Some atmospheric features have been linked to the triggering of myocardial infarction. Because data from the Temperate-Mediterranean is scarce, we sought to study whether meteorological parameters influence the incidence of ST-elevation myocardial infarction (STEMI) as confirmed by primary percutaneous intervention in a city with temperate weather (Porto, Portugal).
MethodsRetrospective analysis of a series of STEMI-patients from January 2010 to December 2017. Temperature (T), relative humidity (RH), precipitation, and atmospheric pressure were obtained from a government-led institute. We utilized a generalized linear model (GLM) with a Poisson distribution, where a series of models with multivariable analysis were computed. The effects (GLM coefficients) are presented as excess relative risk (ERR).
ResultsOne thousand and four consecutive STEMI-patients were included. The most important predictors of STEMI were Tmin two days before (for 1°C drop ERR=1.9%, p=0.009) and a 1% increase in RH three days before (EER=0.7%, p=0.006). Conversely, the same increase in RH the day before reduced the relative risk (EER=-0.6%, p=0.023). Temperature range, atmospheric pressure and precipitation had no impact on STEMI incidence.
ConclusionIn a Temperate-Mediterranean city hot or cold temperature extremes, temperature drop and relative humidity had a significant impact on the occurrence of STEMI.
Algumas características atmosféricas relacionam-se com a ocorrência aumentada de enfarte agudo do miocárdio. Uma vez que os dados relativos a zonas mediterrâneas temperadas são pouco conhecidos, o nosso objetivo foi estudar a incidência de enfarte com elevação de ST em doentes submetidos a angioplastia primária, em relação com parâmetros atmosféricos, numa cidade de clima mediterrâneo temperado (Csb).
MétodosAnálise retrospetiva de uma série de doentes com enfarte com elevação de ST tratados por angioplastia entre janeiro de 2010 e dezembro de 2017. Temperatura (T), humidade relativa (HR), precipitação e pressão atmosférica provenientes de registos do Instituto Português do Mar e da Atmosfera. Modelos de análise linear generalizada (GLM) com distribuição de Poisson foram utilizados para computar vários modelos de análise multivariada, calculando-se excesso de risco relativo (ERR) e respetivos coeficientes (GLM) para cada parâmetro atmosférico estudado.
ResultadosForam incluídos 1004 doentes consecutivos. Os principais preditores da ocorrência de enfarte foram a T mínima dois dias anteriores ao evento (para 1°C de diminuição, EER=1,9%, p=0,009) e 1% de aumento da HR três dias anteriores ao evento (EER=0,7%, p=0,006). Inversamente, o mesmo aumento da HR no dia anterior ao evento diminuiu o risco (EER=-0,6%, p=0,023). Não se obtiveram resultados significativos para a precipitação ou pressão atmosférica.
ConclusãoNuma cidade de clima mediterrâneo temperado sem insultos climáticos extremos, a diminuição da temperatura e o aumento da humidade relativa influenciaram a incidência de enfarte com elevação de ST.
The pathophysiology of an ST-elevation myocardial infarction (STEMI) usually begins with a rupture or erosion of an atherosclerotic plaque followed by coronary spasm and the activation of both platelets and coagulation cascade.1 This leads to thrombus formation and to a sudden obstruction of a coronary artery culminating in myocardial necrosis. To salvage the myocardium, immediate recanalization is warranted, preferably by a primary percutaneous coronary intervention (PCI). Aside from traditional cardiovascular risk factors which are related to atherosclerosis and hence to a heightened risk of a major coronary event, the exact trigger associated with the onset of a STEMI is not always evident.2 In the past few years, epidemiological studies have shown that some chronobiological and environmental parameters such as pollution, abrupt changes in air temperature, relative humidity, rainfall, and atmospheric pressure have been related to an increased incidence of STEMI.3–7 In Portugal, a study of two major cities showed an association between temperature fall and hospital admissions for myocardial infarction.7 Although the risk ratio of environmental triggers to the onset of myocardial infarction has been reported to be small, it exposes the entire population on a continuous and involuntary basis. By addressing its putative relationship, health authorities can be alerted regarding an expected rise in the incidence of STEMI. Since many of the robust data come from latitudes that have particular climatic features,4,8–11 there is a paucity of data regarding its impact in a temperate Mediterranean region. Furthermore, many reports capture either a broad definition of myocardial infarction,12,13 or sometimes its diagnosis comes from an administrative codification without having confirmation via PCI.13,14 This may have led to ascertainment bias. With this study, we sought to assess the impact of atmospheric parameters on the incidence of STEMI in a population who underwent PCI, attended by a tertiary care center in the city of Porto, Portugal.
