presented relevant data. We excluded individual outcomes from studies reporting no adverse outcomes in one or both groups, and studies not satisfying the normality assumption for continuous variables.
A random-effects estimate of the pooled odds of each outcome was generated with the use of the Mantel-Haenszel method. Between-study heterogeneity was explored using the I2 statistic, with substantial heterogeneity defined as an I2 value greater than 50%. We reported p values and the amount of accounted heterogeneity for each covariate. Potential publication bias was assessed with Egger's test and funnel plots for visual inspection when sufficient studies (n>10) were available. Statistical analyses were performed using the Revman software package (Review Manager, Version 5.4. Copenhagen, The Nordic Cochrane Center, the Cochrane Collaboration).
ResultsStudy selectionThe literature retrieval process from this meta-analysis is presented in Figure 1. A total of 368 papers were initially identified, of which 279 records nonrelated to the theme were excluded. After review of the 38 remaining studies, 24 were excluded with reasons: systematic reviews and meta-analysis (n 9); case reports and case series (n 7); five review articles (n 5); two single-arm studies (2); one trial design (1). Finally, a total of 14 studies that were published between 2018 and 2021 involving 2498 patients with left ventricular thrombus (n=631 for DOACs and n=1867 for VKAs) were included in this meta-analysis.10–23 Of the 14 studies, only one was prospective (23); and nine retrospective, observational cohort studies with the full text.10–13,15,16,18,20,21 The other four studies were published as a conference abstract.14,17,19,22
Study population characteristicsThe baseline characteristics of the included studies are shown in Table 1. Overall, there was a predominance of males, constituting 74–90% of cases. The patients’ mean age ranged from 56 to 63±11. The most common cause for LVT was ischemic cardiomyopathy and the main comorbidities were hypertension and diabetes mellitus, followed by dyslipidemia. History of smoking was reported from 15 to 59% of cases. The average follow-up period ranged from 3 to 36 months. Nine studies described the type of DOACs, totaling 407 of the 631 patients. Apixaban was used in 170 (41.7%) patients and rivaroxaban in 200 (49.1%) patients. Dabigatran and edoxaban were used in 35 (8.5%) and 2 (0.4%) patients, respectively. Triple therapy was reported in five studies, 214 patients (8.5% of the total population).
Study and patients baseline characteristics.
| Jaidka et al., 2018 | Robinson et al., 2018 | Bass et al., 2019 | Gama et al., 2019 | Iqbal et al., 2020 | Robinson et al., 2020 | Daher et al., 2020 | Gudetti et al., 2020 | Jones et al., 2020 | Yunis et al., 2020 | Willeford et al., 2020 | Ali et al., 2020 | Cochran et al., 2021 | Abdelnabi et al., 2021 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients, n | 49 | 75 | 949 | 66 | 84 | 357 | 59 | 99 | 101 | 264 | 151 | 92 | 73 | 79 |
| VKAs | 37 | 40 | 769 | 53 | 62 | 236 | 42 | 80 | 60 | 200 | 129 | 60 | 59 | 40 |
| DOACs | 12 | 35 | 180 | 13 | 22 | 121 | 17 | 19 | 41 | 64 | 22 | 32 | 14 | 39 |
| Apixaban | NR | 26 | 77 | NR | 8 | NR | 12 | 15 | 15 | NR | 4 | 13 | NR | NR |
| Dabigatran | NR | 2 | 28 | NR | 1 | NR | 1 | 2 | 0 | NR | 0 | 1 | NR | NR |
| Edoxaban | NR | 0 | 0 | NR | 0 | NR | 0 | 0 | 2 | NR | 0 | 0 | NR | NR |
| Rivaroxaban | NR | 7 | 75 | NR | 13 | NR | 4 | 2 | 24 | NR | 18 | 18 | NR | 39 |
| Age (mean±SD) | 59±11 | NR | 64* | 63±11 | 62±14 | 58±15 | 59±14 | 61±12 | 59±14 | NR | 56* | NR | NR | 49±12 |
