To assess the clinical impact of a cardiac rehabilitation program in an older population.
MethodsThis is a retrospective analysis of 731 coronary patients who attended phase 2 of a cardiac rehabilitation program between January 2009 and December 2016. We compared the response to the program of older (≥65 years) and younger (<65 years) patients, analyzing changes in metabolic profile (including body mass index, waist circumference and lipid profile), exercise capacity, cardiac autonomic regulation parameters (such as chronotropic index and resting heart rate), and health-related quality of life scores.
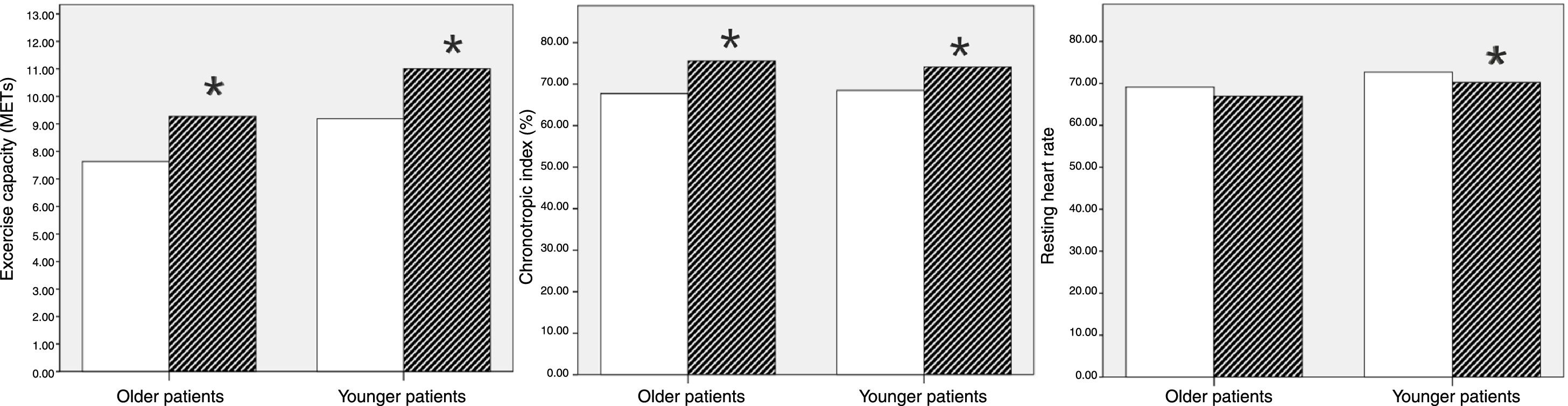
ResultsOlder patients represented 15.9% of our cohort. They showed significant reductions in waist circumference (male patients: 98.0±7.9 cm vs. 95.9±7.9 cm, p<0.001; female patients: 90.5±11.4 cm vs. 87.2±11.7 cm, p<0.001), LDL cholesterol (102.5 [86.3-128.0] mg/dl vs. 65.0 [55.0-86.0] mg/dl, p<0.001) and triglycerides (115.0 [87.8-148.5] mg/dl vs. 97.0 [81.8-130.0] mg/dl, p<0.001). Post-training data also showed a noticeable improvement in older patients’ exercise capacity (7.6±1.8 METs vs. 9.3±1.8 METs, p<0.001), along with a higher chronotropic index and lower resting heart rate. Additionally, health-related quality of life indices improved in older subjects. However, our overall analysis found no significant differences between the groups in changes of the studied parameters.
ConclusionOlder coronary patients benefit from cardiac rehabilitation interventions, similarly to their younger counterparts. Greater involvement of elderly patients in cardiac rehabilitation is needed to fully realize the therapeutic and secondary preventive potential of such programs.
Avaliar o impacto clínico de um programa de reabilitação cardíaca na população idosa.
