Transcatheter aortic valve implantation (TAVI) is an emerging minimally invasive treatment modality in high surgical risk or inoperable patients.
AimThe aim of this study was to ascertain the effect of TAVI on left ventricular (LV) systolic and diastolic function and serum B-type natriuretic peptide (BNP) levels in high surgical risk or inoperable patients with severe aortic stenosis.
MethodsFifty-five patients were included in our retrospective study. LV systolic and diastolic function was assessed with conventional and tissue Doppler imaging (TDI) prior to and after TAVI. Additionally, BNP was measured 24 h before and three months after the procedure. Echocardiographic controls were performed at one, three and six months and one year and mean values were taken. At the end of the study, LV systolic and diastolic function, serum BNP levels and New York Heart Association functional capacity were assessed and compared to baseline parameters.
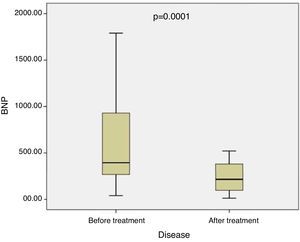
ResultsThe TAVI procedure was successful in all patients. In-hospital mortality was 1.8% (one patient). There was a substantial improvement in LV function and functional capacity at follow-up. In addition, a statistically significant decrease was detected in serum BNP levels post-TAVI (median 380 pg/ml [176.6-929.3] vs. 215 pg/ml [96.0-383.0], p=0.0001). Only one patient required a permanent pacemaker (1.8%) and there was no mortality after TAVI during follow-up. There were significant increases in LV ejection fraction and aortic valve area (51.0±13.1% vs. 58.4±9.1%, p<0.001, and 0.6±0.1 cm2 vs. 2.1±0.2 cm2, p=0.0001, respectively). At the end of the study, conventional Doppler echocardiography revealed improvement in diastolic function, with an increase in mitral E wave, a decrease in mitral A wave and an increase in E/A ratio. Deceleration time and isovolumetric relaxation time were shortened and myocardial performance (Tei) index decreased. TDI showed an increase in systolic myocardial velocity (Sm) and early diastolic velocity (Em). Septal mitral annular Sm and Em were increased, whereas MPI was reduced.
ConclusionWe found that LV structural changes and diastolic dysfunction occur in patients with severe aortic stenosis and that TAVI is able to reverse these abnormalities, which we demonstrated by both conventional echocardiography and TDI. In addition, serum BNP levels were decreased after TAVI.
A implantação de válvula aórtica por via percutânea (VAP) é uma terapêutica minimamente invasiva e de uso crescente em doentes inoperáveis ou de alto risco cirúrgico.
ObjetivoO objetivo deste estudo foi avaliar o efeito da implantação de VAP nas funções sistólica e diastólica do ventrículo esquerdo, e nos níveis plasmáticos do peptídeo natriurético tipo B (BNP), em doentes com estenose aórtica grave considerados inoperáveis ou de alto risco cirúrgico.
MétodosEstudo restrospetivo em que foram incluídos 55 doentes. As funções sitólica e diastólica do ventrículo esquerdo foram determinadas por ecocardiografia Doppler convencional e tecidular, antes e após implantação de VAP. Os níveis de BNP foram medidos 24h antes e três meses após o procedimento. Foram efetuadas reavaliações ecocardiográficas aos um, três, seis e 12 meses. No final do estudo foram avaliadas as funções sitólica e diastólica do ventrículo esquerdo, os níveis plasmáticos do BNP e a classe funcional pela classificação da New York Heart Association (NYHA), e efetuada a comparação com os valores basais.
ResultadosA VAP foi implantada com sucesso em todos os doentes. A mortalidade intra-hospitalar foi de 1,8% (n=1). Documentou-se uma melhoria substancial na função ventricular esquerda e da capacidade funcional no follow-up. Observou-se uma redução estatisticamente significativa dos níveis plasmáticos de BNP após VAP (mediana: 380 [176,6 – 929,3] pg/mL versus 215 [96,0 – 383,0] pg/mL, p=0,0001). Foi necessária a implantação de pacemaker permanente em apenas um doente (1,8%) e não houve mais mortes durante o follow-up. Observou-se um aumento significativo da fração de ejeção do ventrículo esquerdo (51,0±13,1% versus 58,4±9,1%, p<0,001) e da área valvular aórtica (0,6±0,1cm2versus 2,1±0,2cm2, p=0,0001). No final do estudo, observou-se uma melhoria dos parâmetros de função diastólica, com aumento da onda E mitral, diminuição da onda A mitral e aumento da relação E/A. Os tempos de desaceleração da onda E e o de relaxamento isovolumétrico encurtaram e o indíce de Tei diminuiu. Por ecocardiografia com Doppler tecidular observou-se um aumento da velocidade sistólica de deslocamento da parede lateral (Sm) e da velocidade da onda E’ (Em). Ocorreu igualmente um aumento das velocidades de deslocamento do anel mitral septal (Sm e Em) e uma redução do índice de Tei.
