Atrial fibrillation (AF) is an important and potentially modifiable cause of stroke. It has been known since 1989 that oral anticoagulant drugs, such as warfarin, lead to a dramatic decrease in stroke associated with AF. The best risk-benefit ratio is obtained with intensity of oral anticoagulant treatment for an INR of 2–3, even in the elderly. Given the risks of anticoagulant therapy, including bleeding, individual thromboembolic risk must be assessed in patients with AF. In 2009, dabigatran was shown to be a reasonable alternative to vitamin K antagonists, establishing itself as a major alternative to warfarin in AF patients. Rivaroxaban and apixaban have subsequently also been shown to be alternatives to warfarin. When there are contraindications to vitamin K antagonists, antiplatelet agents can produce a therapeutic effect, although much less than oral anticoagulants. Apixaban may be a better alternative to aspirin in this setting. Patients with low-risk atrial fibrillation (no risk factors) have not been the subjects of specific clinical trials. It is unclear what would be the best therapeutic choice for these patients.
A fibrilação auricular (FA) é uma causa importante e potencialmente modificável do acidente vascular cerebral. Desde 1989 que se encontra demonstrado que o uso de anticoagulantes orais, como a varfarina, se associa a uma redução dramática da incidência de acidente vascular cerebral associado a FA. A intensidade da anticoagulação oral com uma melhor relação risco-benefício é obtida com um INR de 2-3, mesmo no paciente idoso. Tendo em consideração os riscos da anticoagulação oral, incluindo as hemorragias, é necessário estimar o risco tromboembólico individual nos doentes com FA. Em 2009, o dabigatrano mostrou ser uma alternativa razoável aos antagonistas da vitamina K – vindo a estabelecer-se como uma alternativa importante à varfarina em doentes com FA. Foi subsequentemente demonstrado que quer o rivaroxabano quer o apixabano têm um estatuto semelhante ao dabigatrano, enquanto alternativas importantes à varfarina. Quando existam contra-indicações à terapêutica com antagonistas da vitamina K, os antiplaquetários podem produzir um efeito terapêutico, sem dúvida um efeito muito menos importante do que os anticoagulantes orais. O apixabano poderá ser uma alternativa preferível à aspirina neste contexto. Os doentes com FA de “baixo risco” (sem factores de risco) não foram estudados em ensaios clínicos levados a cabo especificamente para esta situação. É pouco claro qual é a melhor alternativa terapêutica nestes doentes.
Atrial fibrillation (AF) is a supraventricular tachyarrhythmia characterized by uncoordinated atrial activation, resulting in deterioration of atrial function. According to the 2010 ESC guidelines,1 AF is considered to be paroxysmal if it ends spontaneously or persistent if it lasts more than seven days or requires termination by cardioversion. According to the same document, “long-standing persistent AF has lasted for ≥1 year when it is decided to adopt a rhythm control strategy”, and “permanent AF is said to exist when the presence of the arrhythmia is accepted by the patient (and physician)”.1
AF is the most common sustained arrhythmia, being responsible for one-third of hospitalizations related to cardiac rhythm disturbances.2 In the last 20 years, admissions due to AF have risen by 60%, which may not only be the result of changes in admission thresholds or clinical practices, but could also reflect a genuine increase in the population incidence.3 In a large European study (the Rotterdam study), the overall prevalence was 5.5%, rising from 0.7% in those aged 55–59 years to 17.8% in those aged 85 and over.4 In the FAMA study, the overall prevalence of AF in 10447 patients aged 40 or over was 2.5%; male gender, increasing age, body mass index, hypertension and lack of physical exercise were noted to influence the prevalence of AF.5
AF is associated with increased long-term risk of stroke. According to the Framingham study,6 the two-year age-adjusted incidence of stroke among patients with AF averages 5%, approximately 5 times that of people without AF. The estimated relative risk (RR) of stroke for patients with AF ranges from 2.6 in those in the 7th decade of life to 4.5 in the 9th decade. Furthermore, the attributable risk of stroke for AF ranges from 1.5% in patients aged 50–59 years to 23.5% in those aged between 80 and 89 years.6
The formation of thrombi due to blood stasis in the left atrial appendage is believed to be a common initial step for cardioembolism in patients with AF7; many other independent risk factors are linked to an increased risk of stroke in these patients, the most consistent being a previous history of stroke, thromboembolism or transient ischemic attack (TIA), diabetes, hypertension and age.8 Other factors are congestive heart failure (CHF) and coronary artery disease (CAD).9
As a result of the high morbidity and mortality associated with AF, it is imperative to prevent its complications, especially thromboembolic phenomena. The aim of this narrative review is to analyze existing data regarding the efficacy and the risk-benefit ratio of the various antithrombotic modalities available for the prevention of the major vascular complications related to nonvalvular AF, particularly stroke and systemic embolism. All secondary cases of AF – in the context of myocardial infarction (MI), cardiac surgery, pericarditis, myocarditis, hyperthyroidism or acute lung disease – were excluded from this review, since in these cases AF may cease to exist with management of the underlying condition.
Due to the heterogeneity of the articles of interest (in the number of patients enrolled, inclusion and exclusion criteria, length of follow-up and drugs under evaluation), an individual description of major clinical trials was performed.
The present report was not funded by any interested party, either industry or governmental, and the decision to carry out this review was taken exclusively by the authors.
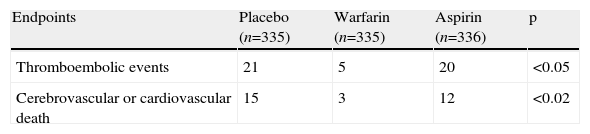
Clinical trials on antithrombotic therapy in atrial fibrillationStudies involving warfarin or other oral anticoagulantsAFASAK I (1989)In the first Copenhagen Atrial Fibrillation, Aspirin, and Anticoagulant Therapy Study (AFASAK I), 1007 patients aged 18 or over with chronic nonvalvular AF documented by electrocardiogram (ECG) were randomized to openly receive warfarin (international normalized ratio [INR] 2.8–4.2, n=335), or, blindly, aspirin (75mg/day, n=336) or placebo (n=336).10 The following were exclusion criteria: cerebrovascular events within the past month, previous anticoagulant therapy for more than six months, hypertension above 180/100mmHg, valvular heart disease, valve replacement, or current therapy or contraindication to aspirin or warfarin treatment. The primary endpoint was stroke, TIA or systemic embolism. The secondary event was death.
The mean follow-up was two years. In the warfarin group, compared to the aspirin group and placebo, there was a significantly lower incidence of embolic complications (5, 20 and 21 events, respectively, p<0.05) and mortality from cardiovascular causes or stroke (3, 12 and 15 events, respectively, p<0.02). The annual incidence of thromboembolic complications was 2.0% with warfarin and 5.5% with aspirin and placebo. Nonfatal bleeding complications occurred in 21 patients with warfarin (7%), in two patients with aspirin (2%) and in no patients on placebo (0%). Some of the main results are shown in Table 1.
Some major findings of the Copenhagen Atrial Fibrillation, Aspirin, and Anticoagulant Therapy Study (AFASAK I).
| Endpoints | Placebo (n=335) | Warfarin (n=335) | Aspirin (n=336) | p |
| Thromboembolic events | 21 | 5 | 20 | <0.05 |
| Cerebrovascular or cardiovascular death | 15 | 3 | 12 | <0.02 |
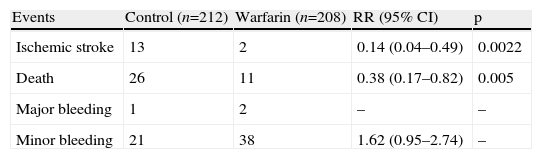
The Boston Area Anticoagulation Trial for Atrial Fibrillation (BAATAF) was an unblinded trial in which 420 adult patients with chronic or paroxysmal nonvalvular AF documented by ECG were randomized to receive low-dose warfarin (n=212; prothrombin-time ratio 1.2 to 1.5, corresponding to an INR between 1.5 and 2.7) or no anticoagulant treatment (n=208; aspirin or nothing).11 Exclusion criteria were intracardiac thrombus, left ventricular aneurysm, severe CHF, valve replacement, stroke in the previous 6 months, increased bleeding risk, planned cardioversion, indication for aspirin therapy or indication or contraindication for anticoagulation. The primary endpoint was ischemic stroke. Systemic embolism was also an endpoint. Bleeding complications and deaths were recorded.
The mean follow-up was 2.2 years. The annual rate of stroke was 2.98% in the placebo group and 0.41% in the warfarin group (RR 0.14, p=0.0022). The annual mortality rate was 5.97% for placebo and 2.25% for warfarin (RR 0.38, p=0.005). There was only one fatal hemorrhage in each group, and three major bleeding events (two with warfarin and one with placebo). There were 38 minor bleeding episodes with warfarin and 21 episodes with placebo (RR 1.62, 95% confidence interval [CI] 0.95–2.74). Some of the main results are shown in Table 2.
Some major findings of the Boston Area Anticoagulation Trial for Atrial Fibrillation (BAATAF).
| Events | Control (n=212) | Warfarin (n=208) | RR (95% CI) | p |
| Ischemic stroke | 13 | 2 | 0.14 (0.04–0.49) | 0.0022 |
| Death | 26 | 11 | 0.38 (0.17–0.82) | 0.005 |
| Major bleeding | 1 | 2 | – | – |
| Minor bleeding | 21 | 38 | 1.62 (0.95–2.74) | – |
CI: confidence interval; RR: risk ratio.
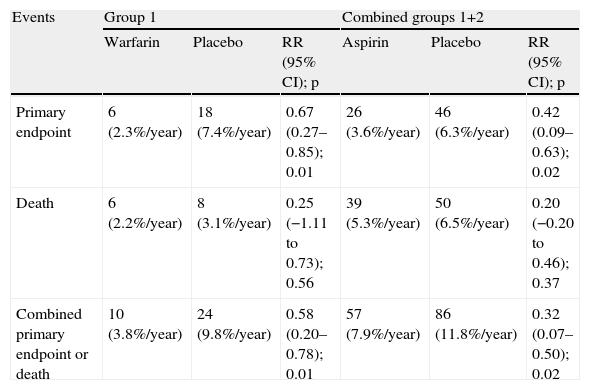
In the Stroke Prevention in Atrial Fibrillation (SPAF) multicenter randomized trial, 1330 patients with permanent or paroxysmal nonvalvular AF diagnosed by ECG 12 months previously were enrolled in order to compare aspirin (325mg daily, double-blind) or warfarin (INR 2.0–4.5) with placebo.12 Patients with ischemic stroke and TIA more than two years before the study were included. Patients were excluded if they had valve replacement, mitral stenosis, or other requirements or contraindication for aspirin or warfarin therapy. Two groups were formed. In group 1, patients received warfarin openly (n=210) or, blindly, aspirin (n=206) or placebo (n=211). In group 2, patients received aspirin (n=346) or placebo (n=357). The primary endpoint was ischemic stroke and systemic embolism.
During a median follow-up of 1.3 years, there was a 42% reduction in the primary event rate in group 2 (3.6%/year [aspirin] vs. 6.3%/year [placebo], p=0.02) and a 67% reduction in group 1 (2.3%/year [warfarin] vs. 7.4%/year [placebo], p=0.01). The primary event and mortality decreased by 58% (p=0.01) with warfarin and 32% (p=0.02) with aspirin. The risk of significant bleeding was similar in all groups. Some of the main results are shown in Table 3.
Some major findings of the Stroke Prevention in Atrial Fibrillation (SPAF) study.
| Events | Group 1 | Combined groups 1+2 | ||||
| Warfarin | Placebo | RR (95% CI); p | Aspirin | Placebo | RR (95% CI); p | |
| Primary endpoint | 6 (2.3%/year) | 18 (7.4%/year) | 0.67 (0.27–0.85); 0.01 | 26 (3.6%/year) | 46 (6.3%/year) | 0.42 (0.09–0.63); 0.02 |
| Death | 6 (2.2%/year) | 8 (3.1%/year) | 0.25 (−1.11 to 0.73); 0.56 | 39 (5.3%/year) | 50 (6.5%/year) | 0.20 (−0.20 to 0.46); 0.37 |
| Combined primary endpoint or death | 10 (3.8%/year) | 24 (9.8%/year) | 0.58 (0.20–0.78); 0.01 | 57 (7.9%/year) | 86 (11.8%/year) | 0.32 (0.07–0.50); 0.02 |
CI: confidence interval; RR: risk reduction.