MétodosEstudo retrospetivo constituído por 731 doentes com doença coronária, que concluíram a fase II de um programa de reabilitação cardíaca entre janeiro de 2009 e dezembro de 2016. Comparámos a resposta ao programa dos idosos (≥ 65 anos) e dos jovens (< 65 anos), avaliando as alterações no perfil metabólico (incluindo o índice de massa corporal, perímetro abdominal e perfil lipídico), capacidade funcional, parâmetros de função autonómica cardíaca (como o índice cronotrópico e frequência cardíaca em repouso) e qualidade de vida.
ResultadosOs idosos representaram 15,9% da população. Estes mostraram uma redução significativa do perímetro abdominal (homens: 98,0±7,9 cm versus 95,9±7,9 cm, p<0,001; mulheres: 90,5±11,4 cm versus 87,2±11,7 cm, p<0,001), bem como uma redução nos níveis de colesterol-LDL (102,5 [86,3; 128,0] mg/dl versus 65,0 [55,0; 86,0] mg/dl, p<0,001) e de triglicerídeos (115,0 [87,8; 148,5] mg/dl versus 97,0 [81,8; 130,0] mg/dl, p<0,001). No fim do programa, os idosos aumentaram a sua capacidade funcional (7,6±1,8 METs versus 9,3±1,8 METs, p<0,001) e o índice cronotrópico e apresentaram uma redução na frequência cardíaca de repouso. Adicionalmente, estes doentes demonstraram um aumento dos índices de qualidade de vida. Comparando os resultados dos dois grupos no fim do programa, não encontrámos diferenças relevantes nas alterações dos parâmetros estudados.
ConclusãoOs idosos com doença coronária beneficiam do programa de reabilitação cardíaca e este benefício é equiparável ao encontrado nos doentes jovens. É fundamental aumentar a referenciação deste subgrupo para que estes possam usufruir do potencial preventivo e terapêutico destes programas.
Cardiac rehabilitation (CR) is a comprehensive program that combines exercise training and lifestyle interventions, and is recommended in patients after an acute coronary syndrome.1 The positive effects of CR on mortality, morbidity, quality of life and psychological well-being are recognized.2 Despite these benefits, some patient subgroups are consistently under-enrolled, including older patients. Participation in secondary prevention programs only reaches around 20% of eligible older patients, and long-term adherence is even worse.3 Besides cardiac disease, aging is associated with increased prevalence of other comorbidities, including musculoskeletal disease, peripheral arterial disease, chronic respiratory disease, cerebrovascular disorders and cognitive impairment,4 which can limit the implementation of exercise-based CR programs. Furthermore, acute disease and hospitalization may aggravate the vulnerability of older patients and contribute to progressive disability. The purpose of this study was to study older patients who attended CR programs and to assess the clinical impact of this intervention in this subgroup compared to younger patients.
MethodsEthicsThe procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 1983.
SubjectsWe performed a retrospective analysis of 731 consecutive patients referred for CR at Centro Hospitalar São João, Porto, after an acute coronary syndrome, between January 2009 and December 2016. Only patients who completed at least 50% of scheduled sessions were included. Patients were stratified in two age groups according the World Health Organization criteria4: older (≥65 years) and younger (18-64 years).
Characteristics of the study populationInformation concerning demographics, cardiovascular (CV) risk profile, characterization of the index acute coronary event, left ventricular systolic function (assessed by transthoracic echocardiography, with dysfunction being classified as mild, moderate or severe, according to international guidelines5), and discharge medication was collected from clinical records.
Response to the cardiac rehabilitation programThe response to the CR program was assessed considering its effects on metabolic profile, exercise capacity (EC) and cardiac autonomic regulation, as well as on health-related quality of life scores.
Patients’ metabolic profiles were analyzed based on body mass index (BMI), waist circumference, and low-density lipoprotein (LDL) cholesterol and triglyceride (TG) levels. Weight was measured to the nearest kg using a balanced floor scale. Waist circumference was measured twice by a single observer using a standard tape measure at the level of the patient's umbilicus and the mean value recorded to the nearest cm. Laboratory tests were performed on blood samples collected after 12 hours’ fasting. To compare the effect of CR on the metabolic profile of both groups, we used the relative changes between baseline, at admission in hospital during the index coronary event (pre-CR) and final (post-CR) measurements (eg.: post-CR LDL level-pre-CR LDL level)/pre-CR LDL level×100), expressed as a percentage.