ConclusãoOs doentes com estenose aórtica grave têm alterações estruturais do ventrículo esquerdo e disfunção diastólica. A implantação de VAP pode reverter estas alterações, conforme foi demonstrado neste estudo de ecocardiografia Doppler convencional e tecidular. Ocorreu ainda uma redução dos níveis plasmáticos de BNP após implantação de VAP.
Degenerative aortic stenosis (AS) is the most common valvulopathy in the Western world. Transcatheter aortic valve implantation (TAVI) is an alternative treatment modality for patients with severe symptomatic AS who are at high risk for conventional aortic valve replacement (AVR) or are considered inoperable.1
B-type natriuretic peptide (BNP) is a marker of high left ventricular (LV) filling pressures and high wall shear stress independently of etiology and a strong predictor of mortality in heart failure patients.
The prognostic value of BNP has been previously shown in heart failure and severe AS.2 The present study aimed to examine changes in serum BNP levels over time after transcatheter aortic valve implantation (TAVI). In addition, we aimed to assess the relationship of BNP with LV systolic and diastolic function in patients undergoing TAVI.
MethodsPatientsBetween 2013 and 2015, 55 patients with symptomatic severe AS (aortic valve area [AVA] <1 cm2 or aortic valve index <0.5 cm2/m2) were enrolled. All had been referred for TAVI because of high operative risk, and all patients whose BNP levels were measured at baseline and after the TAVI procedure were included in the study. Suitability for TAVI was carefully considered in all patients by a multidisciplinary team consisting of an interventional cardiologist, a cardiac surgeon, a cardiac anesthetist and the patient's primary cardiologist. Patients’ symptomatic status was determined at baseline and at follow-up, including New York Heart Association (NYHA) functional class. Serum BNP levels were measured using a fluorescent immunoassay (Triage BNP Test, Biosite Diagnostics, San Diego, CA) within 24 h prior to the procedure (defined as baseline levels), and at the third month control.
Echocardiographic assessmentAll patients underwent echocardiographic assessment at baseline and after the TAVI procedure in accordance with the American Society of Echocardiography criteria. Measurements were obtained in parasternal long-axis, parasternal short-axis, apical 4-chamber and apical 5-chamber views with the patient in the left lateral position. LV diastolic dysfunction (LVDD) was determined according to the standard guidelines. Criteria for the classification of LVDD were as follows: impaired diastolic relaxation was defined as E/A ratio <1 and E-wave deceleration time (EDT) >240 ms; pseudonormal filling as E/A ratio of 1-1.5, EDT >240 ms and isovolumetric relaxation time (IVRT) <90 ms or ratio between pulmonary vein diastolic and systolic filling velocities (PVd/PVs) >1.5; and restrictive pattern as EDT <160 ms with E/A ratio >1 and IVRT <70 ms.
For tissue Doppler imaging (TDI), mitral flow was acquired in apical 2- and 4-chamber views. The sample volume was placed at the junction of the mitral annulus and the LV septum and lateral, inferior and anterior walls and was maintained perpendicular to the axis of the wall. Systolic myocardial velocity (Sm) and early diastolic (Em) and late diastolic (Am) myocardial velocities were measured and the Em/Am ratio was calculated (Figure 1). The myocardial performance index (MPI) (Tei index) was obtained by dividing the sum of isovolumetric contraction time and IVRT by ejection time on TDI. All patients underwent transesophageal echocardiography to determine annulus size prior to the procedure.
Transcatheter aortic valve implantation procedureTAVI was performed with the Edwards SAPIEN valve (Edward LifeSciences, Irvine, CA), which consists of a trileaflet bioprosthetic bovine pericardial tissue valve, mounted and sutured in a balloon-expandable cobalt-chromium stent. Valve size was selected based on annulus size measured by transesophageal echocardiography and/or during balloon sizing. Valves were implanted in all patients through a transfemoral approach. Balloon predilatation was performed in all patients in order to decide valve size and to aid with valve implantation.
