Pseudoaneurysm formation after aortic valve and root replacement is a postoperative complication that has traditionally been addressed by surgical means. We describe a case of a large subaortic pseudoaneurysm successfully occluded by transcatheter device closure.
A 64-year-old woman with a history of mitral valve repair and ring implantation due to severe valvular regurgitation was referred for surgical aortic valve replacement due to symptomatic severe aortic valve stenosis and dilated aorta. The postoperative period was complicated by refractory shock, and exploratory surgery revealed a cardiac rupture around the aortic valve, followed by annulus repair and implantation of a new bioprosthetic valve. Echocardiography subsequently showed a persistent cardiac communication with to-and-fro flow and a large pericardial effusion. The computed tomography angiogram (Figure 1A and B) revealed a large fluid collection compressing the pulmonary artery and left atrium. The case was discussed at a meeting of the multidisciplinary heart team, in which cardiac surgeons discouraged an additional (fourth) surgical attempt.
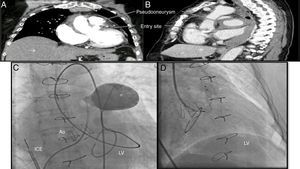
(A) Thoracic computed tomography angiogram, coronal view, showing the pseudoaneurysm and its entry site; (B) sagittal view illustrating a large heterogeneous pericardial fluid collection compressing the great vessels; (C) angiogram of the pseudoaneurysm; (D) closure device inside the pseudoaneurysm and distal disk positioned at the left ventricular wall. Ao: aorta; ICE: intracardiac echocardiography; LV: left ventricle; * pseudoaneurysm/closure device.
A transfemoral approach was used to cannulate the pseudoaneurysm (Figure 1C) and deliver the closure device, an Amplatzer Vascular Plug II™ (St. Jude Medical) (Figure 1D and Videos 1 and 2). At one-year follow-up, imaging confirmed complete cavity closure, device endothelization, and minimal pericardial effusion (Video 3).
Cardiac pseudoaneurysms carry a 30-45% risk of rupture and death within the first year. In high-risk surgical patients transcatheter device closure is a feasible approach to such cardiac defects, and should be increasingly considered as a viable alternative to surgical repair.
Conflicts of interestThe authors have no conflicts of interest to declare.