The Canadian Atrial Fibrillation Anticoagulant Study (CAFA) was stopped before completion of its planned recruitment of 630 patients,13 after the publication of evidence from two different studies10,12 demonstrating the efficacy of warfarin in reducing systemic thromboembolism. In this trial, 187 patients were randomized to warfarin (INR 2–3) and 191 to placebo. The primary outcome events were ischemic stroke (except lacunar), systemic embolism and intracranial or fatal hemorrhage. The results indicated a reduction in the number of primary events in the warfarin group, but none of the results were statistically significant.
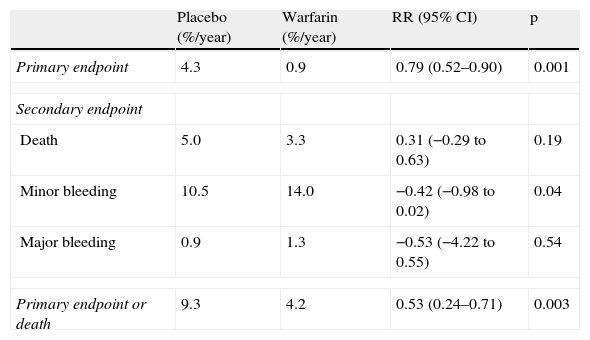
SPINAF (1992)In the Stroke Prevention in Nonrheumatic Atrial Fibrillation (SPINAF) trial,14 a double-blind, randomized, placebo-controlled study, 571 male patients of any age with chronic nonvalvular AF documented by ECG received warfarin (INR 1.2–1.5) or placebo (n=265). Patients were excluded if they had paroxysmal AF and indication for treatment or contraindication to treatment with antiplatelet agents or anticoagulants. The primary endpoint was cerebral infarction and the secondary endpoints were cerebral hemorrhage and death. The mean follow-up was 1.7 years for the placebo group and 1.8 years for the warfarin group.
In the 525 patients without a previous history of stroke, the annual primary event rate was 4.3% in the placebo group (n=265) and 0.9% in the warfarin group (n=260; risk reduction 0.79, p=0.001). In patients over 70 years, the corresponding rate was 4.8% in the placebo group and 0.9% in the warfarin group (risk reduction: 0.79, p=0.02). In the patients with prior stroke, stroke was more common (9.3% for placebo and 6.1% for warfarin; risk reduction 0.40, p=0.63). The only episode of cerebral hemorrhage in patients with no history of previous stroke occurred in a 73-year-old patient in the warfarin group. All other major bleeds were gastrointestinal events, with an annual rate of 0.9% in the placebo group and 1.3% in the warfarin group (p=0.54). The annual minor bleeding rate was 10.5% with placebo and 14.0% with warfarin (p=0.04). In patients without prior stroke, the annual mortality rate was 5.0% with placebo and 3.3% with warfarin (risk reduction 0.3; p=0.19). The risk of stroke or death was 53% lower in the warfarin group (p=0.003). Some of the main results are shown in Table 4.
Some major results of the Stroke Prevention in Nonrheumatic Atrial Fibrillation (SPINAF) trial – group of patients with no history of cerebral infarction.
| Placebo (%/year) | Warfarin (%/year) | RR (95% CI) | p | |
| Primary endpoint | 4.3 | 0.9 | 0.79 (0.52–0.90) | 0.001 |
| Secondary endpoint | ||||
| Death | 5.0 | 3.3 | 0.31 (−0.29 to 0.63) | 0.19 |
| Minor bleeding | 10.5 | 14.0 | −0.42 (−0.98 to 0.02) | 0.04 |
| Major bleeding | 0.9 | 1.3 | −0.53 (−4.22 to 0.55) | 0.54 |
| Primary endpoint or death | 9.3 | 4.2 | 0.53 (0.24–0.71) | 0.003 |
CI: confidence interval; RR: risk reduction.
In the multicenter randomized European Atrial Fibrillation Trial (EAFT),15 1007 patients aged over 25 with nonvalvular AF documented by ECG and with TIA or minor ischemic stroke in the previous three months were divided into two groups. The first group received open anticoagulation with warfarin (INR 2.5–4.0, n=225), or double-blind treatment with either aspirin (300mg/day, n=230) or placebo (n=214). Group 2 included patients with contraindications to anticoagulation, who were randomized to receive double-blind treatment with aspirin (n=174) or placebo (n=164). Exclusion criteria included secondary causes of AF, current antiplatelet or anticoagulant therapy, other cardiac embolic sources (such as prosthetic valves, cardiac aneurysm, atrial myxoma or MI in the preceding three months), and contraindication to, or absolute indication for, aspirin. Patients were excluded from receiving anticoagulant treatment if they had high bleeding risk, hypertension (>180/100mmHg), chronic alcoholism, hemorrhagic retinopathy or previous intracranial hemorrhage. The primary endpoint was death from vascular disease, nonfatal stroke (ischemic and hemorrhagic), nonfatal MI, or systemic embolism. Secondary events were death from all causes, all strokes (fatal and nonfatal) and other major thromboembolic events.
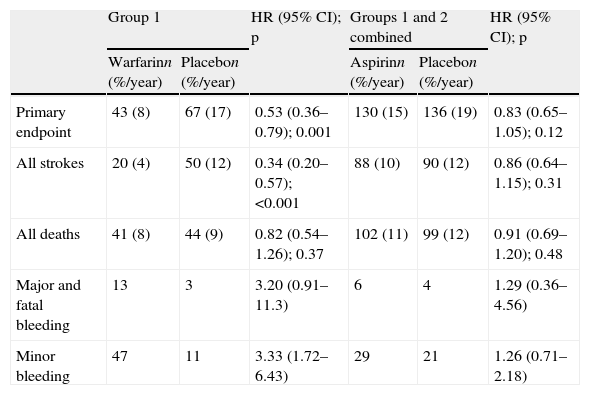
The mean follow-up was 2.3 years. In group 1, the annual primary event rate was 8% with warfarin and 17% with placebo (hazard ratio [HR] 0.53, p=0.001). The risk of stroke was reduced from 12% to 4%/year (HR 0.34, p<0.001). Combining the results of both groups, the annual primary event rate was 15% with aspirin and 19% with placebo (HR 0.83, p=0.12). The annual rate of stroke was 10% with aspirin and 12% with placebo (HR 0.86, p=0.31). Regarding mortality, there was no statistically significant difference between warfarin and placebo (8%/year vs. 9%/year, HR 0.82, p=0.37) or between aspirin and placebo (11%/year vs. 12%/year, HR 0.91, p=0.48). With respect to the primary event, warfarin was more effective than aspirin (HR 0.60, p=0.008), largely due to the decreased rate of stroke (HR 0.38, p<0.001). The annual rate of bleeding was higher with warfarin compared to aspirin (HR 2.8, 95% CI 1.7–4.8, p<0.001) and to placebo (HR 3.4, 95% CI 1.9–6.0, p<0.001). Some of the main results are shown in Table 5.
Some major results of the European Atrial Fibrillation Trial (EAFT).
| Group 1 | HR (95% CI); p | Groups 1 and 2 combined | HR (95% CI); p | |||
| Warfarinn (%/year) | Placebon (%/year) | Aspirinn (%/year) | Placebon (%/year) | |||
| Primary endpoint | 43 (8) | 67 (17) | 0.53 (0.36–0.79); 0.001 | 130 (15) | 136 (19) | 0.83 (0.65–1.05); 0.12 |
| All strokes | 20 (4) | 50 (12) | 0.34 (0.20–0.57); <0.001 | 88 (10) | 90 (12) | 0.86 (0.64–1.15); 0.31 |
| All deaths | 41 (8) | 44 (9) | 0.82 (0.54–1.26); 0.37 | 102 (11) | 99 (12) | 0.91 (0.69–1.20); 0.48 |
| Major and fatal bleeding | 13 | 3 | 3.20 (0.91–11.3) | 6 | 4 | 1.29 (0.36–4.56) |
| Minor bleeding | 47 | 11 | 3.33 (1.72–6.43) | 29 | 21 | 1.26 (0.71–2.18) |
CI: confidence interval; HR: hazard ratio.
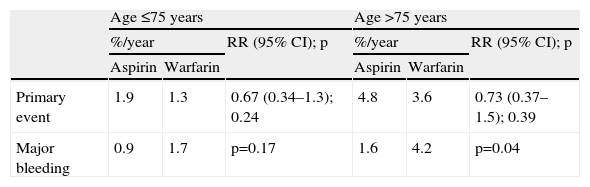
In the multicenter, randomized, unblinded Stroke Prevention in Atrial Fibrillation II study (SPAFII), 715 adult patients aged 75 years or less and 385 patients aged over 75 years with nonvalvular AF documented by ECG were enrolled to receive aspirin (325mg/day) or warfarin (INR 2.0–4.5).16 Patients were excluded if they had prosthetic heart valves, mitral stenosis, or requirements for or contraindication to warfarin or aspirin, lone AF in patients under 60 years old, or ischemic stroke or TIA in the previous two years. The primary event was ischemic stroke and systemic embolism in n patients aged 75 or less, the annual primary event rate was 1.9% with aspirin and 1.3% with warfarin (RR 0.67, p=0.24, mean prothrombin time ratio=1.5). In patients older than 75 years, the annual primary event rate was 4.8% with aspirin and 3.6% with warfarin (RR 0.73, p=0.39), mean prothrombin (time ratio=1.4). The overall annual primary event rate was 2.7% with aspirin and 1.9% with warfarin (RR 0.70, p=0.15). Patients with risk factors for thromboembolism (history of hypertension, prior thromboembolism, recent heart failure) assigned to aspirin had a higher primary event rate than those without risk factors (p<0.001). In patients aged 75 or less, the annual major bleeding rate was 0.9% with aspirin and 1.7% with warfarin (p=0.17) and in patients over 75 years, the annual bleeding rate was respectively 1.6% and 4.2% (p=0.04). The major bleeding rate with warfarin was higher in older patients, despite similar intensity of coagulation (p=0.008). The rate of intracranial hemorrhage (ICH) was higher in patients aged over 75 with warfarin than in younger patients (1.8% vs. 0.5%, p=0.05). Some of the main results are shown in Table 6.
Some major results of the Stroke Prevention in Atrial Fibrillation II study (SPAF II).
| Age ≤75 years | Age >75 years | |||||
| %/year | RR (95% CI); p | %/year | RR (95% CI); p | |||
| Aspirin | Warfarin | Aspirin | Warfarin | |||
| Primary event | 1.9 | 1.3 | 0.67 (0.34–1.3); 0.24 | 4.8 | 3.6 | 0.73 (0.37–1.5); 0.39 |
| Major bleeding | 0.9 | 1.7 | p=0.17 | 1.6 | 4.2 | p=0.04 |
CI: confidence interval; RR: relative risk.
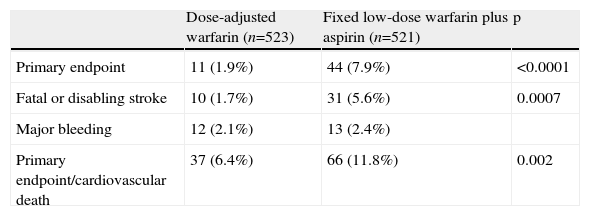
This study (Stroke Prevention in Atrial Fibrillation III) randomized 1044 patients with AF and at least one thromboembolic risk factor to openly receive fixed low-dose warfarin (0.5–3.0mg/day, INR 1.2–1.5) plus aspirin (325mg/day) (n=521), or adjusted-dose warfarin (INR 2.0–3.0, n=523).17 Selection criteria included the presence of AF diagnosed six months earlier and at least one of the following: CHF or left ventricular fractional shortening≤25%, TIA, previous ischemic stroke or systemic embolism (in the previous 30 days), systolic blood pressure higher than 160mmHg, or female gender over 75 years old. Patients were excluded if they had valve replacement, mitral stenosis, indication or contraindication to the use of warfarin or aspirin, or inability to give informed consent. The primary endpoint was stroke and systemic embolism and the secondary events were major bleeding and death.