Preprocedurally all patients were treated with aspirin (100 mg/day) and a 300 mg loading dose of clopidogrel. During the intervention, patients received weight-adjusted intravenous heparin with a target activated clotting time of 250-300 s for the duration of the operation. A percutaneous closure device (Prostar XL or ProGlide) was used in 37 cases (67.2%) and surgical cut-down in the remainder.
Statistical analysisContinuous variables were expressed as means with standard deviation or medians with interquartile range, and categorical variables as proportions and percentages. The non-parametric Kolmogorov-Smirnov test and histograms were used to assess, statistically and graphically, the normality of distribution of continuous variables. Differences between groups were analyzed by a two-tailed Student's t test for independent samples (or Wilcoxon's non-parametric test when appropriate) for continuous variables. Correlations of variables were assessed using Pearson or Spearman's correlation analysis. A two-sided p-value <0.05 was considered to represent statistical significance. The statistical analysis was performed using SPSS 16 for Windows (SPSS Inc, Chicago, Illinois, USA).
ResultsThe study population consisted of 55 patients referred for TAVI. Mean logistic EuroSCORE was 25.62±6.34%, mean Society of Thoracic Surgeons score was 10.19±3.14 and mean age was 79.9±7.8 years. The clinical characteristics of the study population are presented in Table 1.
Baseline clinical characteristics of the study population.
| Age (years) | 78.9±7.8 |
| Gender (male/female), n | 21/34 |
| BMI (kg/m2) | 27.1±4.0 |
| STS score | 10.19±3.14 |
| Logistic EuroSCORE | 25.62±6.34 |
| NYHA class IV, n (%) | 12 (21.8) |
| Diabetes, n (%) | 20 (36.4) |
| Smoker, n (%) | 4 (7.3) |
| Systemic hypertension, n (%) | 34 (61.8) |
| CAD, n (%) | 30 (54.5) |
| PAD, n (%) | 15 (27.2) |
| COPD, n (%) | 50 (90.9) |
| Mild | 13 (26) |
| Moderate | 29 (58) |
| Severe | 8 (16) |
| Renal failure (CrCl <60 ml/min), n (%) | 17 (30.9) |
| Previous CABG, n (%) | 7 (12.7) |
| Previous stroke, n (%) | 6 (10.9) |
| Previous PPI, n (%) | 2 (3.6) |
| AF, n (%) | 4 (7.2) |
Values are expressed as number (%) or mean ± standard deviation.
AF: atrial fibrillation; BMI: body mass index; CABG: coronary artery bypass grafting; CAD: coronary artery disease; COPD: chronic obstructive pulmonary disease; CrCl: creatine clearance; NYHA: New York Heart Association; PAD: peripheral artery disease; PPI: permanent pacemaker implantation; STS: Society of Thoracic Surgeons.
The 30-day mortality rate was 1.8% (one patient within 48 h). One patient required a permanent pacemaker (1.8%) and no mortality was recorded after TAVI at follow-up. The clinical features and conventional echocardiographic and TDI characteristics of patients initially and at one year after TAVI are presented in Tables 2 and 3.
Clinical features and conventional echocardiographic measurements before and after TAVI.
