Stent restenosis remains a clinical challenge for patients with ischemic heart disease, since it is associated with repeated coronary interventions as well as higher hospitalization rates and medical costs. Inflammation plays a significant role. Although an association between stent restenosis, increased C-reactive protein (CRP) and decreased albumin levels has been previously reported, no studies have investigated the ability of the CRP/albumin ratio to predict stent restenosis.
MethodsThis retrospective study included 448 patients who had previously undergone primary percutaneous coronary intervention and who were referred for subsequent reintervention due to recurrence of anginal symptoms. The study population was divided into two groups based on whether the patient had developed stent restenosis. They were then stratified into three groups according to their CRP/albumin ratio.
ResultsOut of 448 patients, stent restenosis was observed in 24.5% (n=110), as determined by coronary angiography. Patients with stent restenosis had a higher CRP/albumin ratio, greater platelet distribution width (PDW), higher CRP levels, and lower levels of both high-density lipoprotein (HDL) cholesterol and serum albumin. The CRP/albumin ratio (OR: 2.289, 95% CI: 1.056-4.959; p=0.036), stent diameter, PDW and HDL cholesterol levels were found to be independent predictors of stent restenosis. A ROC curve comparison demonstrated that the CRP/albumin ratio was a better predictor of restenosis than either albumin and CRP individually, but it was not better than PDW and HDL cholesterol.
ConclusionAs a novel inflammation-based risk score, the CRP/albumin ratio may be an easily accessible marker for assessment of stent restenosis risk.
A reestenose de stent permanece como um desafio clínico em doentes com cardiopatia isquémica. A reestenose de stent está associada a intervenções coronárias recorrentes bem como a aumento de internamentos e de custos médicos. A inflamação tem um papel significativo. Embora a associação entre reestenose de stent e o aumento dos níveis de proteína C-reativa (PCR) e a diminuição dos níveis de albumina tenham sido previamente registados, nenhum estudo pesquisou a possibilidade da PCR/albumina prever um diagnóstico de reestenose de stent.
MétodosEste estudo retrospetivo incluiu 448 doentes que tinham sido previamente submetidos a intervenção coronária percutânea primária e que foram referidos para reintervenção posterior devido a ressurgimento dos sintomas de angina. A população do estudo foi dividida em dois grupos com base no facto do doente ter desenvolvido reestenose de stent. Posteriormente, foram estratificados em três grupos de acordo com as relações PCR/albumina.
ResultadosDe um grupo de 448 doentes, a reestenose de stent foi observada em 24,5% (n = 110), conforme determinado por avaliação através de angiografia coronária. Os doentes com reestenose de stent apresentaram uma relação PCR/albumina mais elevada, variação maior do diâmetro das plaquetas (DP), níveis mais elevados de PCR e níveis mais baixos de colesterol de lipoproteínas de alta densidade (HDL) e de albumina sérica. Os níveis da relação PCR/albumina (OR: 2,289, IC 95%:1,056 – 4,959; p = 0,036), o diâmetro do stent, a variação maior do DP e o colesterol HDL foram considerados fatores preditores independentes da restenose de stent. A comparação das curvas ROC demonstrou que a relação PCR/albumina constituiu um fator preditor melhor do que a albumina e a PCR, isoladamente, não sendo, no entanto, melhor do que o DP e o colesterol HDL.
ConclusãoComo novo score de risco baseado em inflamação, a relação PCR/albumina pode ser um marcador facilmente acessível para a avaliação do risco de reestenose de stent.