MethodsStudied population and definitionsThis study is a retrospective analysis of STEMI-patients treated with primary PCI at CHUP – Centro Hospitalar Universitário do Porto – between 1 January 2010 and 31 December 2017. STEMI-patients were diagnosed after clinical and electrocardiographic criteria as explained elsewhere,15 only those who were admitted to our center and who had an angiographic lesion assessed by invasive coronariography compatible with the clinical setting were considered for analysis. Those who did not go to the hospital, died before intervention or did not undergo PCI for any reason and hence a culprit lesion was not confirmed, were excluded. All STEMI-patients treated at our center were included in a prospective anonymized database where demographic, clinical, and procedural features were registered.
Patient informed consent for the current study was waived because the records were anonymized. This study was approved by the local ethics committee (local number 223-DEFI/235-CE) and was conducted in accordance with the revised Declaration of Helsinki.
Climate characteristicsPortugal is a country in the Western Europe with a Mediterranean climate. Porto is its second biggest city with a population of approximately 1.7 million living in its metropolitan area (approximate 2000 km2). Our PCI center covers around 400 000 inhabitants without significant meteorological disparities. According to Koppen-Geiger, Porto's climate is classified as a warm-summer Mediterranean climate (Csb),16 which is characterized by a lack of mildly hot temperatures, a cold and rainy winter and fall, and a mild, hot summer and spring.
Meteorological data was obtained from the Portuguese Institute for Sea and Atmosphere I.P., a government-lead institute, from 2010 to 2017 – a total of 2922 days. Most of the data were registered in the Pedras Rubras (88.4% of days) station and the remaining at Serra do Pilar (9.3% of days) and São Gens (2.3% of days) stations. These gather the overall meteorological conditions representative of the area covered by our center. The following variables were collected: atmospheric temperature (expressed in °C) mean (Tmean), minimum (Tmin), maximum (Tmax), relative humidity (%, mean), rainfall (expressed in mm; mean), atmospheric pressure (expressed in hPa; mean). Missing values of meteorological parameters were inputted using the mean of the flanking values, with exception for precipitation. Because analysis with and without inputted missing values were similar, the analyzed data was performed after inputted missing values. Definition of seasons was used by the meteorological criteria as follows: Summer includes June, July and August months; Fall includes September, October and November; Winter includes December, January and February; Spring includes March, April and May.
Statistical analysisStatistical analysis was performed with IBM SPSS Statistics (v.26) using GLM with a Poisson distribution. For ascertaining the effect of meteorological variables, a series of models were considered for exposure at different hazard periods before the event - same day to previous seven days and the average values of two-day to seven-day period. As the individualized cases were not used, adjustment to the clinical variables from the data was not performed.
The effects (GLM coefficients) are presented as excess relative risk (ERR) for a unit drop in the temperature parameters – maximum, minimum and median temperature. The other meteorological parameters - diurnal temperature range (DTR), relative humidity, precipitation and atmospheric pressure - are presented for a unit rise. Univariate and multivariable analysis were computed to study independent parameters which predicted a higher risk of STEMI occurrence. Statistical significance was set for a two-tailed p-value <0.05, unadjusted for multiplicity.
ResultsOverall, 1004 STEMI-patients confirmed by PCI had full data available and were included in the study (mean 0.3 STEMI per day). Patients’ mean age was 62.5±12.9 years and 75% were men.