| Male | 75% | NR | 70% | 77% | 90% | 74.5% | 82.6% | 74% | 82.5% | NR | 80.1% | 81.5% | 76.7% | 57% |
| Clinical characteristics | ||||||||||||||
| Hypertension | 20 (40.8%) | NR | NR | NR | 27 (32%) | 263 (73.6%) | 27 (45.7%) | 76 (78%) | 45 (44%) | NR | 62 (41.1%) | NR | NR | 41 (53.1%) |
| Diabetes mellitus | 8 (16.3) | NR | NR | NR | 22 (26%) | 124 (35%) | 11 (18.6%) | 37 (38%) | 17 (17%) | NR | 41 (27.2%) | 30 (33%) | 30 (41%) | 41 (53.1%) |
| Smoker | 19 (38.8%) | NR | NR | NR | 38 (49%) | NR | 35 (59.3%) | NR | 28 (28%) | NR | NR | 14 (15%) | NR | NR |
| Hyperlipidemia | 15 (30.4%) | NR | NR | NR | 13 (15%) | 197 (55%) | NR | NR | 38 (38%) | NR | NR | NR | NR | NR |
| ICM | 49 (100%) | NR | NR | NR | 73 (87%) | 214 (60%) | 51 (87%) | 58 (59%) | 101 (100%) | NR | 39 (25.8)¥ | NR | 42 (59%) | 61 (78.5%) |
| Triple therapy | 42 (87%) | NR | NR | NR | 32 (38%) | NR | NR | NR | 70 (69%) | NR | 29 (19.2%) | NR | NR | 41 (53.1%) |
| Treatment | ||||||||||||||
| Follow-up period (months) | 6 | 12 | 3 | 12 | 36 | 12 | 3 | 12 | 26 | 24 | 8.3 | 12 | 12 | 6 |
| Duration of anticoagulation | NR | NR | NR | NR | 667±568 | NR | NR | NR | 3 months | NR | NR | NR | NR | NR |
ACO: anticoagulation; DOACs: direct oral anticoagulants; ICM: ischemic cardiomyopathy; N.: No; NR: not referred; SD: standard deviation; SE: systemic embolism; VKAs: vitamin K antagonists.
The outcomes analyzed were efficacy and safety of oral anticoagulation (DOACs vs. VAKs) in the treatment of left ventricular thrombus LVT. Thirteen studies involved the outcome of stroke and/or systemic embolism10–13,15–23; twelve studies mentioned the thrombus resolution,10,12–18,20–23 but only four studies involved the outcome of all-cause mortality.12,16,20,22 Eleven studies reported bleeding events.10–12,15–18,20–23
Effect of NOACs versus that of VKAs and, on stroke or systemic embolism A total of 13 included studies reported the stroke or systemic embolism event rate.10–13,15–23 As shown in (Figure 1), fewer thromboembolic (stroke or systemic embolism) events were reposted in the DOACs-treated patients compared with those receiving VKA (109/618 vs. 386/1814 patients (OR 0.86; 95% CI, 0.55–1.33; p=0.50; I2=32%)), however, it was statistically non-significant. For ischemic stroke, there were no significant differences among the groups, (46/571) DOACs vs. (175/1737) VKA patients (OR 0.86; 95% CI, 0.51–1.42; p=0.56; I2=27%). Systemic embolism rate was (50/320) DOACs vs. (64/1008) VKA patients (OR 0.71; 95% CI, 0.13–3.58; p=0.70; I2=80%).
A total of 12 included studies (n=1474) reported the rate of thrombus resolution.10,12–18,20–23 A total of 1474 patients had imaging follow-up. The vast majority of studies relied on transthoracic echocardiogram (TTE) to evaluate left ventricular thrombus (LVT) resolution. Jones et al. used TTE or cardiac magnetic resonance (CMR),18 and Iqbal et al. used CMR to diagnose LVT at the baseline with subsequent assessments made by TTE.16 LVT resolution was observed in 288/416 in DOACs vs. 732/1085 patients treated with VKA (OR 1.14; 95% CI, 0.77–1.66; p=0.50; I2=33%) (Figure 1).
All-cause mortality was reported by only four studies.12,16,20,22 No significant differences were noted among the groups; all-cause mortality occurred in 30/221 DOAC vs. 82/557 VKA patients (OR 0.92; 95% CI, 0.58–1.45; p=0.74; I2=0%) (Figure 1). Overall, there were no significant differences regarding the efficacy outcomes (OR 0.97; 95% CI, 0.74–1.28; p=0.87; I2=57%) (test for subgroup differences: Chi2=1.34, df=4 (p=0.85), I2=0%).
