Right ventricular infarction is uncommon in isolation but can be observed in 50% of cases of inferior wall myocardial infarction. Diagnosis is difficult and suspicion of this condition should always be borne in mind. Progression to cardiogenic shock is not uncommon, when the outcome is similar to left ventricular infarction; mortality can reach 60%. We present the case of a 64-year-old woman with known coronary disease who was admitted to our coronary care unit after an anterior myocardial infarction. Cardiac catheterization showed diffuse stenosis of the left descending and 70% stenosis of the posterior descending arteries. She was surgically revascularized with a favorable evolution, but was later readmitted for acute decompensated heart failure with cardiogenic shock. She was refractory to medical therapy, with biventricular dysfunction on echocardiographic examination. Cardiac magnetic resonance imaging confirmed the diagnosis of right ventricular infarction.
O enfarte do miocárdio isolado do ventrículo direito é uma entidade patológica incomum; no entanto, pode estar associada a até 50% dos enfartes agudos do miocárdio da parede inferior. A realização deste diagnóstico pressupõe um elevado grau de suspeição clínica. A evolução para choque cardiogénico pode ocorrer num número considerável de casos e o outcome descrito é semelhante ao enfarte miocárdico do ventrículo esquerdo, com uma mortalidade que pode atingir os 60%. Os autores apresentam o caso clínico de uma doente de 64 anos, com história prévia de doença coronária, admitida após enfarte agudo do miocárdio da parede anterior. O cateterismo cardíaco mostrou estenose difusa da artéria coronária descendente anterior e estenose de 70% da artéria coronária descendente posterior. Foi submetida a cirurgia de revascularização miocárdica. Cerca de um mês após este evento, foi readmitida em contexto de insuficiência cardíaca aguda, em choque cardiogénico, com disfunção sistólica biventricular. Apresentava eletrocardiograma semelhante ao prévio, bem como cateterismo cardíaco, que mostrava a patência da pontagem realizada. Após estabilização clínica, foi submetida a RMN cardíaca, que evidenciou a presença de realce tardio na parede livre do ventrículo direito, confirmando a hipótese de enfarte miocárdio do ventrículo direito.
Although right ventricular infarction (RVI) has been known for 70 years, its clinical importance was first recognized in 1974 by Cohn et al.,1 who studied its clinical and hemodynamic features.2 It was first identified in a subgroup of patients with inferior wall myocardial infarction who presented right ventricular failure and elevated right ventricular filling pressures despite relatively normal left ventricular filling pressures. Increasing recognition of RVI, in association with left ventricular infarction or as an isolated event, highlights the clinical significance of the right ventricle in total cardiac function.
