Acromegaly is a rare disease, mostly caused by a growth hormone (GH)-secreting benign pituitary tumor, with an increased production of GH and insulin-like growth factor 1 (IGF-1). Cardiovascular complications are common and are associated with cardiomyocyte apoptosis and concentric cardiac hypertrophy. Suppression of GH and IGF-1 appears to improve cardiac function only in the short term, with little or no decrease in left ventricular mass or improvement in cardiac function after prolonged treatment. Alcohol septal ablation (ASA) has emerged as a minimally invasive alternative to septal myectomy, with significant improvement in symptoms, gradients and left ventricular remodeling. In this report, we describe the case of a 73-year-old woman with acromegaly due to a pituitary adenoma diagnosed and treated surgically at the age of 38 but with recurrence and reoperation at the age of 50. She was referred to our cardiology department due to a three-month history of progressively worsening exercise-induced dyspnea and orthopnea under optimal medical therapy. Echocardiography and magnetic resonance imaging revealed severe basal hypertrophy of the interventricular septum (19 mm), dynamic left ventricular outflow tract obstruction with a gradient of 70 mmHg at rest and 120 mmHg with Valsalva maneuver, and systolic anterior movement (SAM). Genetic testing excluded the most frequent forms of familial hypertrophic cardiomyopathy. ASA was performed with injection of 2 cc of alcohol in the first septal branch of the left coronary artery, without complications. At one-year reassessment, significant clinical and echocardiographic improvement was noted, with disappearance of SAM. To our knowledge, there have been no previously reported cases of ASA in hypertrophic cardiomyopathy due to acromegaly. We report a case of successful ASA in acromegalic cardiomyopathy.
A acromegalia é uma doença rara, causada essencialmente por um tumor benigno da glândula pituitária secretor de hormona de crescimento (HC), provocando uma produção excessiva de HC e de fator de crescimento semelhante à insulina tipo 1 (IGF-1). As complicações cardiovasculares são comuns e têm sido associadas à apoptose de cardiomiócitos e à hipertrofia cardíaca concêntrica. A supressão de HC e de IGF-1 parece melhorar a função cardíaca apenas a curto prazo, com pouco ou nenhum efeito na redução da massa ventricular esquerda ou na melhoria da função cardíaca a longo prazo. A ablação septal alcoólica (ASA) surgiu como uma alternativa minimamente invasiva à miectomia septal com melhoria significativa a nível de sintomas, gradientes e remodelagem ventricular esquerda. Neste caso clínico, descrevemos as imagens de uma mulher de 73 anos de idade, com acromegalia devido a um adenoma da glândula pituitária diagnosticado, e submetida a cirurgia aos 38 anos, mas com recorrência e reoperação aos 50 anos. A doente foi referenciada ao nosso departamento de cardiologia por um quadro com três meses de evolução de dispneia de esforço e ortopneia com agravamento progressivo sob terapêutica médica otimizada. O ecocardiograma e ressonância magnética cardíaca revelaram uma hipertrofia grave da porção basal do septo interventricular (19 mm), com um gradiente obstrutivo dinâmico da câmara de saída do ventrículo esquerdo de 70 mmHg em repouso e de 120 mmHg com a manobra de Valsalva e com movimento sistólico anterior (SAM) da válvula mitral. A avaliação genética excluiu as formas mais frequentes de cardiomiopatia hipertrófica (CMH) familiar. A ASA foi realizada com 2 cc de injeção de álcool na primeira artéria coronária septal, sem complicações. Na reavaliação do primeiro ano, houve uma melhora clínica e ecocardiográfica significativa com o desaparecimento de SAM. Tanto quanto é do nosso conhecimento, não existe na literatura a descrição de casos de ASA em doentes com CMH por acromegalia. Relatamos aqui o caso de uma ASA bem-sucedida numa cardiomiopatia acromegálica.
Acromegaly is a rare disease that is most often caused by a growth hormone (GH)-secreting benign pituitary tumor and is characterized by progressive skeletal and soft tissue overgrowth, frequently accompanied by cardiovascular, cerebrovascular, and respiratory complications that contribute to the poor prognosis observed in this condition.1 Cardiovascular disorders are common and are mainly responsible for the two-fold increase in mortality seen in acromegalic patients.1,2 The increased autonomous production of GH results in increased insulin-like growth factor 1 (IGF-1), and chronic excess secretion of both hormones is associated with various changes in cardiac structure and function due to cardiomyocyte apoptosis, with concentric cardiac hypertrophy being a frequent finding even in young patients with short disease duration. As a consequence, early impairment of left ventricular (LV) diastolic filling has been described, while impaired systolic function with heart failure may develop in later stages if the disease is untreated or unsuccessfully treated.1–3 Other cardiovascular disorders such as hypertension, coronary artery disease and ventricular arrhythmias may be present and worsen acromegalic cardiomyopathy, defined as any cardiac involvement in acromegalic patients in the absence of other known causes of cardiomyopathy.1 Lowering of GH and IGF-1 to age-corrected normal limits is mandatory; however, treatment of acromegaly appears to improve cardiac function only in the short term, with little or no decrease in left ventricular mass or improvement in cardiac function after prolonged treatment.4
Alcohol septal ablation (ASA) has emerged as a minimally invasive alternative to septal myectomy for patients with obstructive hypertrophic cardiomyopathy (HCM) and symptoms refractory to medical therapy. This procedure alleviates symptoms by producing a targeted, limited infarction of the upper interventricular septum, resulting in an increase in left ventricular outflow tract (LVOT) diameter, a decrease in LVOT gradients, and regression of the component of LV hypertrophy that is due to pressure overload. Clinical success, with significant improvement in symptoms and reduction in gradients, is achieved in the great majority of patients and has been correlated with left ventricular remodeling. Non-randomized comparisons of septal ablation and septal myectomy have shown similar mortality rates and post-procedure New York Heart Association (NYHA) class for the two procedures.5,6 To our knowledge, there have been no previously reported cases of ASA in hypertrophic cardiomyopathy due to acromegaly. We report a case of successful ASA in acromegalic cardiomyopathy.