The study was stopped after a median follow-up of 1.1 years due to a higher rate of ischemic stroke and systemic embolism in the group with combined therapy (7.9%/year vs. 1.9%/year; p<0.0001). The same conclusions were found for the annual rates of disabling or fatal stroke (5.6%/year vs. 1.7%/year, p=0.0007) and rates of primary event or death from cardiovascular causes (11.8%/year vs. 6.4%/year, p=0.002). The major bleeding rate was similar in both groups (2.4%/year for the group with combined therapy vs. 2.1%/year for the warfarin group). The mean INR in the combined therapy group was 1.3 compared to 2.4 in the group with adjusted-dose warfarin. Some of the main results are shown in Table 7.
Some major results of the Stroke Prevention in Atrial Fibrillation III (SPAF III) trial.
| Dose-adjusted warfarin (n=523) | Fixed low-dose warfarin plus aspirin (n=521) | p | |
| Primary endpoint | 11 (1.9%) | 44 (7.9%) | <0.0001 |
| Fatal or disabling stroke | 10 (1.7%) | 31 (5.6%) | 0.0007 |
| Major bleeding | 12 (2.1%) | 13 (2.4%) | |
| Primary endpoint/cardiovascular death | 37 (6.4%) | 66 (11.8%) | 0.002 |
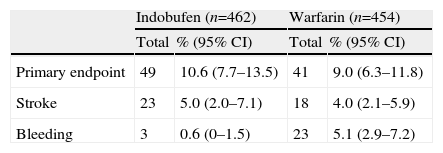
In this multicenter study (Studio Italiano Fibrilazzione Atriale),18 916 patients aged over 30 with chronic or paroxysmal nonvalvular atrial fibrillation and a recent episode (in the previous 15 days) of cerebral ischemia (TIA or stroke), were randomized to receive indobufen (462 patients, 100mg [if creatinine clearance <80ml/min] or 200mg) or warfarin (454 patients, INR=2–3.5) over 12 months. Exclusion criteria included rheumatic or congenital valvular disease, valvular prostheses, cardioversion in the previous two weeks, intracardiac thrombus or tumor, left ventricular aneurysm, heart failure (NYHA class >III), MI or unstable angina in the previous month, severe hypertension, and carotid endarterectomy or coronary or peripheral revascularization procedures in the previous six months. The primary endpoint was nonfatal stroke (ischemic and hemorrhagic), systemic embolism, nonfatal MI and death from cardiovascular causes.
The incidence of the primary outcome was 10.6% for the indobufen group and 9% in the warfarin group, with no statistically significant difference between the groups. The incidence of noncerebral bleeding was 0.6% for the indobufen group and 5.1% in the warfarin group, the difference being statistically significant (p<0.01). Some of the main results are shown in Table 8.
Some major results of the Studio Italiano Fibrilazzione Atriale (SIFA).
| Indobufen (n=462) | Warfarin (n=454) | |||
| Total | % (95% CI) | Total | % (95% CI) | |
| Primary endpoint | 49 | 10.6 (7.7–13.5) | 41 | 9.0 (6.3–11.8) |
| Stroke | 23 | 5.0 (2.0–7.1) | 18 | 4.0 (2.1–5.9) |
| Bleeding | 3 | 0.6 (0–1.5) | 23 | 5.1 (2.9–7.2) |
CI: confidence interval.
The second Copenhagen Atrial Fibrillation, Aspirin, and Anticoagulant Therapy Study (AFASAK II)19 was terminated prematurely after the publication of evidence from a different study17 demonstrating the ineffectiveness of low-intensity anticoagulation plus aspirin. In this trial, 677 patients with chronic nonvalvular AF were randomized to receive, unblinded, fixed low-dose warfarin (1.25mg/day), fixed low-dose warfarin (1.25mg/day) plus aspirin (300mg/day), aspirin (300mg/day) or adjusted-dose warfarin (INR 2.0–3.0). The cumulative primary event rate (stroke or systemic thromboembolic event) after one year was 5.8%, 7.2%, 3.6% and 2.8% for fixed low-dose warfarin, warfarin plus aspirin, aspirin, and adjusted-dose warfarin, respectively (p=0.67). The cumulative mortality rate after three years was 3.9%, 5.9%, 13.4% and 10.3%, respectively (p=0.27).
In another report from the same study20 to an evaluation was carried out of bleeding events. During treatment with fixed low-dose warfarin, warfarin plus aspirin, aspirin, and adjusted-dose warfarin, the annual major bleeding rate was 0.8%, 0.3%, 1.4% and 1.1%, respectively (p=0.20). After three years of treatment, the cumulative bleeding rate was 24.7%, 24.4%, 30.0% and 41.1%, respectively (p=0.003).
Minidose Warfarin in Nonrheumatic Atrial Fibrillation (1998)This study was stopped early after the publication of evidence17 indicating that low-dose warfarin puts patients at high risk of stroke compared to those with an INR adjusted to 2–3. In this open-labeled multicenter study,21 303 patients aged over 60 and with chronic nonrheumatic AF were randomized to receive fixed low-dose (1.25mg/day) or adjusted-dose warfarin (INR 2–3). The primary event rate was 6.2% for the fixed low-dose warfarin and 3.6% in the group with adjusted-dose warfarin (p=0.29). The rate of ischemic stroke was higher in the group with fixed low-dose warfarin (3.7%/year vs. 0%/year, p=0.025). Major bleeding occurred in 2.6%/year in the group with adjusted-dose warfarin and 1%/year in the group with fixed low-dose warfarin (p=0.19).
PATAF (1999)In the Primary prevention of Arterial Thromboembolism in nonrheumatic Atrial Fibrillation (PATAF) trial,22 729 patients aged over 60 years with chronic or paroxysmal AF, diagnosed by ECG up to two years prior to selection, were divided into two groups. Patients in group 1 were randomized to receive adjusted-dose anticoagulant (n=131, INR 2.5–3.5), low-dose anticoagulant (n=122, INR 1.1–1.6) or aspirin (n=141, 150mg/day). Patients in group 2 received aspirin (n=178, 150mg/day) or low-dose anticoagulant (n=157, INR 1.1–1.6). The following were exclusion criteria: AF with a treatable cause, previous stroke, rheumatic valvular disease, MI or cardiovascular surgery in the previous year, cardiomyopathy (left ventricular ejection fraction [LVEF] <40%), chronic heart failure, previous systemic embolism, coumarin use in the previous 3 months, contraindication to aspirin or coumarin, life expectancy less than 2 years and the presence of a pacemaker. Patients were excluded from standard anticoagulation if they were older than 78, or had retinopathy, duodenal ulcer, history of gastrointestinal or genitourinary bleeding, or hypertension (>185/105mmHg). The primary endpoint was ischemic or hemorrhagic stroke, systemic embolism, major bleeding and vascular death. Secondary outcome events were nonfatal MI, retinal infarction, TIA, minor bleeding or non-vascular death.
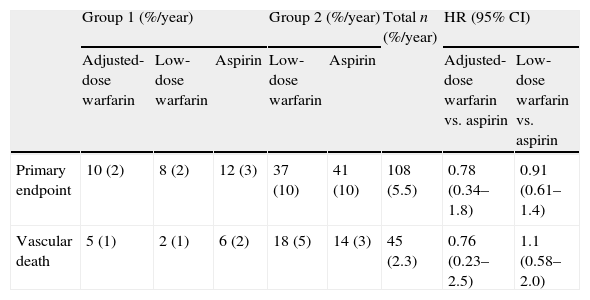
There were 108 primary events (annual rate of 5.5%), with no significant differences between patients with dose-adjusted (HR 0.78, 95% CI 0.34–1.8) or low-dose anticoagulant therapy (HR 0.91, 95% CI 0.61–1.4) compared to aspirin. There were 45 deaths from vascular causes (annual rate of 2%) and there were also no significant differences between patients with dose-adjusted anticoagulant therapy (HR 0.76, 95% CI 0.23–2.5) or low-dose therapy (HR 1.1, 95% CI 0.58–2.0) compared to aspirin. The annual rate of bleeding was 3.9%, with no significant differences between patients with dose-adjusted (HR 1.3, 95% CI 0.59–3.0) or with low-dose anticoagulation (HR 1.02, 95% CI 0.58–1.8) compared to aspirin. Some of the main results are shown in Table 9.
Some major results of the Primary prevention of Arterial Thromboembolism in nonrheumatic Atrial Fibrillation (PATAF) trial.
| Group 1 (%/year) | Group 2 (%/year) | Total n (%/year) | HR (95% CI) | |||||
| Adjusted-dose warfarin | Low-dose warfarin | Aspirin | Low-dose warfarin | Aspirin | Adjusted-dose warfarin vs. aspirin | Low-dose warfarin vs. aspirin | ||
| Primary endpoint | 10 (2) | 8 (2) | 12 (3) | 37 (10) | 41 (10) | 108 (5.5) | 0.78 (0.34–1.8) | 0.91 (0.61–1.4) |
| Vascular death | 5 (1) | 2 (1) | 6 (2) | 18 (5) | 14 (3) | 45 (2.3) | 0.76 (0.23–2.5) | 1.1 (0.58–2.0) |
CI: confidence interval; HR: hazard ratio.
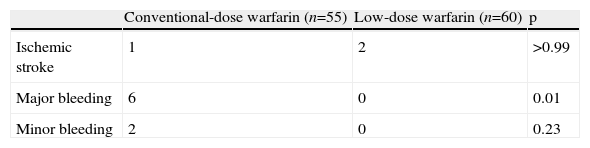
This study (by the Japanese Nonvalvular Atrial Fibrillation-Embolism Secondary Prevention Cooperative Study Group) randomized 115 patients younger than 80 years old with nonvalvular AF and with a history of stroke or TIA (1–6 months previously) to receive conventional-dose warfarin (INR 2.2–3.5, n=55) or low-dose warfarin (INR 1.5–2.1, n=60).23 Exclusion criteria included intracardiac thrombus, left ventricular aneurysm, CHF (NYHA class IV), heart valve disease, previous episode of ICH, severe kidney or liver disease and cancer. The primary endpoint was stroke, systemic embolism, TIA and amaurosis fugax, and the secondary event was bleeding.
The study was stopped after a median follow-up of 658±423 days, due to the occurrence of major bleeding complications in six patients with conventional-dose warfarin, which represents an occurrence rate of 6.6% per year, compared to 0%/year in patients treated with low-dose warfarin. These six patients, with a mean age of 73.7±3.7 years, had an INR within the range established prior to the events (median INR=2.8). The annual rate of recurrent ischemic stroke was low in both groups (1.1% with conventional-dose and 1.7% with low-dose warfarin, p>0.99). Some of the main results are shown in Table 10.
Some major results of the Japanese Nonvalvular Atrial Fibrillation–Embolism Secondary Prevention Cooperative Group.
| Conventional-dose warfarin (n=55) | Low-dose warfarin (n=60) | p | |
| Ischemic stroke | 1 | 2 | >0.99 |
| Major bleeding | 6 | 0 | 0.01 |
| Minor bleeding | 2 | 0 | 0.23 |
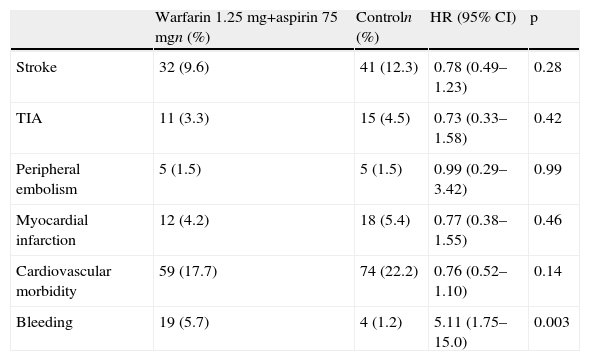
In the open multicenter Swedish Atrial Fibrillation Trial,24 668 patients aged over 60 with persistent or permanent nonvalvular AF were randomized to receive fixed-dose warfarin (1.25mg) plus aspirin (75mg, n=334), or no antithrombotic treatment (n=334). Exclusion criteria were prior stroke or TIA, heart valve prosthesis, cardiac valvular disease, hypertension (>190/110mmHg), reversible causes of atrial fibrillation, severe heart failure (NYHA III-IV), hypertension, bradycardia, renal failure, liver disease, chronic obstructive pulmonary disease, bleeding disorder, and indication for or contraindication to anticoagulation or antiplatelet agents. The primary endpoint was stroke and secondary endpoints were death from any cause, cardiovascular morbidity, TIA, MI, peripheral embolism and bleeding.