| Variables | Before TAVI | After TAVI (1 death) | p |
|---|---|---|---|
| NYHA class, n (%) | |||
| I | 0 | 8 (14.8) | |
| II | 3 (5.5) | 39 (72.3) | |
| III | 40 (72.7) | 5 (9.2) | |
| IV | 12 (21.8) | 2 (3.7) | |
| Peak AVG, mmHg | 72.0±18.4 | 15.2±4.6 | 0.0001 |
| Mean AVG, mmHg | 51.0±15.1 | 8.2±2.4 | 0.0001 |
| AVA, cm2 | 0.6±0.1 | 2.1±0.2 | 0.0001 |
| LVEF, % | 51.0±13.1 | 58.4±9.1 | 0.0001 |
| LVEDD, mm | 48.4±7.2 | 48.2±5.5 | NS |
| LVESD, mm | 33.8±9.1 | 31.5±6.0 | 0.03 |
| LVEDV, ml | 97.6±22.6 | 108.4±22.5 | 0.001 |
| LVESV, ml | 37.6±10.7 | 34.8±8.6 | NS |
| LVSV index, ml/m2 | 61.7±16.1 | 74.0±16.3 | 0.0001 |
| IVSD, mm | 14.4±1.7 | 13.1±1.8 | 0.0001 |
| PWD, mm | 13.6±1.5 | 12.7±1.5 | 0.001 |
| LAd, mm | 29.1±2.7 | 27.0±2.2 | 0.001 |
| PASP, mmHg | 49.1±18.2 | 34.6±11.9 | 0.0001 |
| LV MPI | 0.47±0.11 | 0.43±0.05 | 0.03 |
| E wave, m/s | 0.55±0.10 | 0.75±0.11 | 0.0001 |
| A wave, m/s | 0.75±0.10 | 0.54±0.10 | 0.0001 |
| E/A | 0.71±0.05 | 1.36±0.14 | 0.0001 |
| DT, ms | 237.7±20.0 | 196.9±18.6 | 0.0001 |
| IVRT, ms | 119.5±7.6 | 100.3±8.2 | 0.0001 |
| Normal LV diastolic function, n (%) | 0 | 17 (30.9) | |
| Grade 1 LV diastolic dysfunction, n (%) | 26 (47.3) | 35 (63.6) | |
| Grade 2 LV diastolic dysfunction, n (%) | 17 (30.9) | 2 (3.6) | |
| Grade 3 LV diastolic dysfunction, n (%) | 12 (21.8) | 1 (1.8) | |
Values are expressed as means ± SD or percentages unless otherwise indicated.
AVA: aortic valve area; AVG: aortic valve gradient; BNP: brain-type natriuretic peptide; DT: deceleration time; IVRT: isovolumetric relaxation time; IVSD: interventricular septal diameter; LA: left atrial; LAd: left atrial anteroposterior diameter; LAVI: left atrial volume index; LV: left ventricular; LVEDD: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction; LVESD: left ventricular end-systolic diameter; LVEDV: left ventricular end-diastolic volume; LVESV: left ventricular end-systolic volume; LVSV: left ventricular stroke volume; MPI: myocardial performance index; NS: not significant; NYHA: New York Heart Association; PASP: pulmonary artery systolic pressure; PWD: posterior wall diameter; TAVI: transcatheter aortic valve implantation.
Baseline and follow-up tissue Doppler imaging assessments of left ventricular lateral and septal wall.
| Variables | Before TAVI | After TAVI (3rd month) | p |
|---|---|---|---|
| LV lat Sm (cm/s) | 7.0 (7.0-8.2) | 9.0 (8.0-10.0) | 0.01 |
| LV lat Em (cm/s) | 9.0 (7.0-12.3) | 11.7 (9.7-15.0) | <0.001 |
| LV lat Am (cm/s) | 10.8±2.5 | 10.1±2.4 | NS |
| LV lat Em/Am | 0.83 (0.60-1.26) | 1.20 (0.91-1.36) | <0.001 |
| LV lat IVRT (ms) | 99.3±19.0 | 85.7±13.0 | <0.001 |
| LV lat MPI | 0.677±0.025 | 0.614±0.020 | <0.001 |
| LV sep Sm (cm/s) | 7.5 (7.0-9.0) | 8.0 (8.0-9.0) | 0.007 |
| LV sep Em (cm/s) | 8.0 (6.0-9.0) | 9.0 (7.0-13.0) | <0.001 |
| LV sep Am (cm/s) | 10.0 (9.0-11.0) | 10.0 (8.0-10.0) | NS |
| LV sep Em/Am | 0.80 (0.62-1.00) | 1.05 (0.80-1.30) | <0.001 |
| LV sep IVRT (ms) | 97.0 (80.0-107.5) | 83.0 (75.5-98.0) | <0.001 |
| LV sep MPI | 0.696±0.026 | 0.604±0.024 | <0.001 |
| Septal E/e’ ratio | 15.09±1.60 | 13.69±1.55 | <0.001 |
| Lateral E/e’ ratio | 15.67±1.46 | 14.72±1.41 | <0.001 |
| Mean E/e’ | 15.37±1.52 | 14.20±1.41 | <0.001 |
Values are expressed as means ± standard deviation or means (range).