Deaths from ischemic heart disease have decreased in recent years due to increased use of percutaneous coronary intervention (PCI). Primary PCI (pPCI) is generally the first line of treatment for patients with ST-segment elevation myocardial infarction (STEMI), and stenting is recommended over balloon angioplasty.1 However, restenosis, a gradual re-narrowing of the stented segment, continues to be a clinical challenge. Stent restenosis decreases the patient's quality of life and is associated with repeated coronary interventions as well as higher hospitalization rates and medical costs.2–4
Stent restenosis is a complex and multifactorial process that begins with stent deployment in the coronary artery.5 Inflammation plays a key role in arterial damage after stent placement, accelerating macrophage accumulation and neovascularization. The inflammation process also leads to neointimal tissue proliferation, thrombus formation at the stent struts and activation of neutrophils, fibrin and platelets, all of which result in stent restenosis.6,7 Studies on stent-induced inflammation have found a significant association between C-reactive protein (CRP) and stent restenosis.5,8,9 An acute phase protein that is released from the liver, CRP is a useful marker for objectively stratifying an active inflammation process. Similarly, serum albumin is a negative acute phase protein in acute inflammation and has been shown to have an inverse relationship with stent restenosis.10
The CRP/albumin ratio has been identified as an inflammation-based prognostic marker and is considered to reflect the relationship between CRP and albumin levels in determining the prognosis of critical diseases and malignancy.11,12 The fact that the CRP/albumin ratio is a good indicator of inflammatory status led us to investigate its relationship with stent restenosis. In this study, we aimed to assess whether the CRP/albumin ratio and levels of CRP and albumin at the time of initial pPCI are associated with subsequent stent restenosis in STEMI patients who were treated with bare-metal stents (BMS).
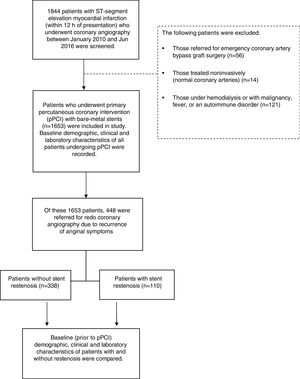
MethodsStudy populationBetween January 2010 and June 2016, 1844 STEMI patients were referred for coronary angiography and pPCI, and these formed the basis of our study population. Of these, 191 were excluded from the study: those referred for emergency coronary artery bypass graft surgery, those treated noninvasively, those under hemodialysis, and those with malignancy, fever or an autoimmune disorder. Of the remaining 1653 patients, 448 were referred for redo coronary angiography due to recurrence of anginal symptoms and were therefore included in this retrospective study (Figure 1). The first STEMI was defined based on the following criteria: a typical increase or decrease in cardiac biomarkers; ongoing ischemic symptoms (within 12 hours of presentation); newly developed left bundle branch block pattern or new ST elevation in two or more contiguous leads, with readings of at least 0.2 mV in leads V1, V2 and V3 or at least 0.1 mV in the other leads; or imaging evidence of a new loss of viable myocardium or new regional wall motion abnormality.13 Stent restenosis was defined as the presence of clinical symptoms and/or signs of ischemia and at least 50% narrowing in lumen diameter at follow-up angiography.14
The study protocol was reviewed and approved by the local ethics committee of Kafkas University and was conducted in accordance with the Declaration of Helsinki.
Data collectionAll patients who were referred for coronary reintervention due to recurrence of ischemic symptoms were hospitalized. To establish the effects of the first pPCI on subsequent stent restenosis, patients’ baseline clinical, demographic, biochemical and hematological characteristics at the time of the first pPCI were recorded. Complete blood count and blood biochemical parameters were assessed in all patients on admission and prior to pPCI. CRP and serum albumin levels were determined using an automatic biochemical analyzer (Cobas 8000 c502, Roche Diagnostics). The CRP/albumin ratio was calculated as the ratio of CRP to albumin multiplied by 10 for ease of interpretation. The neutrophil/lymphocyte ratio was calculated from the complete blood count obtained on admission. Blood samples were retested for creatine kinase-myocardial band (CK-MB) every six hours until peak levels were identified. The estimated glomerular filtration rate (eGFR) was determined using the Cockcroft-Gault formula from the blood samples obtained on admission. Left ventricular ejection fraction (LVEF) was defined as the postprocedural ejection fraction and was assessed using a modified version of Simpson's method.
Angiographic analysisThe standard Judkins percutaneous transfemoral technique was performed by experienced interventional cardiologists on all patients who underwent pPCI. Coronary angiograms and pPCIs were recorded using digital media (DICOM viewer, MedCom GmbH, Darmstadt, Germany). The digital angiography and PCI records of all patients who were admitted with STEMI and underwent BMS implantation (the records of the first angiography) were analyzed quantitatively in terms of lesion and intervention characteristics. Coronary blood flow patterns before and after pPCI were assessed using Thrombolysis in Myocardial Infarction (TIMI) flow grade as defined previously, and epicardial no-reflow was defined as TIMI flow grade <3 at the target vessel lesion in the absence of spasm, thrombus, dissection and/or significant residual stenosis.15 Similarly, thrombus burden was assessed according to the TIMI thrombus grading scale as defined by Gibson et al.15 The sizes of the stents used in the interventions were confirmed from hospital records. All patients had received 300 mg aspirin and a 600-mg loading dose of clopidogrel on a routine basis before the intervention and received unfractionated heparin during the intervention. The decision whether to use tirofiban was left to the operator's discretion.