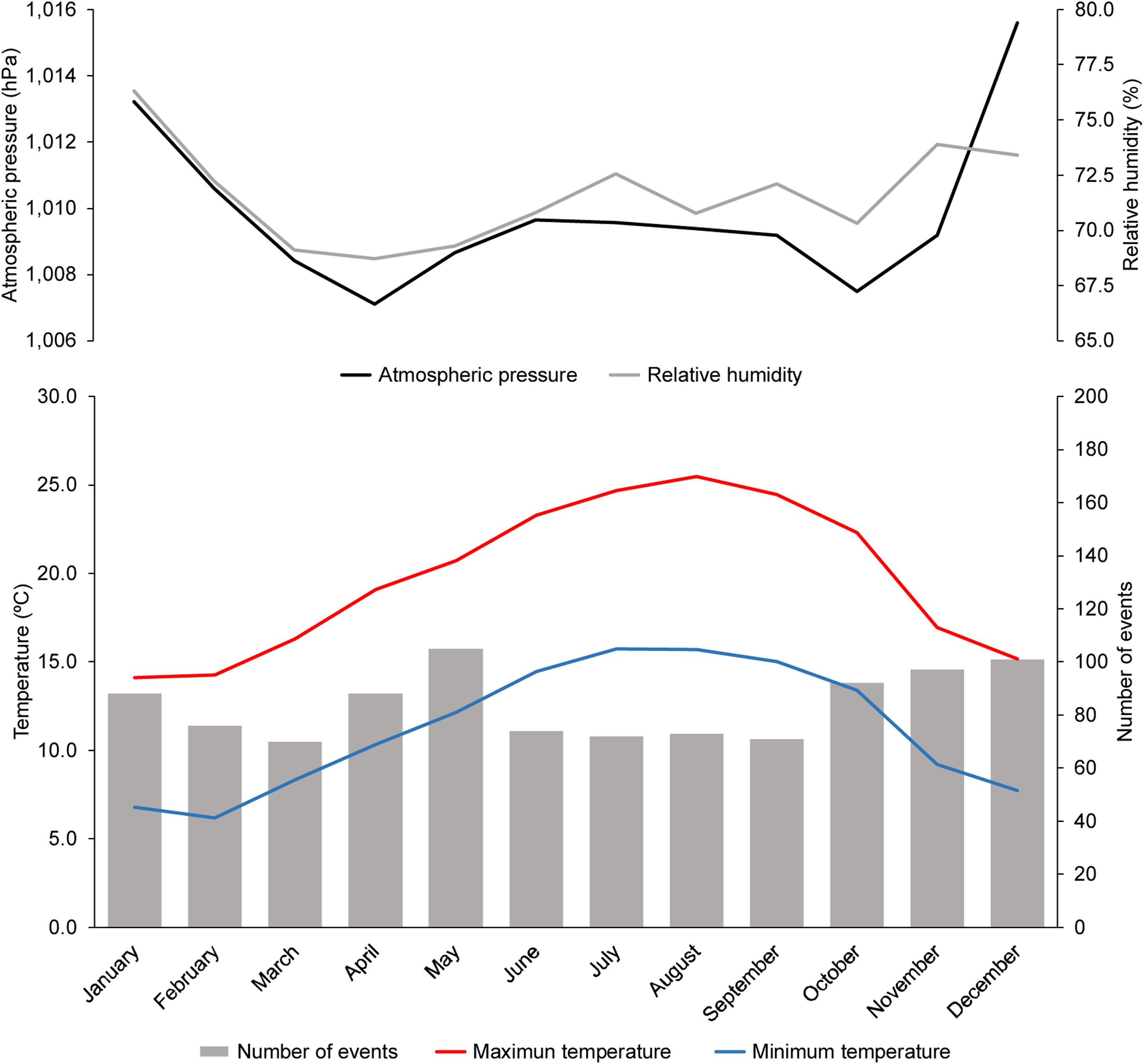
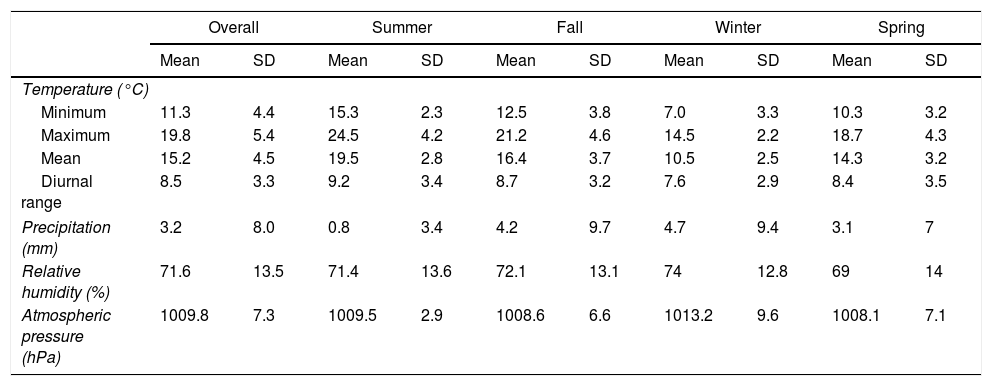
Meteorological parameters are described in Table 1. As expected, summer was the hottest season and winter the coldest. The rainiest seasons were fall and winter. Relative humidity (RH) was also higher in these seasons, whereas the atmospheric pressure was higher during the winter.
