In an era in which coronary heart disease is one of the leading causes of death worldwide, several studies report the persistence of obstacles to accessing revascularization, and percutaneous coronary intervention in particular, which may be associated with worse outcomes.
ObjectivesTo compare cardiovascular outcomes in patients admitted to hospitals with and without on-site percutaneous coronary intervention (PCI) capabilities.
Material and MethodsA retrospective study based on the National Registry of Acute Coronary Syndromes (ACS)—with data collection from 2010 to 2018. Division of the patients into two groups: with and without ST-elevation. Two subgroups were subsequently created according to the presence/absence of on-site PCI. A propensity score was performed to standardize the results. Patients without information about hospital admission (with/without PCI) were excluded.
Results6008 patients were included after exclusion criteria and propensity score were applied. We found that patients admitted for ACS with ST-elevation (STE-ACS) had more episodes of sustained ventricular tachycardia (OR 2.14; CI (1.26−3.61); p=0.004) in hospitals without on-site PCI. Regarding ACS without ST elevation (NSTE-ACS), there were more cases of congestive heart failure (OR 0.79; CI (0.65−0.98)) in hospitals with on-site PCI.
ConclusionThe incidence of a greater number of major adverse events in hospitalizations without on-site PCI, particularly in the case of STE-ACS, is a consequence of the delay before revascularization. National and local strategies must be established to reduce the negative impact of the absence of on-site PCI and the resulting time before revascularization.
Numa era em que a doença coronária é uma das principais causas de morte a nível mundial, vários estudos referem a persistência de obstáculos no acesso à revascularização, sobretudo na facilidade de acesso à intervenção coronária percutânea, podendo tal estar associado a piores outcomes.
ObjectivosComparar os outcomes cardiovasculares dos doentes submetidos a intervenção coronária percutânea (ICP) em hospitais com e sem intervenção on-site.
Material e MétodosEstudo retrospectivo baseado no Registo Nacional de Síndromes Coronários Agudos (SCA)—com colheita de dados de 2010 a 2018. Divisão dos SCA em 2 grupos: com e sem supradesnivelamento do segmento ST. Criados ainda 2 subgrupos, de acordo com a presença/ausência de ICP on-site, para cada uma destas entidades. Realizado score de propensão (SdP) para uniformização dos resultados. Excluídos doentes sem informação sobre a realização de ICP.
ResultadosAdmitidos 6008 doentes após aplicação de critérios de exclusão e SdP. Verificamos que os doentes admitidos por SCA com supraST apresentaram mais episódios de Taquicardia Ventricular mantida (OR 2,14; IC (1,26–3,61); p=0,004) em hospitais sem ICP on-site. Relativamente aos SCA sem supraST, verificou-se um predomínio de insuficiência cardíaca congestiva (ICC) (OR 0,79; IC (0,65–0,98); p=0,03) em hospitais com ICP on-site.
ConclusãoA ocorrência de um maior número de eventos adversos major nos hospitais sem ICP on-site, em particular no caso do SCA com supraST, é consequência do atraso até revascularização. Estratégias nacionais e locais devem ser definidas para reduzir o impacto negativo da ausência de ICP on-site e consequente tempo até revascularização.
Despite recent advances in the cardiovascular field, cardiovascular diseases continue to be the main cause of death in Europe, including Portugal.1,2 Due to the need for adequate intervention in patients admitted with acute coronary syndrome (ACS), the current European Society of Cardiology (ESC) guidelines3,4 reinforce the need for early percutaneous coronary intervention (PCI),5,6 with a view to minimizing the complications and mortality associated with this disease.
A recent study7 revealed that the presence of obstacles to accessing revascularization procedures, as well as an increase in mortality, may be related to the geographical area where the patient is initially admitted.8–10 This can be explained partly due to catheterization laboratories (cath labs) being located in large urban centers,9 which may compromise the revascularization of patients initially admitted to more peripheral hospitals without PCI capabilities. Few studies have focused on the real impact of the presence/absence of on-site PCI on our patient outcomes.6,9 “Time is myocardium”, and as such there is an urgent need to assess the real impact of the presence/absence of on-site PCI on our patient outcomes, especially in non-ST-elevation ACS (NSTE-ACS) which has a wider intervention window.