Statistical analysisThe statistical analysis was performed using IBM SPSS version 22.0 (IBM SPSS Inc., Chicago, IL). The normality of the data was determined using the Kolmogorov-Smirnov test. With respect to data distribution and normality, continuous variables were expressed as mean ± standard deviation or median [interquartile range] (25th-75th percentiles), and the t test or Mann-Whitney U-test was conducted to compare variables between two groups. Continuous variables with and without normal distribution were compared between three groups using analysis of variance and the Kruskal-Wallis H-test, respectively. Categorical variables were presented as numbers (percentages) and compared using Fisher's exact test or the chi-square test. Multivariate logistic regression analysis was performed to identify independent predictors of stent restenosis using variables that showed a statistically significant association with stent restenosis in univariate analysis. Multicollinearity between the CRP/albumin ratio and CRP and albumin levels was assessed by eigenvalues and condition indices. Linearity was tested following the logarithmic transformation of each parameter. A receiver operating characteristic (ROC) curve was used to derive the best cut-off value of the CRP/albumin ratio for predicting stent restenosis using Youden's J statistic. A p-value <0.05 was taken to indicate statistical significance.
ResultsThe study population consisted of 448 patients who underwent repeat coronary intervention (mean age 56±11 years; 17.8% female). The mean interval between coronary reintervention and the first STEMI was 21.07±3.89 months. Stent restenosis was observed in 24.5% (n=110) of the study population who underwent a second coronary angiography. The baseline clinical and angiographic characteristics of the total population and of patients with and without stent restenosis are shown in Table 1. Patients with stent restenosis had a higher CRP/albumin ratio, more frequent involvement of the left anterior descending artery (LAD), greater platelet distribution width (PDW), higher CRP levels, and lower levels of both high-density lipoprotein (HDL) cholesterol and serum albumin, compared to those without stent restenosis. Furthermore, patients with stent restenosis had higher thrombus burden, greater stent length and smaller angiographic reference lumen diameter, and had more frequently received tirofiban infusion at the time of the first pPCI. There was no difference between the two groups in terms of preprocedural TIMI flow (Table 1).
Demographic, clinical and laboratory characteristics of the total study population and of patients with and without restenosis.
| Total population (n=448) | Patients without SR (n=338) | Patients with SR (n=110) | p | |
|---|---|---|---|---|
| Age, years | 56±11 | 56±11 | 57±12 | 0.209 |
| Female, n (%) | 81.0 (18.10) | 60.0 (17.80) | 21.0 (19.10) | 0.751 |
| Diabetes, n (%) | 102.0 (22.80) | 73.0 (21.60) | 29.0 (26.40) | 0.301 |
| Hypertension, n (%) | 180.0 (40.20) | 132.0 (39.10) | 48.0 (43.60) | 0.395 |
| Hyperlipidemia, n (%) | 184.0 (41.10) | 132.0 (39.10) | 52.0 (47.30) | 0.128 |
| Smoking, n (%) | 245.0 (54.70) | 180.0 (53.30) | 65.0 (59.10) | 0.286 |
| LVEF, % | 47.51±7.49 | 47.71±7.42 | 46.94±7.71 | 0.208 |