The mean follow-up was 33 months. The rate of stroke was 9.6% with combined therapy and 12.3% in controls (HR 0.78, p=0.28). The rate of TIA was 3.3% with combined therapy and 4.5% in controls (HR 0.73, p=0.42) while the rate of MI was 4.2% with combined therapy and 5.4% in controls (HR 0.77, p=0.46). During follow-up there were 63 deaths, 9.3% in the group treated with antithrombotics and 10.8% in the untreated group (p=0.55). Bleeding was more frequent with combined therapy (5.7% vs. 1.2%, p=0.003). Some of the main results are shown in Table 11.
Major results of the Swedish Atrial Fibrillation Trial (SAFT) study.
| Warfarin 1.25mg+aspirin 75mgn (%) | Controln (%) | HR (95% CI) | p | |
| Stroke | 32 (9.6) | 41 (12.3) | 0.78 (0.49–1.23) | 0.28 |
| TIA | 11 (3.3) | 15 (4.5) | 0.73 (0.33–1.58) | 0.42 |
| Peripheral embolism | 5 (1.5) | 5 (1.5) | 0.99 (0.29–3.42) | 0.99 |
| Myocardial infarction | 12 (4.2) | 18 (5.4) | 0.77 (0.38–1.55) | 0.46 |
| Cardiovascular morbidity | 59 (17.7) | 74 (22.2) | 0.76 (0.52–1.10) | 0.14 |
| Bleeding | 19 (5.7) | 4 (1.2) | 5.11 (1.75–15.0) | 0.003 |
CI: confidence interval; HR: hazard ratio.
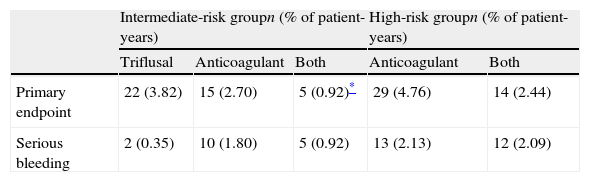
In this multicenter open-label study (National Study for Prevention of Embolism in Atrial Fibrillation),25 1209 patients with chronic or paroxysmal AF were randomized in two groups. The high-risk group included patients without mitral stenosis and with previous embolism or patients with mitral stenosis with or without prior embolism. The remaining patients were included in an intermediate risk group (patients with risk factors or aged over 60 years). In the intermediate risk group, 242 patients received triflusal (600mg/day), 237 received acenocoumarol (INR 2–3) and 235 received a combination of both drugs (INR 1.25–2). In the high-risk group, 259 patients received acenocoumarol (INR 2–3) and 236 patients received combined therapy (INR of 1.4–2.4). Patients were excluded if they had mechanical valve prosthesis, stroke within the previous 6 months, serum creatinine >3mg/dl, alcohol or drug abuse, severe uncontrolled hypertension, diffuse arteriosclerosis, indication for therapy with anti-inflammatory drugs or indication for or contraindication to antiplatelet or anticoagulant therapy. The primary endpoint was death from cardiovascular causes, TIA, nonfatal stroke or systemic embolism.
The mean follow-up was 2.76 years. In the intermediate-risk group, there was a lower incidence of the primary outcome with combined therapy compared to the group with triflusal (HR 0.24, p=0.001) and to the acenocoumarol group (HR 0.33, p=0.02). There was no significant difference between the acenocoumarol and triflusal groups (HR 0.72, p=0.32). Regarding the high-risk group, combined therapy led to a 49% reduction in the primary event rate compared to therapy with acenocoumarol (HR 0.51, p=0.03). Patients in the intermediate-risk group treated with triflusal had a significantly lower bleeding risk than patients treated with acenocoumarol or combined therapy. Patients with mitral stenosis and anticoagulant treatment of embolism had similar rates of embolism, compared to patients without valvular pathology. Some of the main results are shown in Table 12.
Major results of the National Study for Prevention of Embolism in Atrial Fibrillation (NASPEAF).
| Intermediate-risk groupn (% of patient-years) | High-risk groupn (% of patient-years) | ||||
| Triflusal | Anticoagulant | Both | Anticoagulant | Both | |
| Primary endpoint | 22 (3.82) | 15 (2.70) | 5 (0.92)* | 29 (4.76) | 14 (2.44) |
| Serious bleeding | 2 (0.35) | 10 (1.80) | 5 (0.92) | 13 (2.13) | 12 (2.09) |
Ximelagatran is an oral direct thrombin inhibitor. Although it had shown promising results,26,27 with similar antithrombotic efficacy to warfarin, research on this drug has ceased because of its potential hepatotoxicity. The SPORTIF III and SPORTIF V clinical trials, although of historical interest concerning antithrombotic therapy of AF, will therefore not be described here due to space limitations.
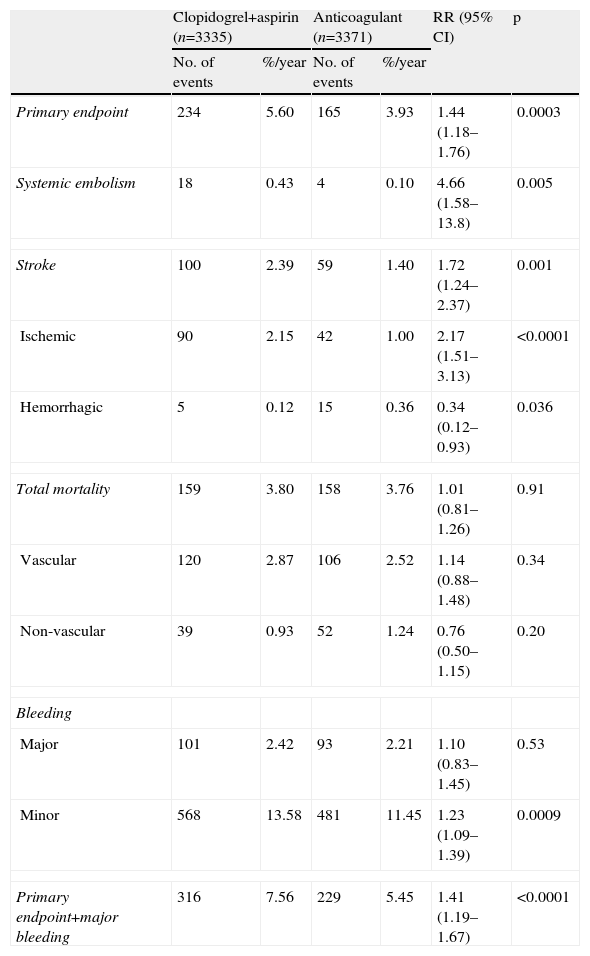
ACTIVE-W (2006)In this open study (Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events),28 6706 patients were randomized to receive oral anticoagulant therapy (OAC) (n=3371; INR 2.0–3.0) or clopidogrel (75mg daily) in combination with aspirin (75–100mg/day, n=3335). Selection criteria included the presence of AF and of at least one of the following characteristics: age ≥75 years; undergoing treatment for arterial hypertension; previous TIA, stroke or systemic embolism; LVEF<45%; peripheral arterial disease; age between 55 and 74 years; and diabetes or CAD. Patients were excluded if they had a contraindication to clopidogrel or OAC, peptic ulcer disease in the previous 6 months, prior ICH, significant thrombocytopenia or mitral stenosis. The primary endpoint was stroke, systemic embolism, MI and death from cardiovascular causes.
The mean follow-up was 1.28 years. The study was discontinued due to clear evidence of the superiority of OAC. There were 165 primary events in patients with OAC (annual risk 3.90%) and 234 events in patients with combined antiplatelet therapy (annual risk 5.60%, RR 1.44, p=0.0003). The risk reduction with OAC therapy was more evident in the prevention of stroke (RR 1.72 with clopidogrel+aspirin, p=0.001) and systemic embolism (RR 4.66 with clopidogrel+aspirin, p=0.005). The rate of MI was less than 1% in both groups. There were no significant differences between the mortality rates in the two groups. The combination of the primary event and major bleeding was more favorable with OAC (RR 1.41 with clopidogrel+aspirin, p<0.0001). The major bleeding rates were similar between the two groups, but minor bleeding were more frequent with combination therapy (RR 1.23, p=0.0009). Patients with OAC who had received this treatment prior to the study (77%) had a greater reduction in cardiovascular events (RR 1.50 with clopidogrel+aspirin, 95% CI 1.19–1.80) and a significantly lower risk of major bleeding (p=0.03). Some of the main results are shown in Table 13.
Major results from the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE-W) study.
| Clopidogrel+aspirin (n=3335) | Anticoagulant (n=3371) | RR (95% CI) | p | |||
| No. of events | %/year | No. of events | %/year | |||
| Primary endpoint | 234 | 5.60 | 165 | 3.93 | 1.44 (1.18–1.76) | 0.0003 |
| Systemic embolism | 18 | 0.43 | 4 | 0.10 | 4.66 (1.58–13.8) | 0.005 |
| Stroke | 100 | 2.39 | 59 | 1.40 | 1.72 (1.24–2.37) | 0.001 |
| Ischemic | 90 | 2.15 | 42 | 1.00 | 2.17 (1.51–3.13) | <0.0001 |
| Hemorrhagic | 5 | 0.12 | 15 | 0.36 | 0.34 (0.12–0.93) | 0.036 |
| Total mortality | 159 | 3.80 | 158 | 3.76 | 1.01 (0.81–1.26) | 0.91 |
| Vascular | 120 | 2.87 | 106 | 2.52 | 1.14 (0.88–1.48) | 0.34 |
| Non-vascular | 39 | 0.93 | 52 | 1.24 | 0.76 (0.50–1.15) | 0.20 |
| Bleeding | ||||||
| Major | 101 | 2.42 | 93 | 2.21 | 1.10 (0.83–1.45) | 0.53 |
| Minor | 568 | 13.58 | 481 | 11.45 | 1.23 (1.09–1.39) | 0.0009 |
| Primary endpoint+major bleeding | 316 | 7.56 | 229 | 5.45 | 1.41 (1.19–1.67) | <0.0001 |
CI: confidence interval; RR: relative risk.
In this randomized study, carried out in 704 Chinese patients with nonvalvular AF, adjusted-dose warfarin (INR 2.0–3.0) was shown to significantly reduce thromboembolic risk compared to 150–160mg/day aspirin.29 The median follow-up was 19 months. Death or ischemic stroke was reduced by warfarin (2.7% vs. 6.0%, p=0.03) and relative risk decreased by 56%. However, there was no significant difference in mortality, and warfarin treatment was associated with an increased bleeding rate (6.9% vs. 2.4%, p<0.05).