All patients underwent standard exercise testing using the Bruce protocol at baseline and at the end of phase 2 of the CR program. EC was assessed using maximum metabolic equivalents (METs) achieved in exercise testing. Chronotropic index (CI) and resting heart rate (HR) were also analyzed as measures of autonomic nervous system regulation. CI was calculated using the equation: (peak exercise HR-resting HR/[220-age]-resting HR)×100, expressed as a percentage. The relative changes between pre-CR and post-CR measurements were also used to compare the effect of the CR program on EC, CI and resting HR in both groups.
Health-related quality of life was assessed using the 36-Item Short Form Health Survey (SF-36), a reliable and validated instrument for measuring health-related quality of life in ischemic heart disease patients.6 It consists of 36 items, 35 of which are grouped under eight multi-item scales that measure physical functioning, role limitations due to physical health problems, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and mental health. The eight scales, in turn, are aggregated into two summary scales tapping physical and mental health: a physical component summary (PCS-36) and a mental component summary (MCS-36). Higher scores in both components of the SF-36 indicate a better state of health-related quality of life. The information was collected at baseline and at the end of phase 2 of the CR program, and the changes between these two assessment points were compared according to age.
InterventionThe CR program was organized in sequential phases, in accordance with published guidelines.7,8 Only patients who completed phases 1 and 2 were included.
Phase 1, during hospital stay, included educational programs for patients about their disease and control of CV risk factors. Early mobility was also encouraged in order to achieve independence in daily activities before hospital discharge. Phase 2 consisted of an outpatient multiprofessional intervention which started a mean of 17.5 days after hospital discharge. This phase included supervised exercise training, nutritional assessment and individualized dietary plans, as well as smoking cessation counseling. Exercise training consisted of biweekly 40-60 min medically supervised sessions at our Cardiovascular Prevention and Rehabilitation Unit, lasting up to three months. For the aerobic component (combination of treadmill, cycle ergometer, rowing machine, and stair climber apparatus), we used a continuous moderate intensity modality set to 60-80% of HR reserve achieved at baseline exercise testing (using Karvonen's formula) along with perceived exertion using the Borg scale between 11 and 13 points (fairly light to somewhat hard). Exercise was set at high repetition and low resistance, consisting of two sets of 15 repetitions per exercise (chest press, leg press and segmental exercises for biceps, triceps and latissimus dorsi), with patients instructed to maintain 1:1 contraction/relaxation cycles and to avoid excessive straining with Valsalva maneuver.
Patients received specific instructions on promoting physical activity to achieve recommended standards, consisting of an average of 600 METs-min/week (40 min per day of moderate intensity activity, such as brisk walking or equivalent). Active smokers received individual assessment and intervention by a trained psychologist through psychobehavioral sessions and pharmacological treatment when needed. Medical therapy was tailored at tolerated maximum doses, according to the international guidelines for secondary prevention of coronary artery disease.1
Statistical analysisQualitative variables were presented as percentages and compared by the chi-square test. Normally distributed quantitative variables were expressed as mean ± standard deviation and compared using the independent sample t test or the paired sample t test as appropriate. Non-normally distributed variables were expressed as median (interquartile range) and compared using the Mann-Whitney or the non-parametric Wilcoxon signed-rank test as appropriate. Multivariate analysis, using binary logistic regression, was performed to adjust the results to possible confounders, particularly the baseline features and endpoints studied. Values of p<0.05 were considered statistically significant. The statistical analysis was performed using IBM SPSS Statistics® version 23.0.