| Total ischemia time, min, median [IQR] | 173.5 [117.0-256.5] | 174.0 [118.0-245.0] | 168.5 [110.0-262.0] | 0.779 |
| IRA, n (%) | ||||
| LAD | 231.0 (51.60) | 170.0 (50.30) | 61.0 (55.50) | 0.032 |
| RCA | 165.0 (36.80) | 133.0 (39.30) | 32.0 (29.10) | |
| CX | 52.0 (11.60) | 35.0 (10.40) | 17.0 (15.50) | |
| Proximal/ostial lesion as IRA, n (%) | 255.0 (56.90) | 192.0 (56.80) | 63.0 (57.30) | 0.931 |
| High-grade thrombus burden, n (%) | 237.0 (52.90) | 168.0 (49.70) | 69.0 (62.70) | 0.017 |
| Pre-dilatation, n (%) | 358.0 (79.90) | 267.0 (79.00) | 91.0 (82.70) | 0.397 |
| Tirofiban infusion n (%) | 186.0 (41.50) | 127.0 (37.60) | 59.0 (53.60) | 0.003 |
| Stent length, mm | 22.24±9.65 | 21.97±9.80 | 23.06±9.16 | 0.029 |
| Stent diameter, mm | 3.10±0.37 | 3.13±0.37 | 3.01±0.35 | 0.009 |
| Post-dilatation, n (%) | 112.0 (25.00) | 86.0 (25.40) | 26.0 (23.60) | 0.704 |
| No-reflow, n (%) | 44.0 (9.80) | 30.0 (8.90) | 14.0 (12.70) | 0.239 |
| Time from first STEMI to reintervention, months | 21.07±3.89 | 22.31±2.62 | 17.25±4.60 | |
| Hemoglobin, g/dl | 13.8±1.7 | 13.7±1.8 | 13.8±1.4 | 0.533 |
| WBC count, /1000 | 12.032±3.552 | 12.151±3.650 | 11.665±3.221 | 0.322 |
| Platelet count, 10 000/ml | 254±62 | 254±63 | 254±60 | 0.876 |
| Mean platelet volume, fl | 9.3±1.3 | 9.3±1.2 | 9.2±1.4 | 0.337 |
| PDW, % | 16.20±1.37 | 16.11±1.34 | 16.48±1.42 | 0.001 |
| Neutrophil count, /1000 | 9.168±3.313 | 9.252±3.403 | 8.912±3.017 | 0.483 |
| Lymphocyte count, /1000, median [IQR] | 1.800 [1.30-2.50] | 1.800 [1.30-2.50] | 1.700 [1.30-2.50] | 0.648 |
| Neutrophil-to-lymphocyte ratio, median [IQR] | 4.80 [3.20-7.26] | 4.85 [3.24-7.23] | 4.69 [3.14-7.36] | 0.984 |
| Total cholesterol, mg/dl | 178.81±43.03 | 180.88±43.92 | 172.17±39.52 | 0.082 |
| LDL-C, mg/dl | 111.55±35.82 | 112.31±36.12 | 109.13±34.90 | 0.336 |
| HDL-C, mg/dl | 40.25±12.51 | 41.20±12.63 | 37.20±11.67 | 0.002 |
| Triglycerides, mg/dl, median [IQR] | 121.00 [87.0-168.5] | 123.00 [88.0-171.0] | 115.00 [76.0-167.0] | 0.172 |
| Glucose on admission, mg/dl, median [IQR] | 126.00 [105.5-168.5] | 125.00 [103.0-170.0] | 133.50 [110.0-165.0] | 0.110 |
| eGFR, ml/min/1.73 m2 | 91.62±24.31 | 92.25±24.83 | 89.67±22.65 | 0.179 |
| CRP, mg/dl, median [IQR] | 9.26 [5.34-16.45] | 8.86 [4.78-15.40] | 11.00 [6.75-18.70] | 0.009 |
| Serum albumin, g/dl | 3.86±0.47 | 3.89±0.48 | 3.77±0.43 | 0.006 |
| Total protein, g/dl | 6.67±0.62 | 6.69±0.63 | 6.62±0.61 | 0.546 |
| CRP/albumin ratio, median [IQR] | 0.258 [0.139-0.421] | 0.237 [0.117-0.39] | 0.300 [0.182-0.51] | 0.003 |
| Baseline uric acid, mg/dl | 5.06±1.40 | 5.10±1.40 | 4.92±1.40 | 0.195 |
| Peak CK-MB, ng/ml, median [IQR] | 167.00 [97.0-303.0] | 170.50 [99.0-303.0] | 149.00 [90.0-301.0] | 0.774 |
CK-MB: creatine kinase-myocardial band; CRP: C-reactive protein; CX: circumflex artery; eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; IQR: interquartile range (25th-75th percentiles); IRA: infarct-related artery; LAD: left anterior descending artery; LDL-C: low-density lipoprotein cholesterol; LVEF: left ventricular ejection fraction; PDW: platelet distribution width; RCA: right coronary artery; SR: stent restenosis; STEMI: ST-segment elevation myocardial infarction; WBC: white blood cell.