Description of weather parameters.
| Overall | Summer | Fall | Winter | Spring | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Temperature (°C) | ||||||||||
| Minimum | 11.3 | 4.4 | 15.3 | 2.3 | 12.5 | 3.8 | 7.0 | 3.3 | 10.3 | 3.2 |
| Maximum | 19.8 | 5.4 | 24.5 | 4.2 | 21.2 | 4.6 | 14.5 | 2.2 | 18.7 | 4.3 |
| Mean | 15.2 | 4.5 | 19.5 | 2.8 | 16.4 | 3.7 | 10.5 | 2.5 | 14.3 | 3.2 |
| Diurnal range | 8.5 | 3.3 | 9.2 | 3.4 | 8.7 | 3.2 | 7.6 | 2.9 | 8.4 | 3.5 |
| Precipitation (mm) | 3.2 | 8.0 | 0.8 | 3.4 | 4.2 | 9.7 | 4.7 | 9.4 | 3.1 | 7 |
| Relative humidity (%) | 71.6 | 13.5 | 71.4 | 13.6 | 72.1 | 13.1 | 74 | 12.8 | 69 | 14 |
| Atmospheric pressure (hPa) | 1009.8 | 7.3 | 1009.5 | 2.9 | 1008.6 | 6.6 | 1013.2 | 9.6 | 1008.1 | 7.1 |
Legend: SD: standard deviation.
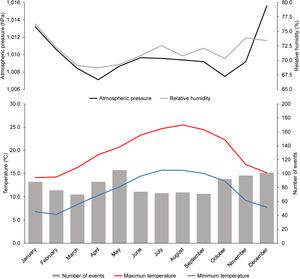
Monthly variation in temperature is depicted in Figure 1. A higher number of STEMI was appreciated from October to January, as well as in the months of April and May.
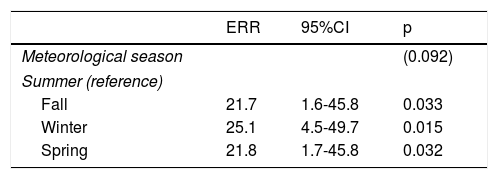
Although we did not encounter statistically significant seasonality, we observed an increased risk ratio in fall, winter and spring, as compared to summer (Table 2).
