Kawasaki disease (KD) with cardiac involvement can result in the development of coronary aneurysm, stenosis or thrombosis with significant cardiovascular implications. We report the case of a 23-month-old male with a late diagnosis of KD, in whom intravenous immunoglobulin treatment was not feasible. The patient's course was assessed by routine echocardiography. At the age of five years, angiographic assessment revealed an aneurysm of the anterior descending coronary artery measuring 17 mm×7 mm involving the first diagonal branch, 90% post-aneurysmal stenosis, and an aneurysm of the right coronary artery measuring 32 mm×6 mm. Due to the critical anatomy of the anterior descending artery the revascularization method of choice was coronary artery bypass surgery with an internal mammary artery graft, under cardiopulmonary bypass. There were no significant intraoperative or postoperative complications. This confirms coronary artery bypass grafting as a reliable treatment option for patients who present with coronary sequelae from KD, even at a very young age.
A doença de Kawasaki pode resultar no desenvolvimento de aneurisma, estenose e trombose coronária com importantes implicações cardiovasculares. Reportamos o caso de um doente do sexo masculino de 23 meses com o diagnóstico tardio de doença de Kawasaki, impossibilitando o tratamento atempado com imunoglobulina endovenosa. O doente foi seguido em ambulatório com controlo ecocardiográfico e angiográfico. Aos cinco anos de idade a coronariografia revelava: a) aneurisma da artéria descendente anterior com 17×7 mm, envolvendo a primeira diagonal; b) estenose de 90% pós-aneurismática: c) aneurisma da coronária direita com 32×6 mm. Tendo em consideração a anatomia crítica da lesão envolvendo a artéria descendente anterior, a estratégia de intervenção escolhida foi cirurgia de revascularização miocárdica com um enxerto de artéria mamária esquerda in situ, sob circulação extracorporal. O procedimento decorreu sem intercorrências intra ou pós-operatórias de relevo. A cirurgia de revascularização miocárdica apresenta-se como uma opção viável na presença de sequelas coronárias de doença de Kawasaki, mesmo em doentes muito jovens.
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is a vasculitis of unknown etiology first described by Tomisaku Kawasaki in 1961, in Japan.1 Its incidence in Portugal is estimated at six per 100 000 children under five years of age,2 which is comparable to the range reported in other European studies.2,3
In the acute phase its clinical features include fever, typical changes in the mucous membranes, edema and desquamation of the extremities, polymorphous rash and cervical adenopathies. However, the major morbidity associated with KD is cardiac involvement due to vasculitis of medium-sized vessels.4 Coronary artery aneurysm (CAA) is the classic KD-related complication. CAA occurs in 15-25% of untreated patients2,5–7 and can be demonstrated by echocardiography as soon as seven days after fever onset. Formation of CAAs is most common in the proximal left anterior descending artery (LAD) and the proximal right coronary artery (RCA), especially at branch points.8
Approximately half of CAAs regress to normal lumen diameter within two years of illness onset. The likelihood of regression is inversely proportional to the diameter of the aneurysm.3,5,6 CAAs in patients with onset in infancy, proximal location, or saccular form, are also less likely to regress.3,6,8
Persistent CAAs are prone to the development of stenosis, tortuosity, calcification and thrombosis; they can be responsible for myocardial infarction (<5%) and death (1-5%).5,7–9
Case reportA 23-month-old male presented at his local hospital with desquamation of the extremities, two weeks after onset of fever, cervical adenopathies, strawberry tongue, conjunctivitis and cheilitis. He had a three-year-old half-brother with surgically corrected complex congenital heart disease. No other significant family or personal medical history was present. He was diagnosed with KD associated with large aneurysms and treated with aspirin. Due to the late diagnosis, intravenous immunoglobulin (IVIG) was not given at the time of diagnosis.
After completing nine months of dual antithrombotic therapy with low-dose aspirin and clopidogrel, the patient was assessed by diagnostic coronary angiography, which identified CAAs of the proximal LAD measuring 22 mm×8 mm and of the proximal RCA measuring 25 mm×6 mm. He was then started on warfarin and monitored with regular echocardiographic assessment. No change in CAA measurements was documented in the subsequent echocardiographic exams or by repeat coronary angiography one year later.
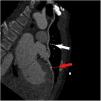
At five years of age, weighing 23.1 kg and measuring 116 cm, the patient was re-catheterized and progression of the previously documented lesions was noted. He was asymptomatic. Physical examination was unremarkable. Coronary angiography showed a CAA of the LAD measuring 17 mm×7 mm involving the first diagonal branch associated with a 90% post-aneurysmal stenosis (Figure 1), and a CAA of the RCA measuring 32 mm×6 mm.
The patient was admitted and myocardial revascularization was proposed. As ostial and long-segment lesions of important coronary arteries had been documented, coronary artery bypass grafting (CABG) was the procedure of choice.