Multivariate regression analysis was used to determine the independent predictors of stent restenosis using the parameters that were associated with stent restenosis in univariate analysis. The CRP/albumin ratio (odds ratio [OR]: 2.289, 95% confidence interval [CI]: 1.056-4.959; p=0.036), stent diameter (per 1 mm, OR: 0.370, 95% CI: 0.180-0.760; p=0.007), PDW (per 1 percent, OR: 1.247, 95% CI: 1.023-1.522; p=0.029), and HDL cholesterol (OR: 0.973, 95% CI: 0.952-0.994; p=0.014) were found to be independent predictors of stent restenosis (Table 2).
Univariate and multivariate logistic regression analysis of demographic, clinical, laboratory and coronary angiographic characteristics for prediction of restenosis.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Stent diameter (per 1 mm) | 0.401 | 0.210-0.764 | 0.005 | 0.370 | 0.180-0.760 | 0.007 |
| PDW (per 1 percent) | 1.252 | 1.041-1.506 | 0.017 | 1.247 | 1.023-1.522 | 0.029 |
| HDL-C (mg/dl) | 1.252 | 1.041-1.506 | 0.017 | 0.973 | 0.952-0.994 | 0.014 |
| CRP/albumin ratio | 2.539 | 1.285-5.016 | 0.007 | 2.289 | 1.056-4.959 | 0.036 |
CI: confidence interval; CRP: C-reactive protein; HDL-C: high-density lipoprotein cholesterol; OR: odds ratio; PDW: platelet distribution width.
The variables included in the multivariate analysis were infarct-related artery, high-grade thrombus burden, stent length, stent diameter, PDW, HDL cholesterol and CRP/albumin ratio.
Because no specific cut-off was identified for the CRP/albumin ratio, subjects who underwent repeat coronary angiography were stratified into three groups according to CRP/albumin ratio by equalizing the number of patients: tertile 1 (<0.170, n=149), tertile 2 (0.170-0.363, n=150) and tertile 3 (>0.363, n=149). There were significant differences between these tertiles. Mean CRP level, age, frequency of hypertension, total ischemia time, peak CK-MB, incidence of proximal coronary lesion involvement, LAD involvement as the infarct-related artery, and presence of no-reflow increased progressively from tertile 1 to tertile 3, while LVEF and albumin levels decreased progressively (Table 3). It was also observed that stent restenosis increased progressively with the tertiles’ increasing CRP/albumin ratio (Table 3).
Demographic, clinical, laboratory and coronary angiographic characteristics of the study population stratified according to C-reactive protein/albumin ratio.
| CRP/albumin ratio | ||||
|---|---|---|---|---|
| <0.170 (n=149) | 0.170-0.363 (n=150) | >0.363 (n=149) | p | |
| Age | 54±11 | 56±11 | 59±12 | 0.002 |
| Female, n (%) | 24.0 (16.10) | 23.0 (15.30) | 34.0 (22.80) | 0.182 |
| Diabetes, n (%) | 34.0 (22.80) | 33.0 (22.00) | 35.0 (23.50) | 0.954 |
| Hypertension, n (%) | 48.0 (32.20) | 58.0 (38.70) | 74.0 (49.70) | 0.008 |
| Hyperlipidemia, n (%) | 59.0 (39.60) | 68.0 (45.30) | 57.0 (38.30) | 0.418 |
| Smoking, n (%) | 77.0 (51.70) | 88.0 (58.70) | 80.0 (53.70) | 0.459 |
| LVEF, % | 49.85±6.45 | 48.21±6.65 | 44.43±8.25 | <0.001 |
| Total ischemia time, min, median [IQR] | 145.0 [112.0-223.0] | 168.5 [105.0-235.0] | 190.0 [137.0-308.0] | <0.001 |
| IRA, n (%) | ||||