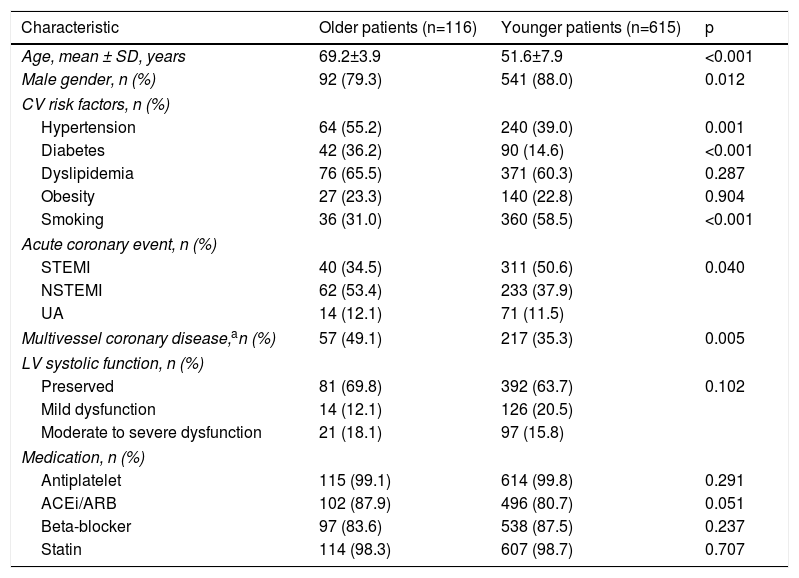
ResultsDemographic and clinical characteristics of the study populationBaseline patient characteristics are listed in Table 1. Older patients represented 15.9% of the population, with a mean age of 69.2±3.9 years. Younger patients had a mean age of 51.6±7.9 years. There was a higher prevalence of hypertension (55.2% vs. 39.0%, p=0.001) and diabetes (36.2% vs. 14.6%, p<0.001) among older patients, while smoking was more frequent in the younger group. Clinical presentation of acute coronary syndrome was different between the groups; non-ST-elevation myocardial infarction was the main diagnosis in older patients (53.4% vs. 37.9%), whereas ST-elevation myocardial infarction was the main diagnosis in younger patients (50.6% vs. 34.5%), p=0.04. Moreover, the prevalence of multivessel disease, defined as the presence of ≥70% stenosis of two or more epicardial coronary arteries on coronary angiography, was higher in older patients (49.1% vs. 35.3%, p=0.005). On the other hand, no significant differences were found between the groups in left ventricular systolic function or medical treatment. Most patients in both groups were taking antiplatelet agents, beta-blockers and statins.
Baseline characteristics of the study population.
| Characteristic | Older patients (n=116) | Younger patients (n=615) | p |
|---|---|---|---|
| Age, mean ± SD, years | 69.2±3.9 | 51.6±7.9 | <0.001 |
| Male gender, n (%) | 92 (79.3) | 541 (88.0) | 0.012 |
| CV risk factors, n (%) | |||
| Hypertension | 64 (55.2) | 240 (39.0) | 0.001 |
| Diabetes | 42 (36.2) | 90 (14.6) | <0.001 |
| Dyslipidemia | 76 (65.5) | 371 (60.3) | 0.287 |
| Obesity | 27 (23.3) | 140 (22.8) | 0.904 |
| Smoking | 36 (31.0) | 360 (58.5) | <0.001 |
| Acute coronary event, n (%) | |||
| STEMI | 40 (34.5) | 311 (50.6) | 0.040 |
| NSTEMI | 62 (53.4) | 233 (37.9) | |
| UA | 14 (12.1) | 71 (11.5) | |
| Multivessel coronary disease,an (%) | 57 (49.1) | 217 (35.3) | 0.005 |
| LV systolic function, n (%) | |||
| Preserved | 81 (69.8) | 392 (63.7) | 0.102 |
| Mild dysfunction | 14 (12.1) | 126 (20.5) | |
| Moderate to severe dysfunction | 21 (18.1) | 97 (15.8) | |
| Medication, n (%) | |||
| Antiplatelet | 115 (99.1) | 614 (99.8) | 0.291 |
| ACEi/ARB | 102 (87.9) | 496 (80.7) | 0.051 |
| Beta-blocker | 97 (83.6) | 538 (87.5) | 0.237 |
| Statin | 114 (98.3) | 607 (98.7) | 0.707 |
ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; CV: cardiovascular; LV: left ventricular; NSTEMI: non-ST-elevation myocardial infarction; SD: standard deviation; STEMI: ST-elevation myocardial infarction; UA: unstable angina.