Eleven of the included studies assessed the effect of DOACs versus that of VKAs on bleeding events using varying criteria to identify and record bleeding incidents.10–12,15–18,20–23 In the study by Guddeti et al., bleeding events were defined as any life-threatening bleeding, drop in hemoglobin ≥2 g, and/or bleeding requiring hospitalization or evaluation by endoscopy.15 Bass et al., defined bleeding events using the Global Use of Strategies to Open Occluded Arteries (GUSTO) criteria, and blood product administration.11 In turn, Iqbal et al. used clinically relevant bleeding and observed three episodes of gastrointestinal bleeding and three epistaxis events none requiring hospitalization or blood transfusion.16 Jones et al. defined bleeding events using the Bleeding Academic Research Consortium (BARC) criteria, and they presented the data of minor bleeding events (BARC 1) and major bleeding events (BARC ≥2).18 Robinson et al. reported bleeding events requiring cessation in anticoagulation;20 Jaidika et al. classified bleeding as minor and major;17 Cochran et al. included minimal, minor, and major bleeding assessed by Thrombolysis in Myocardial Infarction bleeding criteria,12 while no criteria were specified by Ali et al., Willeford et al., and Yunis et al.10,21,22
Any bleeding events were observed in 8.7% of DOACs (46/527) and 8.3% of VKA patients (142/1692) (OR 0.96, 95% CI 0.62–1.48, p=0.88; I2=17%). Clinically relevant bleeding events were reported by 11 of the 14 studies and were observed in 7.01% of DOACs (40/566) and 7.15% of VKA patients (124/1732) (OR 1.09, 95% CI 0.73–1.62, p=0.66; I2=3%). Data for minor bleeding were available in three of 14 studies. Minor bleeding events were reported at a pooled rate of 11% (8/75) in DOAC-treated patients compared with 15% in VKA-treated patients (24/159) (OR 0.59, 95% CI 0.25–1.40, p=0.23; I2=0%). Overall, there were no significant differences regarding the safety outcomes (OR 1.0; 95% CI, 0.78–1.30; p=0.93; I2=2%) (test for subgroup differences: Chi2=1.60, df=2 (p=0.45), I2=0%) (Figure 2).
Publication bias assessed using funnel plots is shown in Figures 3 and 4 (supplementary material).
DiscussionLeft ventricular thrombus is a major cause of embolic stroke after MI and heart failure. To date, current practice society guidelines recommend warfarin as a first-line oral therapy.24,25 More than a decade has passed, and no formal or upgrades to the current guidelines have been made has to recommend the usage of DOACs in patients with LV thrombus and otherwise no other formal indication for VKA usage. The favorable pharmacological and clinical profile of DOAC associated with their ease of administration, absence of a requirement for international normalized ratio monitoring, and absence of dietary restrictions make them increasingly attractive alternatives to VKAs.26 Nonetheless, there is a lack of scientific evidence regarding their safety (major bleeding requiring transfusion, intracranial hemorrhage, ischemic stroke, peripheral embolization) when compared to VKAs. This keeps the medical community from adopting them as first-line therapy.
The present meta-analysis gathers retrospective, prospective, and observational cohort studies allowing for an overall look and update on the currently existing scientific evidence. The common outcomes of the 14 studies analyzed were efficacy and safety of oral anticoagulation (DOACs vs. VAKs) in the treatment of LVT, with thirteen of these studies also including ischemic events (stroke and/or systemic embolism), and four of them including all-cause mortality. Nine of these studies described an individualized analysis for each DOAC.
The efficacy, all-cause mortality, and ischemic outcomes showed no significant differences between the two groups (DOACs vs. warfarin). Regarding the bleeding risk, different classifications of bleeding events were used. Still, in terms of relevant bleeding events (minor or major) the results showed similar results for both DOACs and VKAs groups, with no significant differences in the overall analysis.
As noted, no randomized trials have compared VKAs to DOACs for the prevention of thrombus formation in patients at high risk or for the treatment of LVT. Nonetheless, more recent data have been published showing that DOACs usage was safe and effective in patients with documented LVT, some with recent ST-elevation MI.27–29
LimitationsMost of the studies included were observational studies, and consequently, endpoint and classification varied according to each study's definition. This analysis may be underpowered to extrapolate the efficacy and safety of individual DOACs compared to warfarin. DOAC dose and the duration of treatment were not investigated in this analysis, as most studies did not thoroughly report the protocol.
ConclusionGiven these results, which combine an assessment and follow-up of a total of 2498 patients (n=631 DOACs and n=1867 for VKAs), it becomes clearer that the off-label use of DOACs for the treatment of LVT is non-inferior to VKAs and adds a better pharmacological and clinical profile, with the improvement of the patient's quality of life. Despite the limitations, this meta-analysis is a stepping-stone for the inclusion of DOACs as first-line therapy in future guidelines.
FundingNone declared.
Conflicts of interestThe authors have no conflicts of interest to declare.