| LAD | 65.0 (43.60) | 78.0 (52.00) | 88.0 (59.10) | 0.044 |
| RCA | 66.0 (44.30) | 57.0 (38.00) | 42.0 (28.20) | |
| CX | 18.0 (12.10) | 15.0 (10.00) | 19.0 (12.80) | |
| Proximal/ostial lesion for IRA, n (%) | 73.0 (49.00) | 85.0 (56.70) | 97.0 (65.10) | 0.020 |
| High-grade thrombus burden, n (%) | 90.0 (60.40) | 97.0 (64.70) | 100.0 (67.10) | 0.475 |
| Pre-dilatation, n (%) | 116.0 (77.90) | 117.0 (78.00) | 125.0 (83.90) | 0.333 |
| Tirofiban infusion, n (%) | 61.0 (40.90) | 64.0 (42.70) | 61.0 (40.90) | 0.941 |
| Stent length, mm | 22.50±11.22 | 22.16±8.76 | 22.06±8.83 | 0.999 |
| Stent diameter, mm | 3.13±0.35 | 3.09±0.40 | 3.08±0.36 | 0.216 |
| Post-dilatation, n (%) | 31.0 (20.80) | 44.0 (29.30) | 37.0 (24.80) | 0.235 |
| No-reflow, n (%) | 6.0 (4.00) | 14.0 (9.30) | 24.0 (16.10) | 0.002 |
| Time from first STEMI to reintervention (months) | 21.38±2.98 | 21.00±3.97 | 20.82±4.55 | |
| Hemoglobin, g/dl | 13.6±1.8 | 13.8±1.6 | 13.8±1.7 | 0.867 |
| WBC count, /1000 | 11.737±3.373 | 12.046±3.339 | 12.312±3.917 | 0.428 |
| Platelet count, 10 000/ml | 255±61 | 250±61 | 257±65 | 0.599 |
| Mean platelet volume, fl | 9.1±1.2 | 9.3±1.3 | 9.3±1.4 | 0.458 |
| PDW, % | 16.22±1.22 | 16.34±1.39 | 16.05±1.47 | 0.747 |
| Neutrophil count, /1000 | 8.914±3.041 | 9.223±3.078 | 9.368±3.774 | 0.579 |
| Lymphocyte count, /1000, median [IQR] | 1.700 [1.20-2.50] | 1.800 [1.30-2.40] | 1.800 [1.40-2.60] | 0.358 |
| Neutrophil-to-lymphocyte ratio, median [IQR] | 5.00 [3.16-7.82] | 4.76 [3.59-7.21] | 4.65 [2.99-7.06] | 0.730 |
| Total cholesterol, mg/dl | 177.04±41.82 | 182.73±43.21 | 176.61±44.08 | 0.313 |
| LDL-C, mg/dl | 109.01±34.43 | 117.01±35.81 | 108.56±36.81 | 0.107 |
| HDL-C, mg/dl | 41.24±13.46 | 39.42±11.74 | 40.08±12.30 | 0.756 |
| Triglycerides, mg/dl, median [IQR] | 120.00 [85.0-183.5] | 124.00 [86.0-159.0] | 119.0 [88.0-158.0] | 0.939 |
| Glucose on admission, mg/dl, median [IQR] | 126.00 [103.0-167.0] | 124.00 [103.0-168.0] | 133.00 [109.0-169.0] | 0.323 |
| eGFR, ml/min/1.73 m2 | 95.96±26.34 | 90.93±23.18 | 87.97±22.74 | 0.029 |
| CRP, mg/dl, median [IQR] | 4.070 [2.88-5.33] | 9.265 [7.70-12.10] | 20.50 [16.40-24.50] | <0.001 |
| Serum albumin, g/dl | 3.95±0.52 | 3.83±0.42 | 3.80±0.47 | 0.013 |
| Total protein, g/dl | 6.70±0.61 | 6.66±0.61 | 6.65±0.66 | 0.799 |
| CRP/albumin ratio, median [IQR] | 0.106 [0.073-0.14] | 0.258 [0.204-0.31] | 0.518 [0.422-0.69] | <0.001 |
| Baseline uric acid, mg/dl | 4.87±1.32 | 5.12±1.36 | 5.17±1.50 | 0.202 |
| Peak CK-MB, ng/ml, median [IQR] | 122.00 [82.0-218.0] | 160.5 [102.0-289.0] | 234.0 [120.0-373.0] | <0.001 |
| Stent restenosis, n (%) | 24.0 (16.10) | 41.0 (27.3) | 45.0 (30.2) | 0.010 |
CK-MB: creatine kinase-myocardial band; CRP: C-reactive protein; CX: circumflex artery; eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; IQR: interquartile range (25th-75th percentiles); IRA: infarct-related artery; LAD: left anterior descending artery; LDL-C: low-density lipoprotein cholesterol; LVEF: left ventricular ejection fraction; PDW: platelet distribution width; RCA: right coronary artery; STEMI: ST-segment elevation myocardial infarction; WBC: white blood cell.