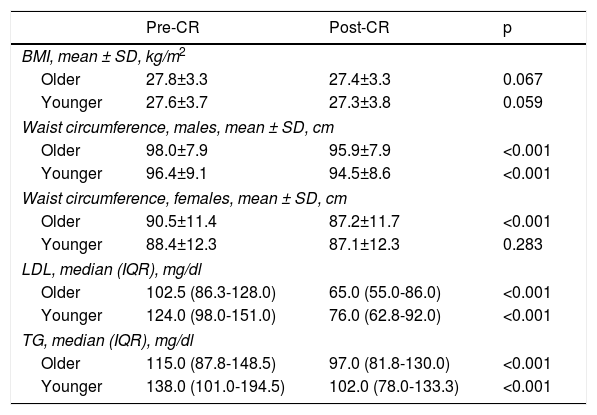
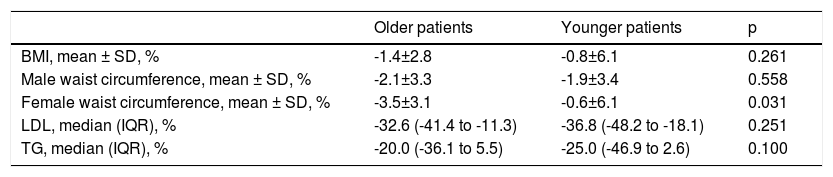
Participation in CR sessions did not differ between groups (older patients: 15.7±4.2; younger patients: 14.3±4.5, p=0.127). Even though no significant changes in BMI were found, older patients demonstrated a significant reduction in waist circumference (male: 98.0±7.9 cm vs. 95.9±7.9 cm, p<0.001; female: 90.5±11.4 cm vs. 87.2±11.7 cm, p<0.001). Significant reductions were also seen in lipid profile (LDL cholesterol: 102.5 [86.3-128.0] mg/dl vs. 65.0 [55.0-86.0] mg/dl, p<0.001; triglycerides: 115.0 [87.8-148.5] mg/dl vs. 97.0 [81.8-130.0] mg/dl, p<0.001), as shown in Table 2. Comparing older patients to the younger group (Table 3), we found that improvements in waist circumference measurements of older female patients were greater than in younger women (-3.5±3.1% vs. -0.6±6.1%, p=0.031), even after adjusting for baseline features and the other study endpoints (odds ratio 0.754, p=0.036).
Within-group comparison of metabolic profile.
| Pre-CR | Post-CR | p | |
|---|---|---|---|
| BMI, mean ± SD, kg/m2 | |||
| Older | 27.8±3.3 | 27.4±3.3 | 0.067 |
| Younger | 27.6±3.7 | 27.3±3.8 | 0.059 |
| Waist circumference, males, mean ± SD, cm | |||
| Older | 98.0±7.9 | 95.9±7.9 | <0.001 |
| Younger | 96.4±9.1 | 94.5±8.6 | <0.001 |
| Waist circumference, females, mean ± SD, cm | |||
| Older | 90.5±11.4 | 87.2±11.7 | <0.001 |
| Younger | 88.4±12.3 | 87.1±12.3 | 0.283 |
| LDL, median (IQR), mg/dl | |||
| Older | 102.5 (86.3-128.0) | 65.0 (55.0-86.0) | <0.001 |
| Younger | 124.0 (98.0-151.0) | 76.0 (62.8-92.0) | <0.001 |
| TG, median (IQR), mg/dl | |||
| Older | 115.0 (87.8-148.5) | 97.0 (81.8-130.0) | <0.001 |
| Younger | 138.0 (101.0-194.5) | 102.0 (78.0-133.3) | <0.001 |
BMI: body mass index; IQR: interquartile range; LDL: low-density lipoprotein; Post-CR: post-cardiac rehabilitation program; Pre-CR: pre-cardiac rehabilitation program SD: standard deviation; TG: triglycerides.