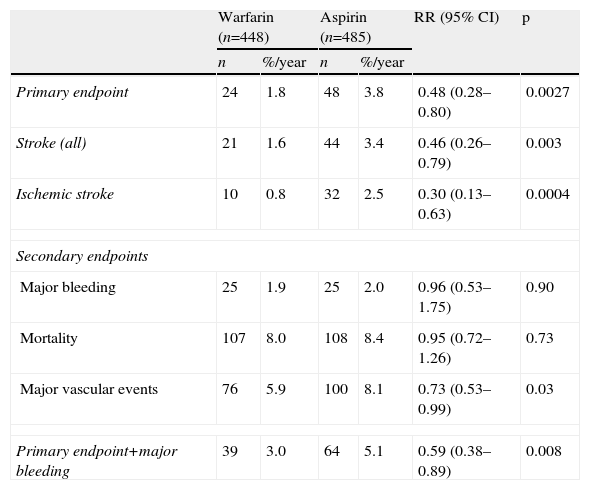
BAFTA (2007)In the open-label Birmingham Atrial Fibrillation treatment of the Aged Study,30 973 patients over 75 years of age followed in primary care and with AF diagnosed by ECG were randomized to receive warfarin (INR 2–3) or aspirin (75mg/day). Patients were excluded if they had rheumatic heart disease, major nontraumatic hemorrhage in the previous five years, ICH, peptic disease in the previous year, esophageal varices, allergic hypersensitivity to warfarin or aspirin, terminal illness, surgery in the previous three months or hypertension (>180/110mmHg). The primary endpoint was fatal or disabling stroke (ischemic or hemorrhagic) and systemic embolism. The secondary events were major extracranial bleeding, other major vascular events (stroke, MI, pulmonary embolism and death from cardiovascular causes) and death. Evaluation of the events was blinded.
The mean follow-up was 2.7 years. The primary event rate was 1.8% in the warfarin group and 3.8% in the aspirin group (RR 0.48, p=0.0027). There was a decrease in the incidence of ischemic stroke in the warfarin group (0.8% vs. 2.5%, p=0.0004). Major vascular events were less frequent in the warfarin group (5.9% vs. 8.1%, RR 0.73, p=0.03). The combination of the primary event with major bleeding was also less frequent in the warfarin group (3.0% vs. 5.1%, RR 0.59, p=0.008). There were no significant differences between warfarin and aspirin regarding total mortality (8.0% vs. 8.4%, p=0.73) or major bleeding (1.9% vs. 2.0%, p=0.90). Some of the main results are shown in Table 14.
Major results from the Birmingham Atrial Fibrillation treatment of the Aged (BAFTA) Study.
| Warfarin (n=448) | Aspirin (n=485) | RR (95% CI) | p | |||
| n | %/year | n | %/year | |||
| Primary endpoint | 24 | 1.8 | 48 | 3.8 | 0.48 (0.28–0.80) | 0.0027 |
| Stroke (all) | 21 | 1.6 | 44 | 3.4 | 0.46 (0.26–0.79) | 0.003 |
| Ischemic stroke | 10 | 0.8 | 32 | 2.5 | 0.30 (0.13–0.63) | 0.0004 |
| Secondary endpoints | ||||||
| Major bleeding | 25 | 1.9 | 25 | 2.0 | 0.96 (0.53–1.75) | 0.90 |
| Mortality | 107 | 8.0 | 108 | 8.4 | 0.95 (0.72–1.26) | 0.73 |
| Major vascular events | 76 | 5.9 | 100 | 8.1 | 0.73 (0.53–0.99) | 0.03 |
| Primary endpoint+major bleeding | 39 | 3.0 | 64 | 5.1 | 0.59 (0.38–0.89) | 0.008 |
CI: confidence interval; RR: relative risk.
This randomized open-label prospective study was designed to evaluate the differences between risks and benefits of adjusted-dose warfarin (INR 2.0–3.0) and aspirin 300mg/day in octogenarians.31 A total of 75 octogenarian patients were included (36 to receive warfarin and 39 to receive aspirin), ambulant and diagnosed as having permanent AF. Patients were excluded if they had any of the following: history of falls or syncopal episode within the previous 12 months; epileptiform seizures; alcoholic liver disease; previous history of thromboembolism; gastrointestinal or genitourinary bleeding in the previous six months; previous intracranial hemorrhage; blood pressure >180/100mmHg; abnormal prothrombin time; Folstein mini mental state score <26; previous intolerance/allergy to warfarin or aspirin; patients already taking warfarin. The follow-up was 12 months and the primary outcome included death, thromboembolism, serious bleeding and withdrawal from the study. There were no significant differences between the two groups regarding the primary outcome. A total of 17 patients reached an endpoint in the aspirin group vs. 9 patients in the warfarin group (p=0.114). However there were significantly fewer adverse reactions with warfarin than with aspirin (p=0.002) and adherence to treatment was equivalent. There was no serious bleeding in the warfarin group, in contrast to aspirin (three events).
Amadeus (2008)In this study,32 subcutaneous idraparinux (a long-acting activated coagulation factor X inhibitor; 2.5mg/week) was compared to adjusted-dose vitamin K antagonists (INR 2–3), in patients with nonvalvular AF. The trial was terminated because of excess bleeding in the idraparinux group.
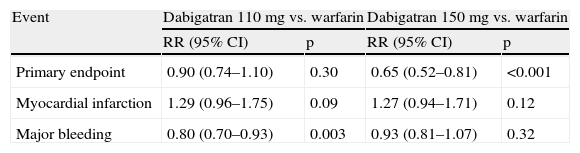
RE-LY (2009)In this clinical trial (Randomized Evaluation of Long-Term Anticoagulation Therapy),33 18113 patients with AF were randomized to receive fixed-dose dabigatran (a direct thrombin inhibitor; 110mg or 150mg twice daily) or warfarin (doses of 1, 3 or 5mg; adjusted to obtain an INR between 2.0–3.0). An update of major results was published in 2010.34 Selection criteria included the presence of AF diagnosed by ECG at the time of selection or in the previous six months and at least one of the following: prior TIA or stroke; LVEF <40%; NYHA class II or symptoms of severe heart failure less than 6 months prior to selection; age ≥75 years or between 65 and 74 years; and diabetes, hypertension or CAD. Patients were excluded if they had severe valvular heart disease, stroke in the previous 14 days, increased bleeding risk, creatinine clearance <30ml/min, active liver disease or pregnancy. The primary endpoint was stroke or systemic embolism.
The mean follow-up was 2 years. The annual rate of the primary outcome was 1.71% with warfarin, 1.54% with 110mg dabigatran (RR 0.90, p=0.30) and 1.11% with 150mg dabigatran (RR 0.65 compared with warfarin, p<0.001).34 The annual rate of MI was 0.64% with warfarin, 0.82% with 110mg dabigatran (RR 1.29, p=0.09) and 0.81% with 150mg dabigatran (RR 1.27, p=0.12). The annual major bleeding rate was 3.57% with warfarin, 2.87% with 110mg dabigatran (RR 0.80, p=0.003) and 3.32% with 150mg dabigatran (RR 0.93, p=0.32).
In the 2009 report, the following findings were presented: (1) The annual mortality rate from cardiovascular causes was 2.69% with warfarin, 2.43% with 110mg dabigatran (RR 0.90, p=0.21) and 2.28% with 150mg dabigatran (RR 0.85, p=0.04); (2) The annual rate of hemorrhagic stroke was 0.38% with warfarin, 0.12% with 110mg dabigatran (RR 0.31, p<0.001) and 0.10% with 150mg dabigatran (RR 0.26, p<0.001); (3) There was a higher rate of major gastrointestinal bleeding with 150mg dabigatran (1.51%/year) compared to warfarin (1.02%/year) (RR 1.50, p<0.001); (4) Compared to 110mg dabigatran, 150mg led to a greater reduction in the risk of stroke or systemic embolism (p=0.005); (5) There was no significant difference between the rate of cardiovascular death (p=0.44) or death from any cause (p=0.66); (6) However, 150mg dabigatran was associated with an increased risk of major (p=0.052), minor (p<0.001), gastrointestinal (p=0.007) and any bleeding33; (7) Dyspepsia occurred in 5.8% of patients treated with warfarin, 11.8% in those treated with 110mg dabigatran and 11.3% in those treated with 150mg dabigatran (p<0.001 for both comparisons); (8) There were no significant modifications in creatinine clearance in the groups with dabigatran; (9) The incidence of alanine aminotransferase and aspartate aminotransferase elevated three times above the normal limit was similar in all groups.33 Some of the main results are shown in Table 15.
Major results of the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) study.
| Event | Dabigatran 110mg vs. warfarin | Dabigatran 150mg vs. warfarin | ||
| RR (95% CI) | p | RR (95% CI) | p | |
| Primary endpoint | 0.90 (0.74–1.10) | 0.30 | 0.65 (0.52–0.81) | <0.001 |
| Myocardial infarction | 1.29 (0.96–1.75) | 0.09 | 1.27 (0.94–1.71) | 0.12 |
| Major bleeding | 0.80 (0.70–0.93) | 0.003 | 0.93 (0.81–1.07) | 0.32 |
CI: confidence interval; RR: relative risk.
In a further report from the same study,35 the effects of dabigatran were studied in relation to the time in therapeutic range (TTR) for warfarin reached in each centre. The effects of dabigatran “vs. warfarin were consistent irrespective of centres’ quality of INR control”. The authors also noted that the “advantages of dabigatran were greater at sites with poor INR control than at those with good INR control”.
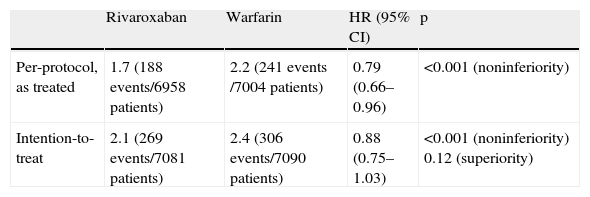
ROCKET-AF (2011)The “Rivaroxaban once-daily oral direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation” study was a randomized, double-blind, double-dummy trial.36 Patients were included if they had at least two risk factors (heart failure, hypertension, age 75 years or over, diabetes), or a past history of stroke, TIA or systemic embolism. Patients (14264) were randomized to take either rivaroxaban (20mg/day, or 15mg in patients with creatinine clearance of 30–49ml/min), or warfarin (INR target of 2.0–3.0). The mean age of the patients was 73 years. The primary endpoint was stroke or systemic embolism; in the per-protocol, as-treated population analysis (rivaroxaban 6958 patients, warfarin 7004 patients), “stroke or systemic embolism occurred in 188 patients in the rivaroxaban group (1.7% per year) and in 241 patients in the warfarin group (2.2% per year) (HR in the rivaroxaban group, 0.79; 95% CI 0.66–0.96; p<0.001 for noninferiority)”36; in the intention-to-treat population (rivaroxaban 7081 patients, warfarin 7090 patients), “primary events occurred in 269 patients in the rivaroxaban group (2.1% per year) and in 306 patients in the warfarin group (2.4% per year) (HR 0.88; 95% CI 0.74–1.03; p<0.001 for noninferiority; p=0.12 for superiority)”36 (Table 16). Secondary efficacy outcomes included the following: myocardial infarction occurred in 101 patients under rivaroxaban therapy, compared to 126 patients in the warfarin group; 208 patients died in the rivaroxaban group, compared to 250 deaths in the warfarin group (as-treated safety population; both comparisons were non-significantly different). The incidence of major and clinically relevant nonmajor bleeding was not significantly different in the two groups, but intracranial hemorrhage and fatal bleeding were less common with rivaroxaban, whereas major bleeding from a gastrointestinal site was more common with rivaroxaban.
Major findings of the ROCKET-AF study. Primary endpoint of stroke or systemic embolism. Event rates per 100 patient-years.
| Rivaroxaban | Warfarin | HR (95% CI) | p | |
| Per-protocol, as treated | 1.7 (188 events/6958 patients) | 2.2 (241 events /7004 patients) | 0.79 (0.66–0.96) | <0.001 (noninferiority) |
| Intention-to-treat | 2.1 (269 events/7081 patients) | 2.4 (306 events/7090 patients) | 0.88 (0.75–1.03) | <0.001 (noninferiority) 0.12 (superiority) |
CI: confidence interval; HR: hazard ratio.