Case reportWe present a case of a 64-year-old woman, obese and dyslipidemic, with a history of coronary angioplasty with stent implantation in the circumflex coronary artery.
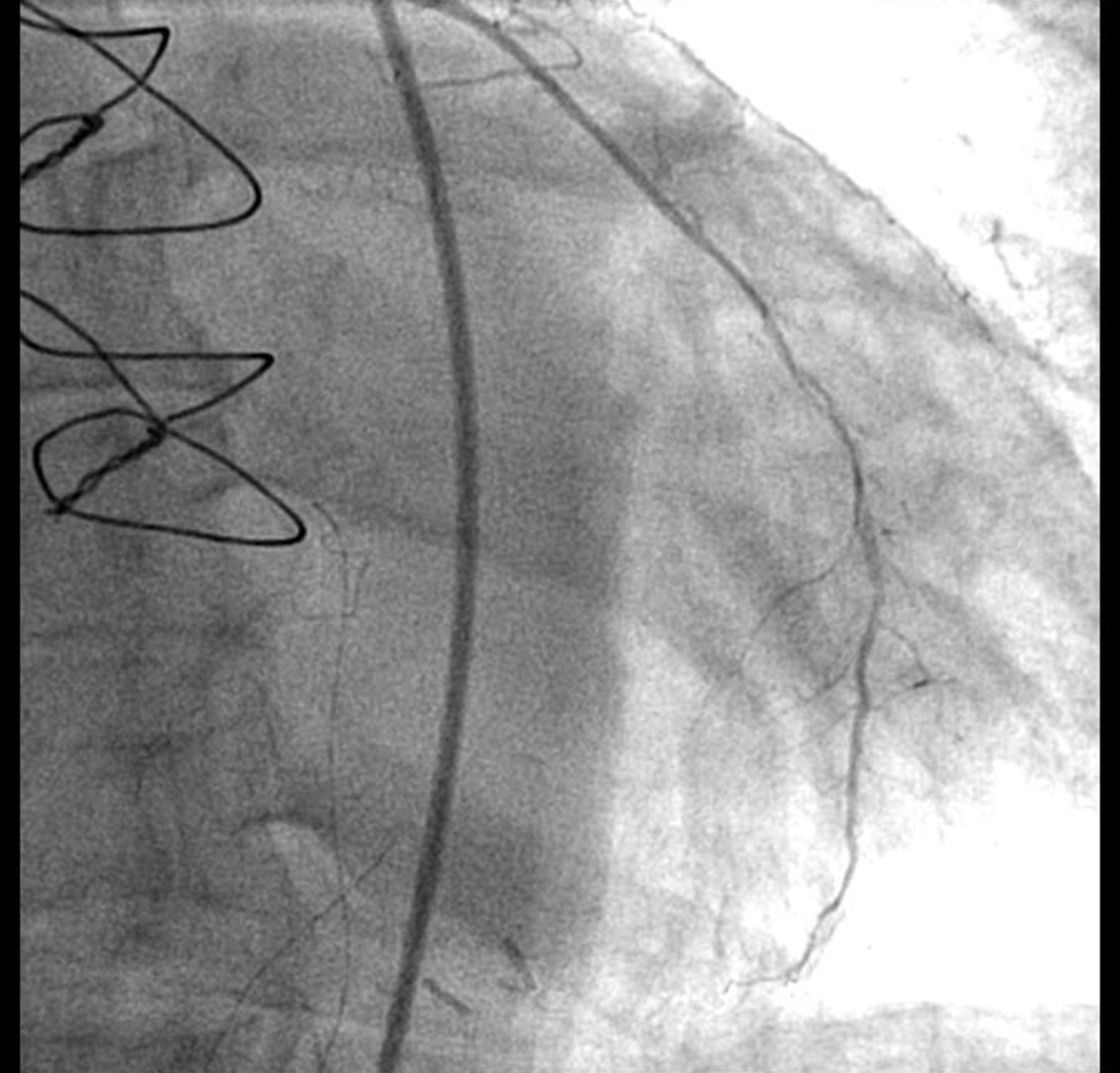
She was admitted to our coronary care unit due to ST-segment elevation myocardial infarction of the anterior wall. Cardiac catheterization revealed long and diffuse stenosis of the left anterior descending and 70% stenosis of the posterior descending coronary arteries (Figure 1).
The coronary anatomy was not suitable for percutaneous revascularization and she underwent coronary artery bypass grafting (CABG) (left internal mammary artery to left anterior descending coronary artery). The transthoracic echocardiogram showed mild impairment of left ventricular systolic function; peak troponin I was 7.04ng/ml. During her stay she evolved favorably with no postoperative complications.
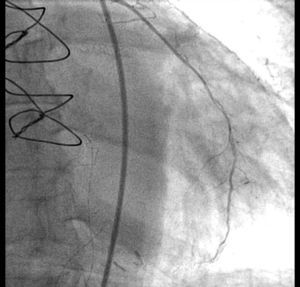
A month later the patient was readmitted to our unit with chest pain and acute heart failure evolving to cardiogenic shock. The ECG was similar to the previous one and troponin I was elevated (2ng/ml). The transthoracic echocardiogram revealed severe biventricular systolic dysfunction. The right ventricle was slightly dilated, tricuspid annular plane systolic excursion was 13mm and S′ on tissue Doppler imaging was 9cm/s. Tricuspid regurgitation was moderate and pulmonary artery systolic pressure (PASP) was estimated at 32mmHg. Although it was difficult to assess, the right ventricular free wall was globally hypokinetic, with no signs suggesting pulmonary embolism, including the McConnell sign. Repeat cardiac catheterization showed good results of the previous angioplasty and CABG (Figure 2) and the known 70% stenosis of the posterior descending coronary artery. Right heart catheterization revealed low peripheral vascular resistance (1.64 Wood units) with pulmonary capillary wedge pressure of 12mmHg and PASP of 23mmHg.
The patient responded poorly to fluid resuscitation, and inotropic support and non-invasive ventilation were required due to worsening of the clinical setting with refractory cardiogenic shock.
After initiation of aggressive medical therapy she gradually began to improve. Due to an episode of self-limited atrial fibrillation the patient was started on anticoagulation.