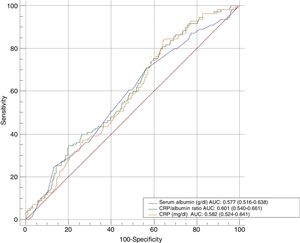
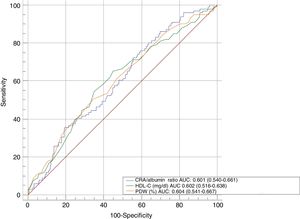
In ROC curve analysis, the area under the curve (AUC) of the CRP/albumin ratio was 0.601 (95% CI: 0.540-0.661; p<0.001). The cut-off value for the CRP/albumin ratio that indicated stent restenosis was 0.167 (with 80.9% sensitivity and 36.1% specificity). ROC curve comparisons were used to determine which variables best predicted stent restenosis. The CRP/albumin ratio was a better predictor than both serum albumin (AUC: 0.577, 95% CI: 0.516-0.638) and CRP (AUC: 0.582, 95% CI: 0.524-0.641) (p=0.050 and p=0.008, respectively) (Figure 2), but there was no significant difference between CRP/albumin ratio and PDW (AUC: 0.604, 95% CI 0.541-0.667) and HDL cholesterol (AUC: 0.602, 95% CI: 0.538-0.665) (p=0.942 and p=0.961, respectively) (Figure 3).
Our study demonstrated that the CRP/albumin ratio was not only associated with, but was also an independent predictor of stent restenosis in STEMI patients undergoing pPCI. The CRP/albumin ratio was better than both CRP and serum albumin levels, individually, in predicting stent restenosis.
pPCI is the standard treatment for patients with STEMI. Compared with balloon angioplasty alone, stenting with a BMS is associated with a lower risk of reinfarction and target vessel revascularization.1 However, with a restenosis rate of 12.7% with drug-eluting stents (DES) and 20.1% with BMS, stent restenosis remains a major concern for the management of STEMI in patients treated with pPCI.16 In our study, stent restenosis was observed in 24.5% of patients who were referred for repeat coronary angiography.
The etiology of stent restenosis is complex and multifactorial. Several risk factors have been identified, including angiographic, clinical and technical factors. Consistent with the results of previous studies, patients with stent restenosis in our study had longer stents and smaller stent lumen diameter,17 higher CRP levels,5,8,9 and lower levels of HDL cholesterol18 and serum albumin.10 Additionally, the CRP/albumin ratio was significantly higher and PDW was greater in patients with restenosis than in those without.
Inflammation plays a central role in stent restenosis. It has been previously established in animal models that there is a significant correlation between the severity of arterial inflammation and neointimal hyperplasia following balloon angioplasty and stenting.19,20 The local inflammatory reaction induced by the trauma of stenting leads to the release of cytokines and growth factors from macrophages and smooth muscle cells, resulting in a proliferative response.21 More importantly, higher baseline levels of acute-phase proteins indicate the hyper-responsiveness of inflammatory cells to any inflammatory stimuli.22 Hence, higher systemic CRP levels or lower serum albumin levels identify patients with an enhanced inflammatory response in the vessel wall to the inflammatory stimulus of stenting. In our study, baseline CRP levels were higher and serum albumin levels were significantly lower in patients with stent restenosis. These findings strongly suggest that baseline inflammatory status is a determining factor in the development of stent restenosis, in addition to the classical etiological factors.