Comparison of changes in metabolic profile between older and younger patient groups after cardiac rehabilitation.
| Older patients | Younger patients | p | |
|---|---|---|---|
| BMI, mean ± SD, % | -1.4±2.8 | -0.8±6.1 | 0.261 |
| Male waist circumference, mean ± SD, % | -2.1±3.3 | -1.9±3.4 | 0.558 |
| Female waist circumference, mean ± SD, % | -3.5±3.1 | -0.6±6.1 | 0.031 |
| LDL, median (IQR), % | -32.6 (-41.4 to -11.3) | -36.8 (-48.2 to -18.1) | 0.251 |
| TG, median (IQR), % | -20.0 (-36.1 to 5.5) | -25.0 (-46.9 to 2.6) | 0.100 |
BMI: body mass index; IQR: interquartile range; LDL: low-density lipoprotein; SD: standard deviation; TG: triglycerides.
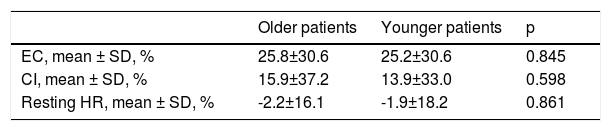
Regarding exercise testing results, there was also a marked improvement in older patients’ outcomes (Figure 1). Post-CR analysis showed an increase in their EC (7.6±1.8 METs vs. 9.3±1.8 METs, p<0.001), as well as an increase in CI (67.7±18.0% vs. 75.6±20.7%, p<0.001) and a reduction in resting HR (69.1±10.6 bpm vs. 66.9±11.9 bpm, p<0.001). However, no significant differences were seen between older and younger patients in relative changes in these parameters after exercise training (Table 4).
Comparison of changes in exercise testing parameters between older and younger patient groups after cardiac rehabilitation.
| Older patients | Younger patients | p | |
|---|---|---|---|
| EC, mean ± SD, % | 25.8±30.6 | 25.2±30.6 | 0.845 |
| CI, mean ± SD, % | 15.9±37.2 | 13.9±33.0 | 0.598 |
| Resting HR, mean ± SD, % | -2.2±16.1 | -1.9±18.2 | 0.861 |
CI: chronotropic index; EC: exercise capacity: HR, heart rate; SD: standard deviation.
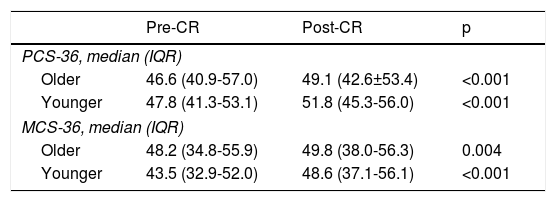
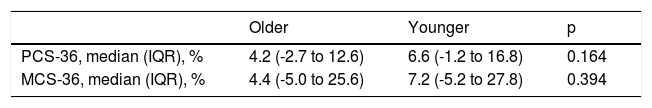
Finally, analyzing the impact of the CR program on health-related quality of life, older patients had improved SF-36 scores, on both the PCS-36 (46.6 [40.9-57.0] vs. 49.1 [42.6±53.4], p<0.001) and the MCS-36 (48.2 [34.8-55.9] vs. 49.8 [38.0-56.3], p=0.004) subscales, as shown in Table 5. As with exercise testing, the relative changes in both subscales in older patients were not significantly different from those of younger patients (Table 6).
Within-group comparison of 36-Item Short Form Health Survey results.
| Pre-CR | Post-CR | p | |
|---|---|---|---|
| PCS-36, median (IQR) | |||
| Older | 46.6 (40.9-57.0) | 49.1 (42.6±53.4) | <0.001 |
| Younger | 47.8 (41.3-53.1) | 51.8 (45.3-56.0) | <0.001 |
| MCS-36, median (IQR) | |||
| Older | 48.2 (34.8-55.9) | 49.8 (38.0-56.3) | 0.004 |
| Younger | 43.5 (32.9-52.0) | 48.6 (37.1-56.1) | <0.001 |
IQR: interquartile range; MCS-36: mental component summary of the 36-Item Short Form Health Survey; PCS-36: physical component summary of the 36-Item Short Form Health Survey; Post-CR: post-cardiac rehabilitation program; Pre-CR: pre-cardiac rehabilitation.