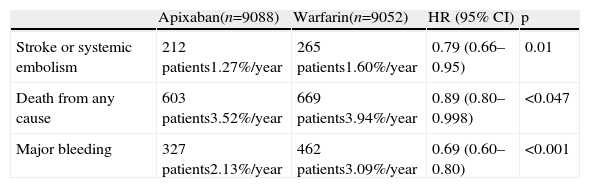
The “Apixaban for reduction in stroke and other thromboembolic events in atrial fibrillation” study was a randomized, double-blind, double-dummy trial.37 Patients were included if they had at least one risk factor (age at least 75 years; previous stroke, TIA or systemic embolism; heart failure; diabetes; hypertension). Patients (18201) with atrial fibrillation were randomized to take either apixaban (a direct factor Xa inhibitor; 5mg twice daily, or 2.5mg in patients with two or more of the following criteria: age at least 80 years, body weight no more than 60kg, plasma creatinine 1.5mg/dl or more; 9120 patients), or warfarin (INR target of 2.0–3.0; 9081 patients). The mean age of the patients was 70 years. The primary endpoint was stroke or systemic embolism, and this endpoint “occurred in 212 patients in the apixaban group (1.27% per year) as compared with 265 patients in the warfarin group (1.60% per year) (HR in the apixaban group, 0.79; 95% CI 0.66–0.95; p<0.001 for noninferiority and p=0.01 for superiority)” (Table 17).
Major findings of the ARISTOTLE study.
| Apixaban(n=9088) | Warfarin(n=9052) | HR (95% CI) | p | |
| Stroke or systemic embolism | 212 patients1.27%/year | 265 patients1.60%/year | 0.79 (0.66–0.95) | 0.01 |
| Death from any cause | 603 patients3.52%/year | 669 patients3.94%/year | 0.89 (0.80–0.998) | <0.047 |
| Major bleeding | 327 patients2.13%/year | 462 patients3.09%/year | 0.69 (0.60–0.80) | <0.001 |
CI: confidence interval; HR: hazard ratio.
Secondary efficacy outcomes included the following: death from any cause was significantly less common in the apixaban group (603 vs. 669 patients, 3.52%/year vs. 3.94% per year; HR 0.89; 95% CI 0.80–0.99; p=0.047); hemorrhagic stroke was significantly less common in the apixaban group (40 vs. 78 patients, HR 0.51; 95% CI 0.35–0.75, p<0.001), as were all cases of stroke; the incidence of myocardial infarction was not significantly different in the two groups (90 vs. 102 cases, apixaban/warfarin; HR 0.88; 95% CI 0.66–1.17, p=0.37).
Major bleeding occurred in 327 patients under apixaban therapy, compared to 462 under warfarin (HR 0.69; 95% CI 0.60–0.80; p<0.001). Intracranial hemorrhage was also significantly less frequent in the apixaban group (0.33% per year vs. 0.80% per year, HR 0.42; 95% CI 0.30–0.58; p<0.001).
Studies involving aspirin or other antiplatelet drugs without anticoagulant drugsAtrial Fibrillation at Low Risk of Stroke during Treatment with Aspirin – SPAF III (1998)In this prospective cohort multicenter study,38 892 patients with AF received a daily dose of aspirin (325mg). The selected patients had atrial fibrillation and low risk of stroke, based on the absence of four thromboembolic risk factors: CHF or left ventricular fractional shortening ≤25%, prior thromboembolism, systolic blood pressure above 160mmHg, or female gender older than 75 years. The study excluded patients with lone AF, valve replacement, mitral stenosis, contraindications for aspirin or indication for anticoagulants. The primary endpoint was ischemic stroke and systemic embolism.
The mean follow-up was 2 years. The annual primary event rate was 2.2% (95% CI 1.6–3.0%). The annual rate of ischemic stroke was 2.0% (95% CI 1.5–2.8%). The primary event rate was higher in patients with hypertension than in those without (3.6% vs. 1.1%, p<0.001). The rate of disabling ischemic stroke was low in both patients with or without hypertension (1.4% vs. 0.5%). Major bleeding occurred at a rate of 0.7% per year. A history of hypertension (RR 3.3, p=0.001) and age (RR 1.7 increase per 10 years, p=0.01) were independent risk factors for stroke.
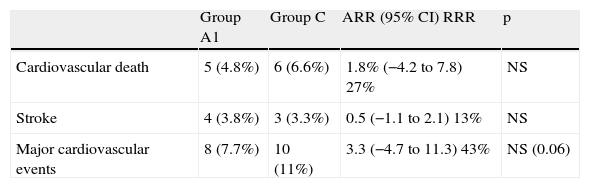
LASAF (1999)In the Low-dose Aspirin, Stroke, and Atrial Fibrillation (LASAF) study, an open, multicenter, randomized study,39 285 patients with AF were divided into three groups. Group A1 was treated with 125mg of aspirin daily (n=104). Group A2 was treated with 125mg of aspirin on alternate days (n=90). Group C (control) was not treated with either OAC or antiplatelet agents (n=91). Exclusion criteria were contraindication to aspirin use or indication for OAC or antiplatelet therapy prior to the beginning of the study. The primary events were cardiovascular death and death from any cause, thrombotic, embolic or hemorrhagic stroke, other embolic events, myocardial infarction, need for coronary surgery and hospital admission for an episode of unstable angina. Stroke, myocardial infarction, death from cardiovascular causes and need for coronary surgery were considered major cardiovascular events.
The follow-up was 1–62 months. The mortality rate from cardiovascular causes was 4.8% in group A1 and 6.6% in group C (relative risk reduction [RRR] 27%). The rate of major cardiovascular events was 7.7% in group A1 and 11% in group C (RRR 43%). The rate of stroke was 3.8% in group A1 and 3.3% in group C (RRR 13%). None of these differences was statistically significant. In group A2, there was a 65% reduction in the risk of stroke compared to group C (1.1% vs. 3.3%, p=0.05). Furthermore, the mortality rate from cardiovascular causes (1.1% vs. 6.6%, p=0.02) and incidence of major cardiovascular events (2.2% vs. 11%, p=0.001) were 80% lower in group A2 compared to group C. The reduction in major cardiovascular events between groups A1 and A2 was statistically significant (7.7% vs. 2.2%, absolute risk reduction [ARR] 5.5%, p<0.05). The differences regarding other endpoints were not statistically significant. Some of the main results are shown in Table 18.
Major findings of the LASAF study.
| Group A1 | Group C | ARR (95% CI) RRR | p | |
| Cardiovascular death | 5 (4.8%) | 6 (6.6%) | 1.8% (−4.2 to 7.8) 27% | NS |
| Stroke | 4 (3.8%) | 3 (3.3%) | 0.5 (−1.1 to 2.1) 13% | NS |
| Major cardiovascular events | 8 (7.7%) | 10 (11%) | 3.3 (−4.7 to 11.3) 43% | NS (0.06) |
| Group A2 | Group C | ARR (95% CI) RRR | p | |
| Cardiovascular death | 1 (1.1%) | 6 (6.6%) | 5.5% (0.5–10.5) (80%) | 0.02 |
| Stroke | 1 (1.1%) | 3 (3.3%) | 2.2 (−1.8 to 6.2) (65%) | 0.05 |
| Major cardiovascular events | 2 (2.2%) | 10 (11%) | 8.8 (1.8–15.8) (80%) | 0.001 |
ARR: absolute risk reduction; CI: confidence interval; RRR: relative risk reduction.
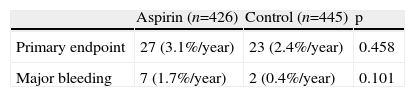
In this open, multicenter study (Japan Atrial Fibrillation Stroke Trial),40 871 Japanese patients with chronic or paroxysmal nonvalvular AF documented by ECG were randomized to receive aspirin (150–200mg, n=426) or no antithrombotic treatment (n=445). Exclusion criteria were prosthetic heart valve, rheumatic heart disease, mitral valve disease, uncontrolled hypertension; reversible causes of AF, severe HF, prior thromboembolism, previous gastrointestinal or intracranial bleeding (in the previous 6 months), and indication for anticoagulation or antiplatelet agents. The primary endpoint was TIA, stroke and death from cardiovascular causes.
The mean follow-up was 768±403 days. The study was terminated early due to the occurrence of 27 primary events in the aspirin group (3.1%/year) compared to 23 events in the control group (2.4%/year), p=0.458, suggesting a low probability of aspirin being superior to no treatment in the prevention of primary events. There were seven major bleeding events in the aspirin group (1.6%) and two events in the control group (0.4%, p=0.101). Some of the main results are shown in Table 19.
Major results of the Japan Atrial Fibrillation Stroke Trial (JAST).
| Aspirin (n=426) | Control (n=445) | p | |
| Primary endpoint | 27 (3.1%/year) | 23 (2.4%/year) | 0.458 |
| Major bleeding | 7 (1.7%/year) | 2 (0.4%/year) | 0.101 |
A post-hoc subgroup analysis of the double-blind randomized study CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance) was published but will not be discussed here since treatment of AF was not the primary aim of the study.41
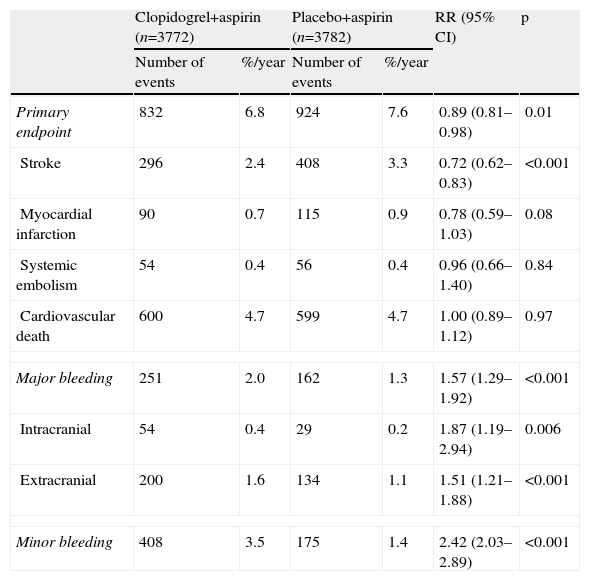
ACTIVE-A (2009)In this study,42 7554 patients with AF and high risk of stroke for whom therapy with vitamin K antagonists was not indicated were randomized to receive, blindly, clopidogrel (3772 patients, 75mg/day) or placebo (3782 patients), in addition to aspirin (75–100mg/day). The inclusion and exclusion criteria were the same as in the ACTIVE-W study, but in this trial patients were excluded if they required a vitamin K antagonist or clopidogrel or had bleeding risk factors. The primary endpoint was any major vascular event (stroke, MI, systemic embolism or death from vascular causes).
After a mean follow-up of 3.6 years, 832 events had occurred in patients receiving clopidogrel (6.8% per year) and 924 events in patients receiving placebo (7.6% per year) (RR 0.89, p=0.01). Stroke occurred in 296 patients receiving clopidogrel+aspirin (2.4% per year) and in 408 patients receiving placebo+aspirin (3.3%/year) (RR 0.72, p<0.001). MI occurred in 90 patients who received clopidogrel+aspirin (0.7%/year) and in 115 patients receiving placebo+aspirin (0.9%/year) (RR 0.78, p=0.08). The annual rates of systemic embolism and mortality from cardiovascular causes were similar between the two groups. Major bleeding occurred in 251 patients receiving clopidogrel+aspirin (2.0%/year) and in 162 patients receiving placebo+aspirin (1.3%/year) (RR 1.57, p<0.001). Some of the main results are shown in Table 20.
Major results of the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE-A) study.
| Clopidogrel+aspirin (n=3772) | Placebo+aspirin (n=3782) | RR (95% CI) | p | |||
| Number of events | %/year | Number of events | %/year | |||
| Primary endpoint | 832 | 6.8 | 924 | 7.6 | 0.89 (0.81–0.98) | 0.01 |
| Stroke | 296 | 2.4 | 408 | 3.3 | 0.72 (0.62–0.83) | <0.001 |
| Myocardial infarction | 90 | 0.7 | 115 | 0.9 | 0.78 (0.59–1.03) | 0.08 |
| Systemic embolism | 54 | 0.4 | 56 | 0.4 | 0.96 (0.66–1.40) | 0.84 |
| Cardiovascular death | 600 | 4.7 | 599 | 4.7 | 1.00 (0.89–1.12) | 0.97 |
| Major bleeding | 251 | 2.0 | 162 | 1.3 | 1.57 (1.29–1.92) | <0.001 |
| Intracranial | 54 | 0.4 | 29 | 0.2 | 1.87 (1.19–2.94) | 0.006 |
| Extracranial | 200 | 1.6 | 134 | 1.1 | 1.51 (1.21–1.88) | <0.001 |
| Minor bleeding | 408 | 3.5 | 175 | 1.4 | 2.42 (2.03–2.89) | <0.001 |
CI: confidence interval; RR: relative risk.