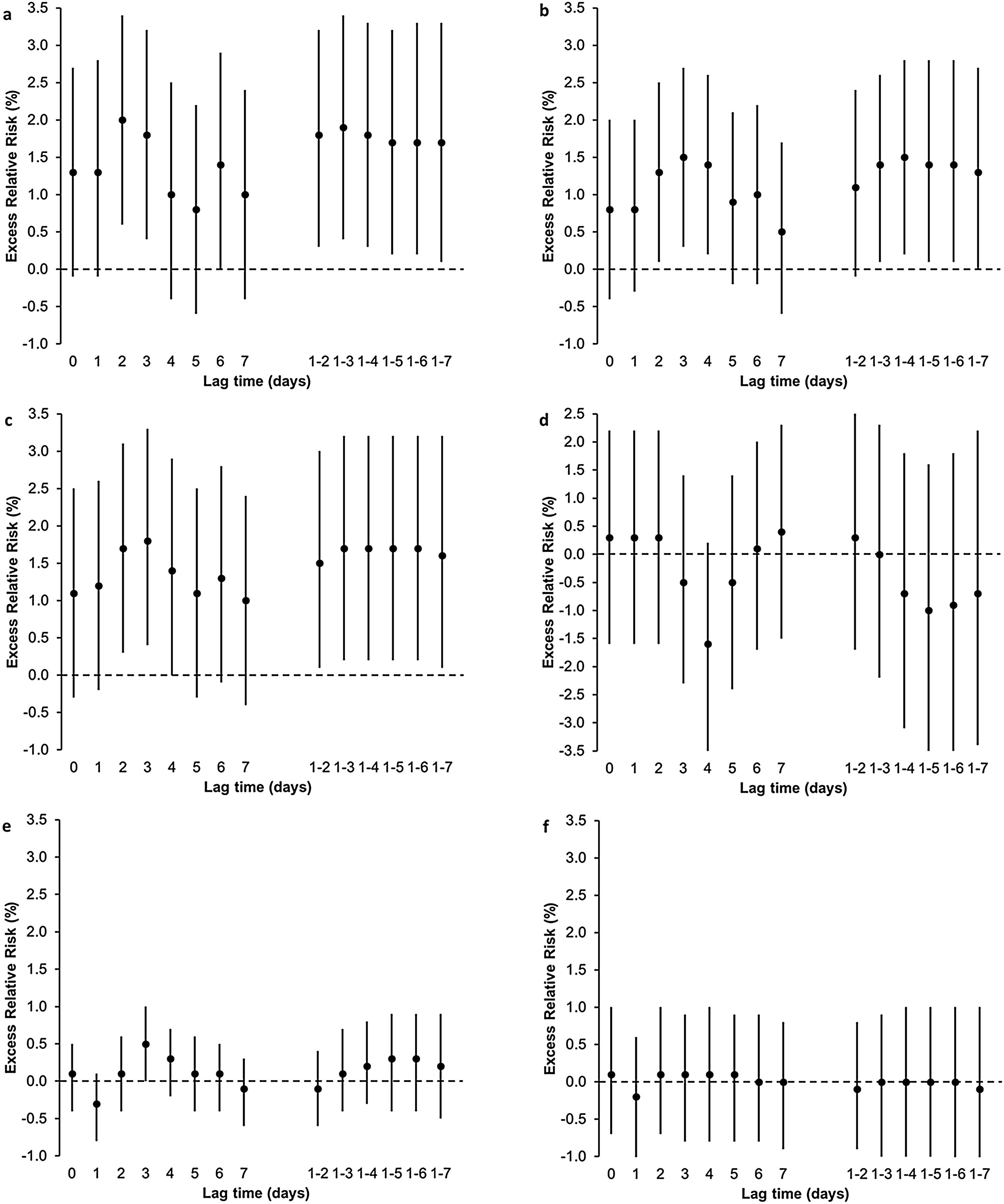
We found several associations between STEMI occurrence and different temperature parameters at different hazard periods. For a 1°C drop in minimum temperature (Tmin), at preceding two, three and six days, relative risk of STEMI increases 2.0%, 1.8% and 1.4%, respectively (Figure 2 and supplemental Table 1). A similar association was found when considering the mean values of Tmin in different hazard periods before the event (two-day to seven-day period). We also found an excess risk for each drop of 1°C in maximum temperature (Tmax) in the preceding two, three and four days before the event (ERR=1.3%, 1.5% and 1.4% respectively). We observed a similar association when considering the mean values of Tmax in different hazard periods before the event (three-day to seven-day period). Finally, a 1°C drop in Tmean in the preceding two, three and four days was associated with an increase of 1.7%, 1.8% and 1.4% in the risk of STEMI. The same association was observed with a decrease in the average values of Tmean in the days before, for all the hazard period considered: two-day to seven-day period (ERR ranging from 1.5 to 1.7%). Besides temperature, we also found that for a 1% increase in relative humidity three days before the event, the risk of STEMI increased 0.5%. We did not find any association between STEMI occurrence and diurnal temperature range, precipitation and atmospheric pressure.