Am: late diastolic myocardial velocity; Em: early diastolic myocardial velocity; IVRT: isovolumetric relaxation time; lat: lateral; LV: left ventricular; MPI: myocardial performance index; NS: not significant; sep: septal; Sm: systolic myocardial velocity.
Statistically significant early decreases in peak aortic valve gradient and mean LVEF and AVA were noted, with significant increases in the latter two. Significant decreases in interventricular septal diameter and posterior wall diameter were observed in the post-TAVI period. The decrease in LV end-systolic diameter end-diastolic diameter after TAVI was non-significant, but the decrease in LV end-systolic diameter during follow-up was statistically significant. Statistically significant decreases in left atrial anteroposterior diameter and increases in LV end-diastolic volume were observed after TAVI, and there was a trend for lower LV end-systolic volume. Consequently, a significant increase in LV stroke volume index was observed in the post-TAVI period. Positive changes in pulmonary artery systolic pressure (PASP) and LV MPI were also noted. PASP and MPI decreased significantly after TAVI (Table 2).
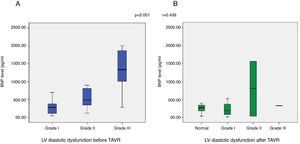
All patients had some degree of LV diastolic dysfunction before the TAVI procedure, and significant improvements in diastolic function was observed after TAVI. Table 2 shows the degree of LV diastolic dysfunction before and after TAVI.
LV lateral wall Sm and Em increased significantly after TAVI. There was no significant change in LV lateral wall Am, hence the lateral wall Em/Am ratio increased (Table 3). There were statistically significant decreases in lateral wall IVRT and MPI after TAVI (Table 3). Septal wall systolic wave velocity increase was also statistically significant. Septal wall Am was not significantly altered after TAVI, whereas there was a statistically significant increase in septal wall Em. Moreover, an increase in both septal wall and lateral Sm was found after TAVI, and this correlated with an increase in LVEF (r=0.38, p=0.001). There was a significant improvement in septal wall MPI after the TAVI procedure. In additional, positive changes in septal wall E/e’ ratio were observed after TAVI (Table 3).
No association was found between serum BNP level and AVA (r=-0.254, p=0.06). However, a significant correlation was found between BNP level and LV ejection fraction (LVEF) (r=-0.44, p=0.001), PASP (r=0.27, p=0.04) and NYHA class (r=0.33, p=0.001). A statistically significant decrease was observed in BNP levels of all patients after TAVI (Figure 1). The correlation between BNP levels and degree of diastolic dysfunction before and after TAVI is demonstrated in Figure 2. Multivariate linear regression analysis revealed that LVEF (p=0.003) was an independent predictor of BNP decrease (Table 4).
Multivariate linear regression analysis demonstrating predictors of falls in B-type natriuretic peptide levels in patients undergoing transcatheter aortic valve implantation.
| Variable | Risk ratio | 95% confidence interval | p |
|---|---|---|---|
| Age | -13.328 | -37.064 to 10.407 | 0.267 |
| Gender | -26.256 | -395.962 to 343.450 | 0.888 |
| LVEF | -20.216 | -33.493 to -6.938 | 0.003 |
| STS score | 38.313 | -23.225 to 99.852 | 0.219 |
| Hypertension | 154.284 | -181.576 to 490.144 | 0.363 |
| CKD | -207.396 | -570.517 to 155.724 | 0.259 |
| BMI | -11.045 | -54.216 to 32.126 | 0.612 |
| Hemoglobin level | -39.866 | -134.831 to 55.099 | 0.405 |
BMI: body mass index; CKD: chronic kidney disease; LVEF: left ventricular ejection fraction; STS: Society of Thoracic Surgeons.
Brain-type natriuretic peptide (BNP) is synthesized within the ventricles (as well as in the brain, where it was first identified). BNP is initially produced as pre-proBNP, which is then cleaved to proBNP and finally to BNP. These hormones have vasodilatory and diuretic effects and are antagonists of the adrenergic and renin-angiotensin systems.
Increased myocardial wall stress has been proposed as a stimulus for the release of natriuretic peptides in AS.3 The prognostic value of these peptides in heart failure is well known,4 and is also becoming increasingly apparent in patients with valvular disease. In particular, in patients with AS, BNP levels are directly related to severity and symptomatology.5,6 In the present study, there was a strong association between NYHA class and serum BNP levels.