Comparison of changes in 36-Item Short Form Health Survey results after cardiac rehabilitation.
| Older | Younger | p | |
|---|---|---|---|
| PCS-36, median (IQR), % | 4.2 (-2.7 to 12.6) | 6.6 (-1.2 to 16.8) | 0.164 |
| MCS-36, median (IQR), % | 4.4 (-5.0 to 25.6) | 7.2 (-5.2 to 27.8) | 0.394 |
CRP: cardiac rehabilitation program; IQR: interquartile range; MCS-36: mental component summary of the 36-Item Short Form Health Survey; PCS-36: physical component summary of the 36-Item Short Form Health Survey.
Although older patients are under-represented in CR programs, this intervention provides broad benefits in these patients, from metabolic profile and functional capacity to health-related quality of life, as we show in the present study.
Changing body composition, including fat redistribution to central and visceral depots, is a hallmark of the physiological aging process, which has profound effects on health and physical function in older adults. Aerobic exercise appears to slow the age-related accumulation of central body fat and is cardioprotective.9 Although our results showed a neutral effect of CR on BMI, a significant reduction in waist circumference was found in both male and female older patients. Exercise training could contribute, at least in part, to an increase in lean/fat mass proportion, which could explain our results. Curiously, we found that reduction of waist circumference was greater in older female patients compared to their younger counterparts. Similar results were previously found. In 2016, Al Quait and Dohert10 compared CR outcomes of 262813 older (≥65 years) patients to 203012 younger (<65 years) patients and showed a positive correlation between older age and change in body shape risk factors. Regarding waist measurements, older female patients had the best outcomes. Other studies are needed to address this subject, considering all factors of female biology, to understand the impact of exercise training in aging women.
Additionally, in our cohort, the lipid profile of older patients improved, practically reaching the target levels recommended. CR programs have been demonstrated to improve lipid levels, the effect of a combination of exercise training, diet and lipid-lowering therapy.11 Our results suggest that these benefits extend to older patients as well.
We also analyzed changes in EC and cardiac autonomic regulation after exercise training. Although older patients performed worse in exercise testing at both assessment points, their EC improved in the same way as younger patients. The marked improvement in EC that we observed in our older patients agrees with previous reports. Balady et al.12 studied changes in EC following CR programs in patients stratified according to age and gender and found that older patients had lower baseline EC. Similarly, exercise training yielded improvement in exercise tolerance among patients in all age groups, without significant differences between groups.
Although the superimposition of CV disease on age-associated decline in aerobic capacity can result in functional impairment in older patients, exercise-based CR may counteract this effect, which can have prognostic implications. Reports on older patients with and without heart disease have demonstrated a positive impact of exercise training on their outcomes,3 while results from the Cardiovascular Health Study, including 5201 patients with a mean age of 73 years, suggested that level of physical activity is an independent predictor of five-year mortality.13
Cardiac autonomic regulation is also an important focus of interest in coronary patients. It is well known that chronotropic incompetence, usually defined as CI≤80%, is an independent predictor of all-cause death in these patients.14 In patients taking beta-blockers, the threshold for chronotropic incompetence has been reviewed and a cut-off of ≤62% has been proposed.15 In our cohort, nearly all patients were under beta-blocker therapy, which could explain the low baseline CI of both groups. Exercise training have been shown to improve measures of HR variability in patients after infarction.16 The same positive effect could be expected on resting HR, which usually decreases with regular physical activity. Although aging is associated with cardiac neurohormonal dysfunction, a decline in sinoatrial node parasympathetic activity and an increase in sympathetic activity,17 we found that CI and resting HR improved in older patients at the end of the phase 2 CR program, similar to younger patients.