Excess relative risk of ST-elevation myocardial infarction for different hazard periods before the event - same day, seven previous days and the average values for the previous seven day period - after a (a) 1°C drop in minimum temperature, (b) 1°C drop in maximum temperature, (c) 1°C drop in mean temperature, (d) 1°C increase in diurnal temperature range, (e) 1% increase in relative humidity and (f) 1 hPa increase in atmospheric pressure. Plots represent mean values and bars 95% confidence interval.
In the stepwise models, the most important predictors of STEMI occurrence are Tmin two days before the event (ERR=1.9%, 95% confidence interval (CI) 0.5 to 3.3%, p=0.009) and a 1% increase in relative humidity three days before the event (ERR=0.7%, 95%CI 0.2 to 1.3%, p=0.006) for an excess of risk, while the same increase in relative humidity one day before the event (ERR=-0.6%, 95%CI -1.1 to -0.1%, p=0.023) was associated with a lower risk.
DiscussionThe main findings of this study are as follows: (1) a drop in Tmin two days before the event is associated with a higher ERR; (2) the highest RH in the previous three days is associated with a higher ERR, whereas the highest RH one day before the event is associated with a lower ERR; (3) although seasonality was not confirmed, there is an higher relative risk in fall, winter and spring, as compared to summer; (4) diurnal temperature range, atmospheric pressure and precipitation did not show any significant impact.
Our results are aligned with most studies on this subject.5,6,12,17–21 At least three European studies (from across Belgium, Madrid, and Paris areas), which had also only included STEMI-patients undergoing PCI, showed that a drop in temperature was related to an excess risk of STEMI.6,19,21 Conversely, in another European cohort (Rome region), a higher temperature in the summer was related to an increased risk of STEMI.22 None of these regions have the same climatic characteristics as our city.
Close to our location, two studies aimed to assess the incidence of acute cardiac disease in relation to climate changes. One study came from Galicia, (Northern Spain), where some regions share the same type of climate as Northern Portugal,23 and aimed to assess the impact of daily meteorological parameters. They failed to show a relationship between daily temperature and the incidence of a myocardial infarction. The other study came from Portugal,7 encompassing data gathered from the two major cities: Lisbon (which as has a Mediterranean Csa Climate) and Porto, and investigated the impact of cold weather on the incidence of acute myocardial infarction captured from diagnosis-related groups database (Coded ICD9:410). They found that for every degree drop in temperature during the winter, there was an increase of up to 2.2% (95% CI=0.9%; 3.3%) in daily hospital admissions for myocardial infarction.
The strength of our study is twofold: first, we studied a population in a temperate Mediterranean climate living in a relatively small area without major meteorological disparities, and second, by only including patients presenting with an occluded coronary artery, as confirmed by invasive angiography, we believe the impact of climate on the incidence of an acute myocardial infarction was better ascertained. By analyzing Figure 1, a lower temperature starting in October is related to a steady rise in the number of events, which then stabilizes and diminishes in the coldest months of January to March. The same trend has been observed in other series,14,24 highlighting that it is probably temperature variation, rather than absolute seasonal low temperature that closely relates to cardiac events. This may suggest that vascular biology is more sensitive to the lowering of temperatures until it adapts. According to one systematic review,25 countries with a higher latitude have a less meaningful association between exposure to the cold and the number of events, presumably because of the adaptive physiological response to lower temperatures, but also by taking precautionary behavior against the cold.
