Coronary artery aneurysm (CAA) formation is a rare complication of coronary intervention that may develop after implantation of bare-metal or drug-eluting stents. The etiology of this entity appears to be multifactorial and its prognosis is poorly understood, but it has been associated with an increased risk of stent thrombosis. To date few cases of CAAs related to bioresorbable vascular scaffold (BVS) implantation have been reported, and the development of CAA after BVS implantation for the treatment of in-stent restenosis (ISR) has not been previously described. Here we present two cases of CAA formation after BVS, which represent the first demonstration of CAA formation after the use of BVS for ISR.
A formação de um aneurisma coronário (CAN) é uma complicação rara após intervenções coronárias. O CAN pode se desenvolver após stent convencional (BMS) e implante de stent farmacológico (DES). A etiologia desta patologia parece ser multifatorial e o prognóstico permanece mal elucidado, mas tem sido associado com um aumento do risco de trombose de stent. Até à data, apenas alguns casos de CAN relacionadas com scaffold bioabsorvível (BVS) foram relatados. O desenvolvimento de CAN após o implante de um BVS para o tratamento da reestenose intra-stent (ISR) não foi anteriormente descrito. Aqui apresentamos dois casos de formação CAN após a BVS, que representam a primeira demonstração de formação CAN após o uso da BVS para ISR.
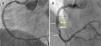
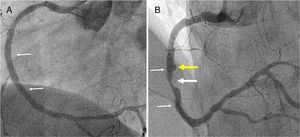
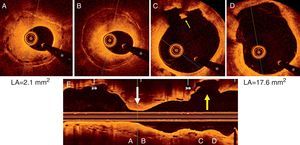
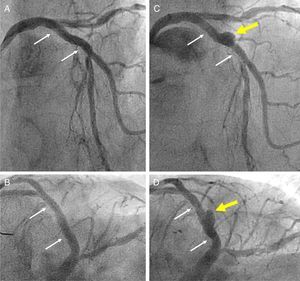
A 45-year-old man with previous history of hyperlipidemia was admitted with an inferior myocardial infarction requiring implantation of a drug-eluting stent (DES) in the mid right coronary artery. One year later he presented with angina and angiography demonstrated severe in-stent restenosis (ISR). After lesion predilation with a cutting balloon, a 3.5 mm×18 mm bioresorbable vascular scaffold (BVS) (Absorb, Abbott Vascular, CA) was implanted and postdilated up to 24 atm using a non-compliant balloon, with an excellent final result (Figure 1A). Optical coherence tomography (OCT) confirmed appropriate expansion and apposition of the BVS, with a minor intimal dissection at its proximal edge. The patient remained completely asymptomatic, but at nine months underwent a scheduled angiography that revealed moderate ISR of the BVS. In addition, a coronary artery aneurysm (CAA) was detected immediately proximal to the BVS location (Figure 1B). OCT showed the presence of an heterogeneous pattern of neointimal hyperplasia (Figure 2A and B) and confirmed the origin of the CAA immediately proximal to the BVS edge (Figure 2C and D). Interestingly, a minor rupture with intraluminal thrombus was also detected at the origin of the CAA. As fractional flow reserve was 0.79 and instantaneous wave-free ratio was 0.93, and the patient denied any symptoms, the lesion was not treated. During follow-up, a stress echocardiogram was negative.
Optical coherence tomography images showing (A and B) an heterogeneous pattern of neointimal hyperplasia with a minimum lumen area (LA) of 2.1 mm2; (C and D) formation of a coronary artery aneurysm (CAA) at the proximal border of the bioresorbable vascular scaffold (BVS) with a maximum LA of 17.6 mm2. A minor rupture with associated intraluminal thrombus was visualized (small yellow arrow) (C); (E) longitudinal view depicting the segment with in-stent restenosis (white arrow) and the CAA (yellow arrow) at the edge of the BVS. * denotes wire artefact. LA: lumen area.
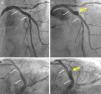
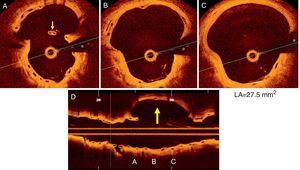
A 67-year-old man with hyperlipidemia was admitted for effort angina. Fifteen years before he had suffered an anterior myocardial infarction and a bare-metal stent (BMS) was implanted in the proximal left anterior descending coronary artery. Coronary angiography revealed proliferative ISR involving the proximal segments of the BMS but also extending 10 mm into the proximal vessel. OCT depicted severe neoatherosclerosis, with heavily calcified plaques, and a thin-cap fibroatheroma in the proximal segment. After aggressive lesion predilation the entire segment was covered with a 3.5 mm×23 mm BVS (Absorb, Abbott Vascular, CA), postdilated using a non-compliant balloon up to 24 atm, with an excellent final result (Figure 3A and B). OCT confirmed correct BVS expansion with a small residual coronary dissection behind the BVS and at its proximal border. The patient remained completely asymptomatic but a scheduled control angiogram at nine months revealed the development of a large CAA in the mid portion of the BVS (Figure 3C and D). OCT provided unique additional insights, revealing a CAA 11 mm in length with a maximum lumen area of 27.5 mm2. Notably, a striking displacement of the BVS struts was depicted, confirming the occurrence of BVS fracture (Figure 4).
(A and B) Angiographic result after implantation of a bioresorbable vascular scaffold (BVS) in the proximal left anterior descending coronary artery (small white arrows indicate the ends of the BVS); (C and D) at nine-month follow-up formation of a coronary artery aneurysm (yellow arrow) is demonstrated in the mid segment of the BVS.
(A-D) Optical coherence tomography images of the coronary artery aneurysm (CAA) (yellow arrow) with a maximum lumen area of 27.5 mm2. Some struts of the bioresorbable vascular scaffold appear covered but largely malapposed (A, thin yellow arrow), others were extensively displaced (B), whereas no struts could be detected in other areas of the CAA (C); (D) longitudinal view. * denotes wire artefact. LA: lumen area.
CAA formation is very rare after stent implantation. The prevalence of this complication after DES implantation ranges between 0.76 and 1.25%.1,2 Different pathophysiological mechanisms have been implicated in the development of CAA, including extensive vessel wall injury (particularly major underlying coronary dissections), excessive positive vessel remodeling, hypersensitivity reactions, stent fractures and even local infection.1 The role of the eluting drug and polymer appears crucial. The same factors have been implicated in the few cases of CAA development after BVS reported to date.3,4 In our patients BVS-related dissections may have been implicated in the pathogenesis of this entity. Moreover, in the second patient the major underlying vessel disruption may have promoted BVS fracture. The Restenosis Intrastent: Bioresorbable Vascular Scaffolds Treatment (RIBS VI) study (an ongoing multicenter registry on the use of BVS for ISR) will provide further insight into the safety and efficacy of BVS in this challenging anatomic scenario.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.