Besides changes in metabolic profile and improvements in functional capacity, there is growing evidence on the impact of CR on quality of life. In the present study, we applied the SF-36 questionnaire to all patients at baseline and at the end of phase 2 of the CR program. Our data showed that, as in younger patients, CR has a positive effect on both the MCS-36 and PCS-36 subscales in older subjects. These findings are in agreement with results from other groups. For instance, Marchionni et al.18 compared CR program outcomes in older and younger patients, and found that the elderly group had significant improvements in all aspects of quality of life studied. Furthermore, Stewart and colleagues19 demonstrated that improved fitness enhances patients’ quality of life and can help older adults to live independently. A routine general psychological assessment of participants, including older subjects, has an important role in a CR program. Simple screening tools can help identify their main problems and can be followed by more sophisticated instruments and referral for treatment as needed. Health-related quality of life assessment not only can have impact on psychosocial well-being, but can also itself be a predictor of mortality, cardiovascular events, hospitalization and costs of care in patients with cardiovascular disease.20 Moreover, considering the role of regular exercise in maintaining mobility, exercise training is an important intervention to reduce or even prevent age-associated disability and can have a marked impact on the daily living needs of older patients. A systematic review of exercise interventions found that multicomponent exercise programs, including endurance, strength, flexibility, and balance training, generally reported significant reductions in disability for older patients. Longer duration of the intervention and follow-up, as well as interventions in more functionally limited individuals, were associated with greater likelihood of benefit.21
As CV risk increases in older population, including higher prevalence of CV risk factors and multivessel coronary disease, as demonstrated in our cohort, the absolute benefit of treatment should increase as well. Perhaps the greatest barrier to the benefits of cardiac rehabilitation in older adults with CV disease is their very low attendance rate in such programs. Practical issues related to the implementation of exercise training programs in older coronary patients include the frequent need for training regimens to be adjusted to accommodate the presence of age-related comorbidities. The least fit individuals are often unable to sustain exercise for long periods and do well starting at very low work levels and repeat intermittent brief bouts of exercise (interval training) that are gradually extended. This can promote progressive fitness, while reducing the potential for overuse injuries.16,22 Beyond their limitations with regard to exercise training, the major contributor to the low utilization of CR by elderly patients is the reluctance of providers to refer them for these programs.23 Many physicians do not recommend CR to their older patients or explain its potential value. Consequently, older adults are less likely to be aware of CR and to pursue options for CR which they do not understand. Additionally, older patients are more likely to live alone and have poor social support, which hampers their attendance at these programs.
This study emphasizes the significant impact of CR programs on the older population, including three aspects of their effects, namely metabolic profile, exercise capacity and health-related quality of life. CR provides an opportunity for longitudinal assessment to address older patients’ issues, redefine optimal management and ultimately improve their outcomes. Increased awareness of physicians, nurses, patients and their families of the benefits of secondary prevention programs like CR will provide a basis for referral and aid the implementation of such programs.
Some study limitations need to be highlighted. This is a retrospective study and selection and referral bias cannot be excluded; however, it represents an application of CR in real-life patient cohorts. Another limitation concerns the assessment of exercise capacity using estimated METs achieved in exercise testing, as opposed to precise measurement with cardiopulmonary gas exchange. Nevertheless, METs have a good correlation with peak oxygen uptake and constitute a valid measure of EC with prognostic value.24 Furthermore, it would be interesting to prolong the follow-up after phase 2 of the CR program to assess whether the effects of CR on metabolic profile, exercise performance and health-related quality of life are maintained over time. Finally, a subgroup analysis of very old patients would also help to determine whether the benefits of CR programs extend to these patients as well.
ConclusionsCurrent data support the beneficial effects of CR and exercise training in older populations, including improvements in metabolic profile, functional capacity and quality of life indices. This positive impact in older patients was at least similar to that observed in younger counterparts. It is crucial that clinicians strongly and repeatedly encourage older adults to participate in exercise-based CR programs, while carefully considering appropriate and individualized recommendations for exercise prescription.
Conflicts of interestThe authors have no conflicts of interest to declare.