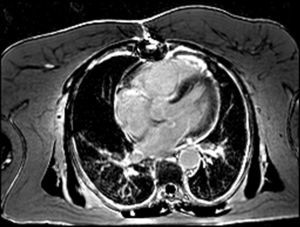
Considering the patient's ischemic burden, new-onset biventricular systolic dysfunction, and the absence of signs of pulmonary embolism, and as she was clinically stable after three days, it was decided to perform cardiac magnetic resonance imaging (MRI), which showed slight left ventricular systolic dysfunction, right ventricular dilatation with severe systolic dysfunction and transmural late enhancement in the mid-apical segments of the right ventricle, highly suggestive of RVI (Figures 3 and 4). Pulmonary artery angiography showed no signs of pulmonary thromboembolism. In this non-linear clinical case cardiac MRI was sufficiently informative to enable a diagnosis to be made: RVI.
The patient was discharged asymptomatic on the 20th day. The echocardiogram a month later showed total recovery of left ventricular function but persistence of right ventricular dysfunction.
DiscussionIsolated right ventricular infarction is a rare condition, with a prevalence of 3%. Its association with inferior wall infarction has been reported in 14–84% of cases; a lower incidence of 13% has been associated with anterior wall infarction. Chronic respiratory disease and right ventricular hypertrophy are known risk factors for its occurrence.2
It is essential to establish a correct diagnosis of this condition as early recognition can prevent a poor outcome. Mortality in inferior wall myocardial infarction with RVI rises to 30% compared to 6% when there is no right ventricular involvement.2,3
Cardiogenic shock can occur in RVI due to right ventricular dysfunction and to atrioventricular dyssynchrony. It is usually associated with a more extensive infarcted area and mortality is similar to cardiogenic shock due to left ventricular infarction. In-hospital mortality can reach 60%.4,5
Clinical manifestations are dependent on the degree of right ventricular dysfunction. Persistent hypotension with increased jugular vein distension and clear lung fields can increase suspicion in the early stages of RVI. Conduction disturbances are frequent, particularly complete heart block and bradycardia. Various degrees of heart block may be present. Mechanical complications can also occur, with several cases described of rupture of papillary muscles and the ventricular septum.6 It is usually very difficult to establish the diagnosis on clinical grounds alone.
Regarding diagnostic options, several non-invasive and invasive tools are available and should complement each other. The ECG can raise suspicion when signs of inferior wall infarction are present, and in such cases the right precordial leads V4R and V5R should always be calculated. An elevation of 1mm in V4R is specific for RVI and has been established as an independent factor for major complications and in-hospital mortality.2
The transthoracic echocardiogram can reveal dilatation of the right chambers, assess ventricular dysfunction and estimate tricuspid regurgitation and right ventricular pressures, providing several hemodynamic parameters and status. It is also essential to visualize motion wall abnormalities and possible mechanical complications.7
Cardiac catheterization provides information on the coronary tree and is the therapeutic tool when percutaneous revascularization is possible. The posterior wall of the right ventricle is more prone to infarction and coronary stenosis is more commonly observed in a left dominant circumflex artery or the distal right coronary artery. RVI has been associated with both occlusion of a non-dominant right coronary artery and significant right ventricular hypertrophy that increases the susceptibility of the RV to ischemia.8
The case we present clearly illustrates the difficulties of diagnosing and managing RVI.
The patient's clinical deterioration with acute decompensated heart failure in spite of therapy, including revascularization, fluid resuscitation and inotropic support, was a warning that further investigation was required. Cardiac MRI provided a more conclusive study of ventricular function and wall motion abnormalities, and gadolinium late enhancement demonstrated that the ischemic region was in the right apical ventricular wall. Cardiac MRI is the most sensitive method to assess right ventricular function. Right ventricular involvement usually occurs in the inferior segments and the apex of the right ventricle, regions in which imaging of wall motion abnormalities with echocardiography is particularly challenging.8 Most reports do not specify an optimal timing for MRI in an acute setting, and each situation calls for different timings.
The clinical outcome is dependent on the extent of the ischemic area and higher in-hospital mortality has been reported with greater degrees of ventricular dysfunction.5,9 Right ventricular dysfunction in isolated RVI is uncommon and associated with a worse prognosis.
ConclusionsCardiac MRI was the key examination as it established the definitive diagnosis of right ventricular infarction, although it is not usually performed in an acute clinical setting. RVI is a rare and often overlooked entity and, due to the complexity of this case, some questions remain unresolved, particularly the absence of significant stenosis in the right coronary artery and of late enhancement in the left ventricular wall on cardiac MRI. This case illustrates the importance of cardiac MRI when the clinical setting is complicated with confounding factors.
Ethics disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.