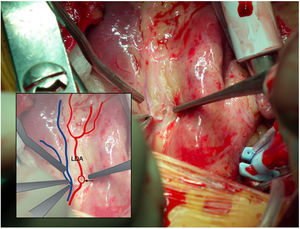
Surgery was performed under general anesthesia. A standard median sternotomy was performed and the left internal mammary artery (LIMA) was harvested. After administration of full-dose heparin, cardiac bypass was established by cannulation of the ascending aorta (16 Fr Medtronic DLP cannula) and the right atrial appendage (28 Fr Medtronic DLP). Anastomosis of the pediculated, non-skeletonized LIMA to the proximal LAD was performed (Figure 2) in the usual manner with an 8-0 polypropylene suture, after ascending aortic clamping and anterograde administration of cold cardioplegic solution. Intraoperative findings consisted of a LIMA with a diameter of 1.5 mm and very good pulsatile flow and a LAD without signs of degeneration, inflammation or calcification, and a diameter of approximately 1 mm distal to the aneurysm. Total bypass time was 28 minutes and total ischemic time was 14 minutes.
The postoperative period was uneventful. Echocardiographic assessment before discharge revealed good biventricular function with no segmental changes of ventricular function.
The patient was discharged six days after CABG, medicated with aspirin 4.3 mg/kg once daily, propranolol 10 mg three times daily, furosemide 10 mg twice daily and warfarin with target international normalized ratio 2-2.5.
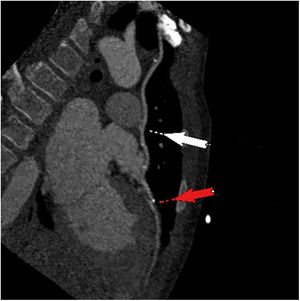
At the time of this report the patient was asymptomatic, with no electrocardiographic, echocardiographic or clinical signs of ischemia. Coronary computed tomography angiography two years after surgery revealed patency of the graft with good distal perfusion of the LAD (Figure 3).
DiscussionAccording to Yuan's review of 637 patients with KD who underwent cardiac surgery between 1990 and 2011, the disease has a male-to-female ratio of 3.1:1. The mean age of onset was 4±3.6 years, the mean age at time of surgery was 13.3±11.1 years and the interval between onset and surgical procedure was 9.5±9.4 years.7 In this review, myocardial infarction occurred in 28.9% of cases, the inferior wall being the most common region of infarction (40.8%). The most common coronary changes found were stenosis, total occlusion and CAA. The most reported intervention was CABG under standard cardiopulmonary bypass, with a mean of 1.67±0.8 grafts per patient, LIMA to LAD being the most commonly used bypass graft.
Management of the cardiac sequelae of KD consists, on the one hand, of prevention and treatment strategies for coronary thrombosis and myocardial infarction and, on the other hand, coronary revascularization procedures when appropriate, to relieve angina and diminish the risk of myocardial infarction and sudden death.5,8
Thrombus formation can easily develop in spite of anticoagulation therapy, and the risk of myocardial infarction and sudden death persists even if correct medical therapy is established.7 In addition, coronary aneurysms with an internal diameter >8 mm or with a z-score ≥10 are associated with a higher risk of cardiac events, making coronary revascularization procedures an important issue.8
KD represents a challenge as far as percutaneous coronary intervention (PCI) is concerned, as low body weight and severely calcified coronary arteries often lead to failure of stent implantation.7,10 Although PCI has been used with success is some cases, CABG appears to be more efficacious.5,7
Evidence regarding coronary revascularization procedures in this population is limited, as it is derived from expert consensus, retrospective reviews and data from the adult population with coronary artery disease.
According to the Research Committee of the Japanese Ministry of Health, Labor and Welfare, CABG should be the revascularization procedure of choice for patients with severe left ventricular dysfunction or presenting multiple, ostial or long-segment coronary lesions. The American Heart Association guidelines state that CABG should be considered when reversible ischemia is present on stress-imaging test results, perfusing the myocardium through the graft is still viable, and no appreciable lesions are present in the artery distal to the planned graft site.11 In addition, these guidelines, list as potential indications for CABG, severe occlusion of the left main coronary artery, severe occlusion of the proximal segment of the LAD, severe occlusion of more than one major coronary artery, and recurrent myocardial infarction.11
Internal mammary grafts grow with the child's somatic growth and have additional benefits in terms of endothelial function, and are therefore the conduit of choice for these patients.5,10,11
Arterial grafts in KD patients have been associated with patency rates of 94%, 82%, and 78% at one, five, and 10 years, respectively; and freedom from cardiac events was 70 at 10 years.12
This case report stresses the importance of early diagnosis and correct management of KD in order to avoid late cardiac sequelae, but also highlights the importance of systematic follow-up and parental education in order to detect coronary lesions that can lead to an adverse prognosis. Treatment with IVIG within 10 days of fever onset, which is associated with a five-fold reduction in CAA, is of great importance.2,3,8 This treatment was not feasible in the present case due to the late diagnosis.
ConclusionWhen performed by an experienced surgeon, CABG is a reliable treatment option for patients who present with coronary sequelae from KD, even at a very young age. As the inflammatory nature of KD is different from the pathophysiology commonly associated with atherosclerotic heart disease, prognostic considerations cannot be extrapolated from the adult coronary population. Further studies with longer follow-up will eventually enable recommendations to be made regarding conduit selection, myocardial revascularization methods and long-term prognosis.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank Dr. João Abecasis for the coronary computed tomography angiography image presented in this case report.