We found that the baseline inflammatory response was exacerbated in patients with restenosis. We also observed that patients’ baseline inflammatory status was related to factors associated with a larger infarct area, including LAD involvement as the culprit lesion, no-reflow, prolonged total ischemia time and elevated peak CK-MB levels. Acute myocardial infarction triggers an inflammatory response that lasts for weeks and months, and this mid-term inflammatory response seems to be more severe in patients with large infarcts and high baseline inflammation.23 However, an increased baseline inflammatory response in patients with restenosis cannot be explained by infarct size alone. Our patients with increased CRP/albumin ratios were older and more frequently had a history of hypertension in addition to reduced eGFR and LVEF. Chronic renal insufficiency has been associated with background inflammation,24 and there is a consistent correlation between heart failure (lower LVEF) and inflammation.25 In addition, aging is accompanied by two- to four-fold increases in the plasma/serum levels of inflammatory mediators such as cytokines and acute phase proteins.26 Hypertension is also clearly associated with chronic mild inflammation.27 Although not all these factors were found to be individually associated with stent restenosis in our study, their cumulative effect might have contributed to an association between the CRP/albumin ratio and restenosis.
The various acute phase reactants may not all respond to inflammatory events to the same degree. Merging albumin and CRP into a single index as an inflammation-based prognostic score provides stability between fluctuating CRP and albumin levels in diseases where inflammation plays an important role. The CRP/albumin ratio has been used as a parameter of inflammatory status in many studies.11,12,28,29 Consistent with previous findings, the present study showed that the CRP/albumin ratio was a better predictor of stent restenosis than either CRP or albumin, individually, in ROC curve analysis.
Interestingly, the present study found PDW to be an independent predictor of stent restenosis. PDW indicates variability in platelet size, which is directly related to platelet density and reactivity in circulating platelets. Changes in these variables play an important role in the development of acute coronary syndrome.30 Recently, it has been shown that PDW is associated with acute stent thrombosis31 and is an independent predictor of no-reflow and in-hospital major cardiac adverse events32 in STEMI patients. In this study, for the first time, we demonstrated that PDW is an independent predictor of stent restenosis.
In addition to inflammation-induced neointimal hyperplasia and vascular remodeling, oxidative stress and increased vascular levels of reactive oxygen species are also thought to be involved in the pathophysiology of stent restenosis.33,34 HDL cholesterol molecules reduce macrophage accumulation, promote removal of oxidized cholesterol from the arterial wall, and can inhibit monocyte activation, adhesiveness and inflammation.35–37 Previous studies have shown that lower HDL levels are an independent risk factor for stent restenosis in different patient groups.38–40 Our study also showed that HDL cholesterol is an independent predictor of stent restenosis. A comparison of the ROC curves showed that CRP/albumin ratio, PDW and HDL cholesterol levels were not inferior to each other in predicting stent restenosis.
LimitationsThe present study has several limitations. First, although the data were acquired prospectively, the study had a retrospective design and was based on a registry analysis. Second, this study provided information about stent restenosis in STEMI patients treated with BMS; it did not include information on patients treated with DES, which currently are widely used. Third, high-sensitivity CRP, which has proven efficacy in demonstrating endovascular inflammation, could not be used in our study, due to the lack of this information in our subjects’ patient records. Finally, the prognostic value of the CRP/albumin ratio could not be assessed in the present study. Stent restenosis and patient prognosis may not necessarily correlate; therefore, the prognostic value of the CRP/albumin ratio in the development of stent restenosis should be verified by further research.
ConclusionThis study suggests that baseline inflammatory status appears to be a significant factor in subsequent stent restenosis in STEMI patients. Based on the evidence that the CRP/albumin ratio is a better predictor than CRP or albumin, individually, assessment of a patient's preprocedural CRP/albumin ratio could be beneficial. In STEMI patients, a high CRP/albumin ratio on admission may be an early, mid- and long-term marker of inflammation that could lead to stent restenosis. Although this study only analyzed restenosis with BMS, which does not correspond to the majority of stents currently used in developed countries, the mechanisms underlying stent restenosis may be common to other types of stents, and this research may be a bridge to DES studies. Additionally, for the first time, PDW has been found to be an independent predictor of stent restenosis. Therefore, PDW may be another easily accessible marker for the risk assessment of stent restenosis.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
Conflicts of interestThe authors have no conflicts of interest to declare
The authors thank www.metastata.com for their contributions to the statistical analysis and trial design.