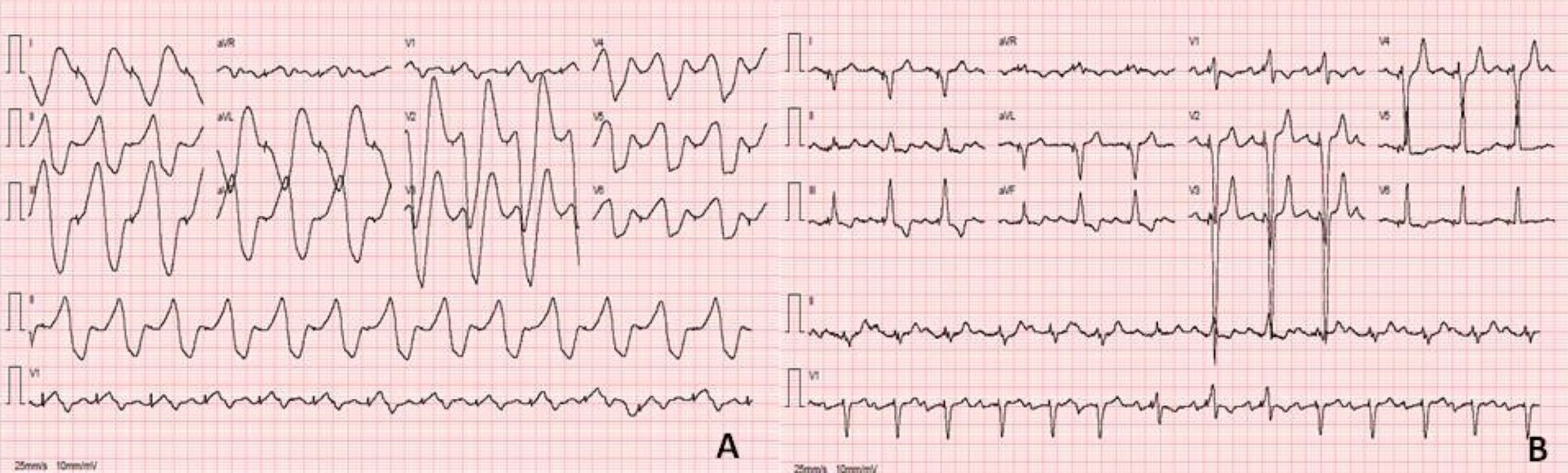
A 58-year-old woman with a history of idiopathic dilated cardiomyopathy and a cardiac resynchronization therapy device (CRT-D) for primary prevention came to the emergency room with “poorly characterized chest pain,” present three hours prior to arrival, and asthenia. On physical examination, she was unresponsive and pale. Her blood pressure was 61/28 mmHg and her heart rate 85 bpm. Electrocardiogram (ECG) showed widened QRS complexes with sine wave appearance (Figure 1A). Arterial blood gas analysis showed hyperkalemia with 8.5 mmol/L. The patient received urgent treatment with fluids, calcium gluconate, dextrose and an insulin infusion while the ECG was monitored. An additional ECG showed sinus rhythm with pacemaker-mediated ventricular conduction (Figure 1B). Hyperkalemia triggers progressive electrocardiographic changes, beginning with peaked T waves and PR prolongation. More severe potassium elevations can result in QRS widening and loss of P waves, with the eventual formation of a sine-wave pattern, as seen here. The rhythm can also degenerate into ventricular fibrillation.
The authors have no conflicts of interest to declare.