Natriuretic peptide levels are related to disease severity in AS and have prognostic value, predicting early outcome7 and long-term mortality from any cause following conventional AVR.8 Recently, BNP was found to be a predictor of 30-day outcome after TAVI.9 However, correlations between BNP level and mortality could not be analyzed in our study due to the limited number of patients. Moreover, BNP elevation is a predictor of low LVEF, as shown in a previous study.10 However, we can state that a decrease in BNP levels predicts increased LVEF after TAVI.
BNP elevation is associated with higher grade diastolic dysfunction and higher PASP in patients with severe AS undergoing TAVI. This marker would be useful clinically if a rise in BNP precedes the currently recognized clinical signs. However, in our study BNP level had no association with severity of AS. Some reports indicate that BNP level is an independent predictor of cardiovascular death in patients with severe AS.11–13 Furthermore, preoperative N-terminal (NT)-proBNP level independently predicts symptom-free survival.7 On the other hand, Pfister et al.14 found no association between NT-proBNP and two-month mortality after transapical TAVI.
Correlates found in our study were mostly symptoms and signs of heart failure, including NYHA class, depressed LVEF, and elevated PASP. Importantly, no relationship was found between BNP level and severity of AS. Moreover, our study revealed an increase in LVEF and improvement in diastolic function as well as decreased PASP and BNP levels in patients with severe AS after TAVI.
Three important conclusions can be derived from these data. First of all, we found that BNP levels are closely linked with findings of heart failure and degree of diastolic dysfunction. Secondly, as in the study by Ben-Dor et al.,10 there was no significant correlation between BNP level and AVA in our study, which included only severe AS patients. Other studies that included mild to severe AS patients did in fact correlate AS severity with higher BNP values.5,15 Thirdly, our study demonstrated improvements in all these parameters and NYHA class.
Pfister et al.14 reported an increase in NT-proBNP levels three days after TAVI, and they were still elevated at three months compared with baseline. In contrast to this finding, we found a significant decrease in BNP levels three months after TAVI. This indicates that BNP levels may fall two months after TAVI. Additionally, Spargias et al.16 reported an early reduction in NT-proBNP after transfemoral TAVI.
In patients with AS, higher increases in annualized BNP were significantly associated with a higher rate of the composite endpoint of occurrence of symptoms, AVR, or cardiovascular death.17 An increase in BNP of >20 pg/ml per year was associated with worse outcomes, even after adjustment for age and echocardiographic parameters. Therefore, follow-up measurement of serum BNP levels may be useful to predict adverse events in patients treated with TAVI.
The majority of studies assessing the effect of TAVI on cardiac function have used classical echocardiographic parameters. These methods have some limitations, due to the fact that they are affected by changes in preload and afterload. In the literature, there is no study using TDI that managed to overcome these limitations to a significant extent. MPI is an independent marker of LV dysfunction that is independent of changes in heart rate and is valuable in the assessment of global LV function and the risk of developing heart failure.18 In our study, LV Doppler measurements demonstrated a decrease in MPI after TAVI compared to baseline. On TDI, lateral and septal wall MPI was found to be significantly diminished after TAVI.
Vogel et al.19 demonstrated a good correlation of LVEF with Sm during ventricular contraction and showed that it is affected by load. In our study, an increase was found in both septal wall and lateral Sm after TAVI, and this also correlated with an increase in LVEF. Moreover, an increase in lateral and septal Em by TAVI was evident, however there was no significant change in Am. Consequently, an increased Em/Am ratio was found in both lateral and septal walls.
This study has some limitations. Our study is an observational, single-center registry of patients referred for TAVI. The sample size may be considered small. Moreover, the follow-up period was relatively short. In this narrow range of high-risk patients with advanced disease, the correlation between BNP and mortality is more difficult to establish; a larger sample size is needed to establish this correlation. Large randomized controlled trials could provide more definitive evidence in the future. The cohort included an elderly population with many comorbidities, which may have affected the other parameters.
Our findings could have important implications in the clinical management and follow-up of these patients. Specifically, we recommend BNP follow-up after TAVI. Decreased serum BNP levels are associated with hemodynamic improvement in these patients. Thus, decreased BNP levels after TAVI may be associated with lower periprocedural and long-term risks.
Our study demonstrated the existence of impairment in LV structure and diastolic function in AS patients and both conventional Doppler echocardiography, and TDI confirmed that this impairment can be reversed by TAVI.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.