Mechanisms that lead to these associations are multifactorial.2,3,26 One of the hypotheses is the cold-related activation of sympathetic nervous system.27 Increased levels of catecholamines lead to a higher heart rate which increases oxygen demands and also reduce the duration of diastole, creating an impediment to coronary blood flow.28 Moreover, to maintain a constant core body temperature in low temperatures, vessels constrict to suppress heat dissipation, which leads to higher blood pressure.5,29,30 This process of vasoconstriction due to cold can also alter the arterial wall shear stress and lead to plaque rupture. Nonetheless, other physiological reasons were investigated to explain this association and some studies show that colder temperatures have pro-coagulant properties which may heighten the risk of myocardial infarction.31,32 It is also plausible that the activation of the sympathetic nervous system leads to a higher production of new platelets, which are more capable of aggregating and adhering to the vessel wall, promoting thrombosis.33 Cold temperatures are also related to a higher number of respiratory infections, namely influenza, which has also been linked to a heightened risk of myocardial infarction.26 Although some studies have shown a rise in cholesterol levels in winter which could act as a cofactor, it appears that this effect may just be due to hemoconcentration, and so the absolute value of cholesterol is not different from other seasons.34 Nevertheless, it is plausible that in winter the average caloric intake is higher than in other seasons, raising the risk not only attributed to a gluco-metabolic dysregulation but also to reduced physical activity and depression.35,36
Contrary to our findings, some series showed that the incidence of STEMI is increased when there is a rise in temperature,22,37 especially in susceptible populations,38 whereas others refute any association between the incidence of STEMI and meteorological conditions. These differences may be ascribed to the latitude of the country where the study was undertaken. Similar to other reports, in our series, in the summer there was a lower relative risk compared to other seasons.7,23,26,39,40 We did also find an increased incidence of STEMI in the months from March to May. Although we do not have a simple explanation for this, it is tempting to speculate that a temperature rise may also trigger more events, as was found in some European cohorts.22,37,38 Some authors have shown that hourly exposure (six hours) to increasing ambient temperature was associated with an excess risk of a myocardial infarction.41 Since we did not capture these ultra-short variations, a positive association with increasing temperature may have been missed.
It seems that the relationship between temperature and the risk of a myocardial infarction is U-shaped, influenced by both increasing and decreasing temperature,42 followed by the observation that temperature extremes are associated with an excess in cardiac death.43
Besides temperature, this investigation also showed an excess risk of STEMI for a 1% increase in RH three days before the event. The opposite results for the same RH variation in lag three and lag one are not easy to interpret. Not only does it likely reflect imbalances in core body temperature and water homeostasis,12 but it may also reflect the effect of unknown confounders undermining a cause and effect relationship in unidimensional appraisal.44 Contradictory results have been reported, either increasing23 or decreasing9 the risk for an acute coronary event for a given increase or decrease in ambient RH. Interestingly, one study showed that the concentrations of fine-particulate matter (PM2.5) was dependent on RH, raising the water-soluble components (especially inorganic ions), the water-soluble organic carbon to organic carbon ratio, pointing to the formation of secondary organic aerosols.45 Since PM2.5 has been associated with cardiovascular risk, including myocardial infarction,46 RH may be a key factor in an increase in air pollutants such PM2.5. Finally, differences in methods to ascertain this effect may result in conflicting results.
A relation between the atmospheric pressure and the number of events was not found. This might be related to the lack of variability of this atmospheric parameter when compared to the temperature variation.36
LimitationsThere are some limitations to this study. One major limitation is that all STEMI-patients that died before treatment were not considered for analysis, thereby not considering whether climate triggers were associated with a particularly severe and a rapidly fatal outcome. Nevertheless, by only addressing those who arrived at the hospital alive and who had a confirmatory PCI, we may have reduced ascertainment bias. Another major concern, which has also been addressed in other similar studies, is that the outdoor meteorological conditions may not reflect indoor and core body temperatures. We did not measure air pollution, which has been associated with triggering myocardial infarction.47 This might have acted as a confounded factor impacting our results. Finally, we did not include the other two tertiary care hospitals in the same city, which may also have a large group of patients sharing the same atmospheric characteristics.
ConclusionsIn a contemporary series of STEMI-patients treated with primary PCI, climate had a significant association with STEMI incidence in a city without extreme meteorological variations. A higher risk is to be expected with the lower minimum temperature two days before the event, and a higher relative humidity three days before the event. Conducting a large, country-scale study to ascertain the occurrence of STEMI in accordance to atmospheric features could be of interest.
FundingUMIB is funded by Foundation for Science and Technology (FCT) Portugal (UID/Multi/00215/2019).
Conflicts of interestThe authors have no conflicts of interest to declare.