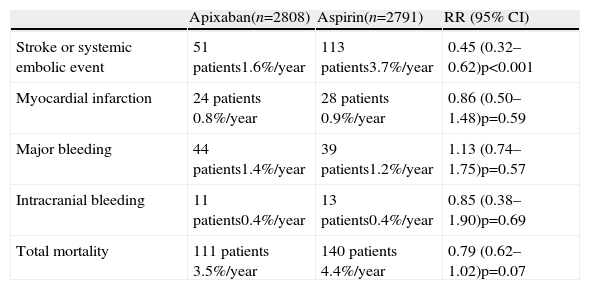
In the Apixaban vs. ASA to reduce the risk of stroke (AVERROES) trial,43 patients with AF and at least one risk factor for stroke, unsuitable for OAC, were randomized to take either aspirin (81–324mg/day) or apixaban, an oral activated factor X inhibitor (5 or 2.5mg twice daily). A total of 5600 patients were enrolled. The study was terminated due to evidence favoring apixaban. Major results of the study included (Table 21): (1) The annual rate of stroke or systemic embolism (the primary outcome) was 3.7% per year on aspirin and 1.6% per year on apixaban (HR 0.45, 95% CI 0.32–0.62, p<0.001); (2) The rate of major bleeding was 1.2%/year on aspirin and 1.4%/year on apixaban (HR 1.13, 95% CI 0.74–1.75, p=0.57); (3) Major intracranial bleeding events occurred in 11 patients treated with apixaban, compared to 13 patients under aspirin therapy; (4) There was no evidence of hepatic toxicity or other major adverse events (Table 21).
Major results of the Apixaban vs. ASA to reduce the risk of stroke (AVERROES) study.
| Apixaban(n=2808) | Aspirin(n=2791) | RR (95% CI) | |
| Stroke or systemic embolic event | 51 patients1.6%/year | 113 patients3.7%/year | 0.45 (0.32–0.62)p<0.001 |
| Myocardial infarction | 24 patients 0.8%/year | 28 patients 0.9%/year | 0.86 (0.50–1.48)p=0.59 |
| Major bleeding | 44 patients1.4%/year | 39 patients1.2%/year | 1.13 (0.74–1.75)p=0.57 |
| Intracranial bleeding | 11 patients0.4%/year | 13 patients0.4%/year | 0.85 (0.38–1.90)p=0.69 |
| Total mortality | 111 patients 3.5%/year | 140 patients 4.4%/year | 0.79 (0.62–1.02)p=0.07 |
CI: confidence interval; RR: relative risk.
In a meta-analysis by Hart et al.,44 data from a total of 29 trials, including 28044 patients, were analyzed. Warfarin therapy (adjusted-dose) reduced the incidence of stroke by 64% (95% CI 49% to 74%), compared to placebo or no treatment. Antiplatelet therapy led to a reduction of 22% (95% CI 6% to 35%), also compared to placebo or no treatment. Compared to antiplatelet therapy, warfarin therapy was associated with a 37% reduction in strokes (95% CI 23% to 48%). Intracranial hemorrhage with warfarin therapy was double the rate with aspirin (risk increase of 0.2% per year). Total mortality was lower with warfarin compared to control or placebo. The authors conclude that their evidence “supports antithrombotic therapy for most patients who have atrial fibrillation”. The aspirin data included results from three trials that combined aspirin with “very low, fixed doses of warfarin”.
Van Walraven et al. performed a meta-analysis including clinical trials comparing oral anticoagulants to aspirin.45 Six clinical trials, including 4052 patients, were selected. The authors showed that the use of oral anticoagulants was associated with less total stroke (“2.4 vs. 4.5 events per 100 patient-years; hazard ratio, 0.55; 95% confidence interval, 0.43–0.71”), less ischemic stroke and less cardiovascular events, but more frequent major bleeding (“2.2 vs. 1.3 events per 100 patient-years; hazard ratio, 1.71; 95% confidence interval, 1.21–2.41”).
Similar data were published by Lip and Edwards,46 Aguilar and Hart,47,48 and Taylor et al.,49 although, in the latter study, several comparisons between anticoagulation and antiplatelet therapy showed non-significant results.
Effectiveness studiesSeveral studies have addressed the issue of the effectiveness of anticoagulation therapy in clinical practice. Data from the studies by Gottlieb et al., Kalra et al. and Caro et al. have been analyzed by Evans and Kalra.50–53 These authors found that patients in clinical practice were older and had higher levels of comorbidity than patients in clinical trials, but stroke rate and major bleeding rate were not different.53 Go et al. found that warfarin therapy was associated with a 51% lower risk of thromboembolism compared to no warfarin therapy, in a group of 11526 patients in clinical practice. The mortality risk was also reduced by warfarin therapy.54 According to the authors, “warfarin was effective in reducing thromboembolic risk in the presence or absence of risk factors for stroke”.54 The effectiveness of anticoagulation has been shown to depend on its intensity.55,56
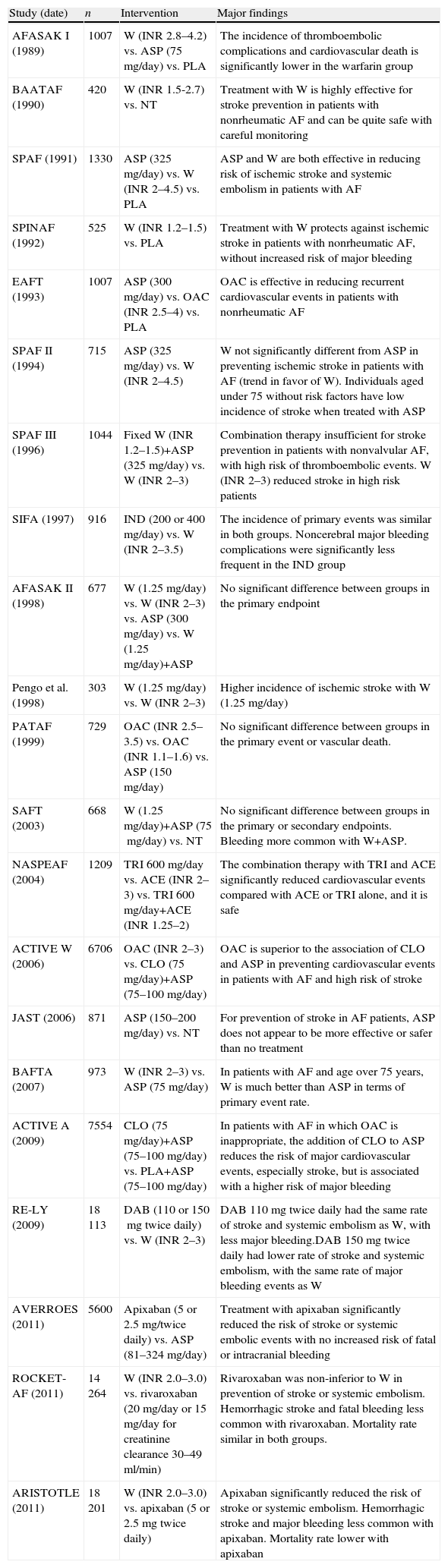
DiscussionAF is associated with an increased risk of ischemic stroke, and one major goal of using antithrombotic therapy is to reduce the incidence of stroke.1,12,24,44,45,57–60 Patients with paroxysmal AF should be regarded as having a stroke risk similar to those with persistent or permanent AF.1 In 1989, Peterson et al. published data supporting the use of oral anticoagulation therapy in patients with chronic AF,10 although the authors underlined concerns about bleeding complications. They showed that warfarin has a significant protective effect in the prevention of thromboembolic complications, but, as in other studies, they found a greater number of bleeding complications20 and abandonment of therapy12,16 compared to the use of aspirin or placebo. Several later studies have pointed in the same direction (Table 22).
Some major studies on thromboembolic prophylaxis in patients with AF and summaries of their conclusions.
| Study (date) | n | Intervention | Major findings |
| AFASAK I (1989) | 1007 | W (INR 2.8–4.2) vs. ASP (75mg/day) vs. PLA | The incidence of thromboembolic complications and cardiovascular death is significantly lower in the warfarin group |
| BAATAF (1990) | 420 | W (INR 1.5-2.7) vs. NT | Treatment with W is highly effective for stroke prevention in patients with nonrheumatic AF and can be quite safe with careful monitoring |
| SPAF (1991) | 1330 | ASP (325mg/day) vs. W (INR 2–4.5) vs. PLA | ASP and W are both effective in reducing risk of ischemic stroke and systemic embolism in patients with AF |
| SPINAF (1992) | 525 | W (INR 1.2–1.5) vs. PLA | Treatment with W protects against ischemic stroke in patients with nonrheumatic AF, without increased risk of major bleeding |
| EAFT (1993) | 1007 | ASP (300mg/day) vs. OAC (INR 2.5–4) vs. PLA | OAC is effective in reducing recurrent cardiovascular events in patients with nonrheumatic AF |
| SPAF II (1994) | 715 | ASP (325mg/day) vs. W (INR 2–4.5) | W not significantly different from ASP in preventing ischemic stroke in patients with AF (trend in favor of W). Individuals aged under 75 without risk factors have low incidence of stroke when treated with ASP |
| SPAF III (1996) | 1044 | Fixed W (INR 1.2–1.5)+ASP (325mg/day) vs. W (INR 2–3) | Combination therapy insufficient for stroke prevention in patients with nonvalvular AF, with high risk of thromboembolic events. W (INR 2–3) reduced stroke in high risk patients |
| SIFA (1997) | 916 | IND (200 or 400mg/day) vs. W (INR 2–3.5) | The incidence of primary events was similar in both groups. Noncerebral major bleeding complications were significantly less frequent in the IND group |
| AFASAK II (1998) | 677 | W (1.25mg/day) vs. W (INR 2–3) vs. ASP (300mg/day) vs. W (1.25mg/day)+ASP | No significant difference between groups in the primary endpoint |
| Pengo et al. (1998) | 303 | W (1.25mg/day) vs. W (INR 2–3) | Higher incidence of ischemic stroke with W (1.25mg/day) |
| PATAF (1999) | 729 | OAC (INR 2.5–3.5) vs. OAC (INR 1.1–1.6) vs. ASP (150mg/day) | No significant difference between groups in the primary event or vascular death. |
| SAFT (2003) | 668 | W (1.25mg/day)+ASP (75mg/day) vs. NT | No significant difference between groups in the primary or secondary endpoints. Bleeding more common with W+ASP. |
| NASPEAF (2004) | 1209 | TRI 600mg/day vs. ACE (INR 2–3) vs. TRI 600mg/day+ACE (INR 1.25–2) | The combination therapy with TRI and ACE significantly reduced cardiovascular events compared with ACE or TRI alone, and it is safe |
| ACTIVE W (2006) | 6706 | OAC (INR 2–3) vs. CLO (75mg/day)+ASP (75–100mg/day) | OAC is superior to the association of CLO and ASP in preventing cardiovascular events in patients with AF and high risk of stroke |
| JAST (2006) | 871 | ASP (150–200mg/day) vs. NT | For prevention of stroke in AF patients, ASP does not appear to be more effective or safer than no treatment |
| BAFTA (2007) | 973 | W (INR 2–3) vs. ASP (75mg/day) | In patients with AF and age over 75 years, W is much better than ASP in terms of primary event rate. |
| ACTIVE A (2009) | 7554 | CLO (75mg/day)+ASP (75–100mg/day) vs. PLA+ASP (75–100mg/day) | In patients with AF in which OAC is inappropriate, the addition of CLO to ASP reduces the risk of major cardiovascular events, especially stroke, but is associated with a higher risk of major bleeding |
| RE-LY (2009) | 18113 | DAB (110 or 150mg twice daily) vs. W (INR 2–3) | DAB 110mg twice daily had the same rate of stroke and systemic embolism as W, with less major bleeding.DAB 150mg twice daily had lower rate of stroke and systemic embolism, with the same rate of major bleeding events as W |
| AVERROES (2011) | 5600 | Apixaban (5 or 2.5mg/twice daily) vs. ASP (81–324mg/day) | Treatment with apixaban significantly reduced the risk of stroke or systemic embolic events with no increased risk of fatal or intracranial bleeding |
| ROCKET-AF (2011) | 14264 | W (INR 2.0–3.0) vs. rivaroxaban (20mg/day or 15mg/day for creatinine clearance 30–49ml/min) | Rivaroxaban was non-inferior to W in prevention of stroke or systemic embolism. Hemorrhagic stroke and fatal bleeding less common with rivaroxaban. Mortality rate similar in both groups. |
| ARISTOTLE (2011) | 18201 | W (INR 2.0–3.0) vs. apixaban (5 or 2.5mg twice daily) | Apixaban significantly reduced the risk of stroke or systemic embolism. Hemorrhagic stroke and major bleeding less common with apixaban. Mortality rate lower with apixaban |
ACE: acenocoumarol; AF: atrial fibrillation; ASP: aspirin; CLO: clopidogrel; DAB: dabigatran; DIP: dipyridamole; IND: indobufen; n: study population; NT: no treatment; OAC: oral anticoagulant drug (vitamin K antagonist); PLA: placebo; TRI: triflusal; W: warfarin.