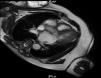
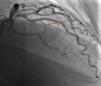
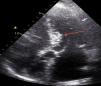
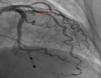
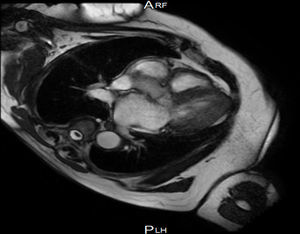
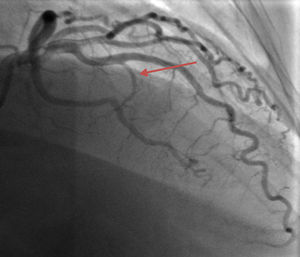
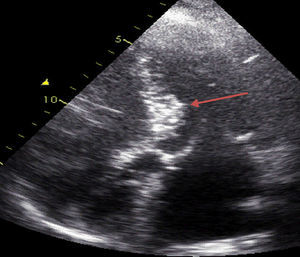
Case reportWe describe the case of a 73-year-old woman with acromegaly due to a pituitary adenoma diagnosed and treated surgically at the age of 38 but with recurrence and reoperation at the age of 50. She had a history of hypertension, multinodular goiter and atrial fibrillation under oral anticoagulation. She was referred to our cardiology department due to echocardiographic evidence of obstructive hypertrophic cardiomyopathy and a three-month history of progressively worsening exercise-induced dyspnea and orthopnea (NYHA class III) under optimal medical therapy. A complete echocardiogram revealed severe asymmetric hypertrophy of the left ventricle, mostly in the basal portion of the interventricular septum (19 mm), without LV dilation, depressed ejection fraction or wall motion abnormalities. There was also a dynamic LVOT obstruction gradient of 70 mmHg at rest and of 120 mmHg with Valsalva maneuver and systolic anterior movement (SAM) of the mitral valve with mild regurgitation and moderate to severe tricuspid regurgitation. A better characterization with magnetic resonance imaging confirmed basal interventricular septal hypertrophy without evidence of intramyocardial fibrosis (Figure 1). Genetic testing excluded the most frequent forms of familial hypertrophic cardiomyopathy. A 24-hour Holter examination revealed permanent atrial fibrillation but no ventricular repolarization or heart rate abnormalities. After a multidisciplinary discussion, ASA was performed, guided by myocardial contrast echocardiography, with injection of 2 cc of alcohol in the first septal branch of the left coronary artery (Figures 2–4). The procedure was uneventful and no atrioventricular (AV) conduction disturbances were detected. The one-year echocardiographic reassessment showed a reduction of the interventricular septum to 13 mm and of 8 mm in the region treated by ASA. The LVOT gradient was 28 mmHg at rest and the SAM of the mitral valve and the moderate to severe tricuspid regurgitation had disappeared. The patient improved significantly to mild-to-moderate heart failure (NYHA class I-II) and no major cardiovascular events were observed during follow-up.
Left ventricular hypertrophy is a well-known feature of cardiac involvement in acromegaly, affecting more than 60% of patients, independently of hypertension.2 The etiology of acromegalic cardiomyopathy has not been fully clarified, but long-term elevations in serum GH and IGF-I levels may cause myocardial hypertrophy and interstitial fibrosis of cardiomyocytes by acting on these cells through specific receptors. In the present report, a 38-year history of undiagnosed acromegaly could have caused this hypertrophic structural pattern responsible for the diastolic filling abnormality observed, and eventually left ventricular dysfunction occurred, resulting in congestive heart failure.3,4 Several studies have demonstrated a significant decrease in LV hypertrophy following successful suppression of hormone levels by surgery or somatostatin analog treatment.2–4 However, as seen in this case, even with corrective surgery there is the suggestion that long-standing GH and IGF-I hypersecretion modifies cardiac structure in a way that can no longer be reversed by disease control. In these cases treatment has to be guided from a cardiological standpoint.
ASA has emerged as a safe and attractive modality to treat patients with obstructive HCM whose symptoms are refractory to optimal medical therapy with negative inotropic agents. The procedure has been refined over the decades since its introduction. However, concerns have been raised over the higher risk of complete AV block and development of a potentially arrhythmogenic scar after ASA.6 Although surgical myectomy is the standard therapy for drug-resistant obstructive HCM, ASA is an alternative that may be considered for many patients. Data indicate that the medium-term functional and hemodynamic success of ASA is high and similar to that of surgery, with the advantage that it may be performed in patients considered unsuitable for surgery.5 In the case presented, the coronary anatomy was favorable, with the approachable septal coronary arteries required for the procedure, which was performed without adverse events. This first report of ASA in acromegalic cardiomyopathy highlights the need to monitor cardiac performance carefully in acromegalic patients even after suppression of GH and normalization of IGF-I levels.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.