Currently, various drugs are available to provide antithrombotic protection for patients with AF. In several studies, warfarin has been shown to be significantly superior to aspirin or placebo in the primary and secondary prevention of thromboembolic events, reduction of risk of cardiovascular death and overall mortality.10–12,15,16,30
The greatest concern regarding the use of warfarin is the risk of bleeding, particularly in the elderly. Most studies have shown an increase in major and minor bleeding in patients treated with warfarin compared to aspirin or placebo.10,19,22 In general, “an assessment of bleeding risk should be part of the patient assessment before starting anticoagulation”.1 The HAS-BLED bleeding risk score is recommended in the 2010 ESC guidelines.1
Although the SPINAF study (published in 1992) appeared to show that warfarin in doses adjusted to provide an INR of 1.2–1.5 is effective in preventing stroke,14 these data were not confirmed by subsequent studies, which indicate a need for higher intensity of warfarin therapy.17,19,21 In the JNAFESP study, “low-dose” warfarin (INR 1.5–2.1) was associated with less bleeding than “conventional-dose” warfarin (INR 2.2–3.5),23 suggesting that “low-dose” warfarin therapy is safer. However, the study population was small and follow-up was short, and the protocol was applied to a Japanese population. Pharmacogenetic, environmental and dietary factors could explain these findings. Hu et al. showed that warfarin is effective in preventing stroke in an Asian population with AF.29
It is known that some genetic variants are responsible for differences in individual response to warfarin therapy, including variants of the CYP2C9 and VKORC1 genes. In a comparative effectiveness study, the 6-month incidence of hospitalization was lower in patients receiving warfarin genotyping, compared to a matched historical control group.61
Hylek et al., in their cohort of 13559 patients, showed that an INR of less than 2 was associated with an increased likelihood of death and severe disability from AF-related stroke.55 They also observed an additional risk of intracranial hemorrhage with the use of warfarin when INR values exceeded 3.93.
Aspirin offers only modest protection against stroke for patients with AF, although it appears to be of some interest in patients with contraindication to anticoagulant treatment.1 Antiplatelet therapy reduced stroke by 22% compared to placebo or no treatment, according to the meta-analysis by Hart et al.44 Antiplatelet therapy, however, is clearly inferior to anticoagulant therapy, according to the same44 and other studies. Aspirin could act by decreasing noncardioembolic strokes.44
Antiplatelet agents other than aspirin, such as indobufen and triflusal, may be of interest, but more data are required.1,18,25 Combined antiplatelet therapy with aspirin and clopidogrel may be superior to aspirin alone. The ACTIVE-A study favored an association of the two drugs,42 although a post-hoc subgroup analysis of the CHARISMA trial41 failed to find any benefit with this combination. Combined treatment was shown to be significantly inferior to treatment with oral anticoagulation, with an INR of 2–3, in the ACTIVE-W trial,28 so it should not be considered as first-line therapy.
The theoretical advantage of a combination of lower intensity anticoagulation with antiplatelet agents was the possibility of preserving the antithrombotic effect with a reduced bleeding risk. However, this therapy showed reduced benefit in the prevention of stroke, major cardiovascular events and bleeding complications, compared to either conventional anticoagulation with an INR of 2–3 or with no treatment.17,24
The numerous interactions between vitamin K antagonists and other drugs or foods and variability in individual response mean frequent monitoring of treatment is necessary. The multiple disadvantages of warfarin have stimulated research into developing new anticoagulant drugs that would be safer and easier to administer, using either thrombin inhibition or activated coagulation factor X inhibition as the mechanism of action.
Ximelagatran is an oral direct thrombin inhibitor. Although this drug had shown promising results, with a similar antithrombotic efficacy to warfarin, it has fallen into disuse because of its potential hepatotoxicity.26,27 In the Amadeus study,32 idraparinux was compared to vitamin K antagonists. There was an excess of clinically relevant bleeding in the idraparinux group, leading to the study being terminated early.
Dabigatran appears not to have greater hepatotoxicity than conventional doses of warfarin.33 It is also an oral direct thrombin inhibitor, widely tested in the RE-LY study.33 In this study, two different doses of dabigatran and a conventional dose of warfarin (INR 2–3) were used. Both doses of dabigatran were not inferior to warfarin in preventing systemic embolism or stroke. With 150mg twice daily, the prevention of thromboembolism was greater than that conferred by warfarin, while with 110mg twice daily, fewer major bleeding accidents occurred.33,34 In the 2009 report, fewer strokes were observed in patients under dabigatran therapy compared to warfarin, but more patients under dabigatran had myocardial infarction or pulmonary embolism.33 However, the 2010 update showed that the incidence of myocardial infarction was no longer significantly different when dabigatran was compared to warfarin.34 Dabigatran was approved by the US Food and Drug Administration for the prevention of stroke and systemic embolism in patients with AF (in 2010). Only the 150mg strength was approved, based on what was considered to be the “inability to identify any subgroup in which use of the lower dose would not represent a substantial disadvantage”.62
In the AVERROES trial, apixaban, an oral activated factor X inhibitor, was compared to aspirin. This study was terminated early after confirmation of significant benefits with apixaban.43
In the ROCKET-AF trial, the oral direct factor Xa inhibitor rivaroxaban was shown to be non-inferior to warfarin in the prevention of stroke and systemic embolism in patients with AF and a history of stroke, TIA, systemic embolism or at least two risk factors for stroke.36
In the ARISTOTLE trial, apixaban was compared to warfarin, with favorable results for stroke and systemic embolism, major bleeding, intracranial bleeding and overall mortality.37
In light of the results from the RE-LY, ROCKET-AF and ARISTOTLE studies, it has been stated that “apixaban, dabigatran and rivaroxaban, as compared to warfarin, all significantly reduce the risk of hemorrhagic stroke”; “the risk of particularly serious bleeding was reduced with each of the three drugs”; although apixaban was shown to reduce the risk of death from any cause, “there is approximately a 10% reduction in the risk of death from any cause across these three trials in which the newer anticoagulants were compared with warfarin”.63 Other points of interest in the same comparison included the fact that dabigatran 150mg decreased the risk of ischemic stroke and that rivaroxaban was used once daily.
In patients with nonvalvular AF, a history of stroke or transient ischemic attack is the strongest independent prognostic factor for stroke and is significantly associated with a new stroke.15 Also, prior myocardial infarction,19 hypertension,17 increasing age1,16,17,19,22,23 and diabetes40 have been identified as independent risk factors for ischemic stroke or systemic embolism in patients with AF. Other factors, such as female gender, chronic kidney disease, systolic blood pressure above 160mmHg and ventricular dysfunction, have also been associated with stroke.1,44,58 Hypertension10 and increasing age are associated with an increased risk of stroke but also appear to be associated with increased bleeding risk with anticoagulant therapy.16,19,20,40 Due to this fact, many clinicians are reluctant to prescribe anticoagulants in elderly patients, even nowadays; however, there are data indicating that advanced age should not by itself be regarded as a contraindication for anticoagulation therapy.19,20 In fact, the absolute benefit of oral anticoagulation for stroke prevention increases as AF patients get older.1
In turn, in younger individuals without comorbidities, it has been argued that anticoagulant therapy may be insufficiently beneficial to justify its risk, expense and inconvenience.14,16 Patients aged<60 years with lone AF carry a low cumulative stroke risk.1
Current thinking is that in patients with AF, an estimate of the individual risk of stroke and of bleeding should precede a decision on antithrombotic therapy,1,24,59,60 in such a way that the benefits of therapy can be expected to outweigh its risks. The rate of stroke in patients with nonvalvular AF depends on the presence of prior cerebrovascular ischemic disease, age,16 use of antithrombotic therapy and other comorbid conditions.1,22,24,60 The identification of various clinical risk factors for stroke has led to the publication of several stroke risk Schemes.1,60 The CHADS2 (Cardiac failure, Hypertension, Age, Diabetes, Stroke [Doubled]) index60 is widely used in clinical practice and integrates a number of factors from previously proposed schemes. The expected incidence of stroke per 100 patients annually (95% CI), without antithrombotic therapy, increases by 1.5 per 1 point increase in the CHADS2 score. The CHA2DS2-VASc (CHF, hypertension, age ≥75 [doubled], diabetes, stroke [doubled], vascular disease, age 65–74, and sex category [female]) score1 is a novel index that could improve the “approach to stroke risk stratification in patients with AF”.64 Stroke risk in patients with AF is currently seen as a continuous phenomenon1 and current guidelines recommend either aspirin or no antithrombotic therapy for patients with no risk factors.1
The reasoning behind therapeutic options in “low-risk” (currently labeled as “no risk factors”) AF is mainly derived by combining epidemiological data with data from clinical trials carried out for other purposes, and not directly from data obtained in clinical trials aiming to compare warfarin or another anticoagulant to antiplatelet drugs or to no treatment in low-risk patients. In fact, we are not aware of any clinical trial specifically designed to deal with this particular issue. Data from meta-analyses45,46 and from population studies54 directly indicate a possible beneficial effect of anticoagulant drugs in low-risk AF, and many low-risk AF patients have been included in major AF clinical trials. Dabigatran has been tested in the RE-LY trial in patients at increased risk of stroke and is not, therefore, currently an empirically tested option for AF with no risk factors; the same is true for rivaroxaban in the ROCKET-AF study and for apixaban in the ARISTOTLE and AVERROES studies. Data in favor of the approach of current guidelines has come from the SPAF II trial, in which “the absolute rates of primary events in low-risk younger patients (without hypertension, recent heart failure, or previous thromboembolism) on aspirin was 0.5% per year (95% CI 0.1–1.9)”.16 The best therapeutic option for low-risk AF, therefore, remains undetermined.
Percutaneous closure of the left atrial appendage is a promising technique,65 but lies outside the scope of the present review.
ConclusionsAF is an important and potentially modifiable cause of stroke. It has been known since 1989 that oral anticoagulant drugs, such as warfarin, lead to a dramatic decrease in stroke associated with AF. The best risk-benefit ratio is obtained with intensity of oral anticoagulant treatment for an INR of 2–3, even in the elderly. Given the risks of anticoagulant therapy, including bleeding, individual thromboembolic risk must be assessed in patients with AF. In 2009, dabigatran was shown to be a reasonable alternative to vitamin K antagonists, establishing itself as a major alternative to warfarin in AF patients. Rivaroxaban and apixaban have subsequently also been shown to be alternatives to warfarin. When there are contraindications to vitamin K antagonists, antiplatelet agents can produce a therapeutic effect, although much less than oral anticoagulants. Apixaban may be a better alternative to aspirin in this setting. Patients with low-risk atrial fibrillation (no risk factors) have not been the subjects of specific clinical trials. It is unclear what would be the best therapeutic choice for these patients.
Conflicts of interestThe authors have no conflicts of interest to declare.