The authors of the study sought to analyze data from the Portuguese Registry of ACS (ProACS) to identify and assess factors that influence the treatment and outcome of patients admitted with ACS, depending on whether or not the admission hospital has on-site PCI capabilities.
MethodologyNational Portuguese Registry of Acute Coronary SyndromesThe National Portuguese Registry of Acute Coronary Syndromes is a continuous and prospective registry, promoted by the Portuguese Society of Cardiology, in which all Cardiology departments in the country are invited to participate actively. The registry began in 2002 and remains active today, with 28 cardiology departments contributing their data daily. Briefly, each site should include all patients admitted to the service with the diagnosis of ACS (with ST-segment elevation (STE) and non-ST-elevation (NSTE)) based on clinical evaluation, as well as the electrocardiographic and analytical changes found.
The registry focuses on collating several variables, in particular: 1) demographic and baseline characteristics of admitted patients; 2) laboratory data on admission and during hospitalization; 3) clinical evolution during hospital stay; 4) pharmacological and invasive strategy performed; 5) cardiovascular events and one-year follow-up, whenever possible. Patient identification remained anonymous at all times, and the registry has been authorized by national authorities and registered on the clinicaltrials.gov platform (NCT 01642329).
All ethical requirements contained in the Declaration of Helsinki 1975 have been met and no human and/or animal experiments have been carried out in this work. Written informed consent for the entry of patient data into the registry has been available since 2010 and has been applied following approval by the ethics committee of each hospital site.
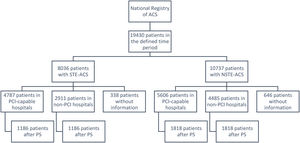
Study designA longitudinal, retrospective, multicenter, non-randomized study based on ProACS between 1st October 2010 and 31st December 2018. All patients with a diagnosis of ACS (STE and NSTE) during the defined time period were included, with patients without information regarding the admission hospital (with vs. without on-site PCI) excluded from the analysis. Subsequently, patients were divided into two groups (STE-ACS and NSTE-ACS), then further subdivided into 2 subgroups, according to their admission to hospitals with or without on-site PCI.
In order to make the two groups as homogeneous as possible, to infer conclusions on the occurrence of cardiovascular complications and mortality, a propensity score (PS) was calculated for each group, using a logistic regression model (Appendix A). A 1:1 pairing was performed, taking into account the following characteristics: age, body mass index, gender, hospital transport via ambulance, cardiovascular risk factors, personal cardiovascular and non-cardiovascular history, medication prior to hospitalization and physical examination on admission (Killip class, blood pressure and heart rate). Two patients were paired whenever their respective scores differed below 0.000001. Appendix A shows in detail which variables are included and their respective PS weighting. Variables common to both groups and the occurrence of death and major cardiovascular events during hospital admission were assessed. Figure 1 summarizes the consecutive stages of the study until the final population was obtained.
Baseline characteristics of the populationThe authors focused on the acquisition of variables related to the population studied. The following variables were collected: 1) population baseline characteristics (age, body mass index, gender, hospital transport, hospital admission site, form of hospital admission, cardiovascular risk factors, cardiovascular history, non-cardiovascular history and previous medication); 2) clinical findings on hospital admission (hemodynamic profile and admission diagnosis); 3) electrocardiographic findings on hospital admission (rhythm, QRS morphology/duration, ST-T segment); 4) angiographic findings (number of coronary vessels with stenosis greater than 50% and culprit vessel, percentage of catheterization performed, PCI).
The variables were compared between the groups created to infer possible differences between them. Times until intervention were also assessed, with the authors focusing on “symptoms to reperfusion”, “first medical contact to reperfusion” and “door to reperfusion” times for the STE-ACS group and “admission to reperfusion” times for the NSTE-ACS group.
Study endpointThe primary endpoint was the occurrence of in-hospital mortality (defined as death from cardiac, vascular or non-cardiac causes) or the occurrence of major cardiovascular events (reinfarction, congestive heart failure (CHF), cardiogenic shock, mechanical complication, atrioventricular block with hemodynamic consequences, sustained ventricular tachycardia (VT) or cardiorespiratory arrest) during hospital admission.
Statistical analysisCategorical variables were described by calculating the respective absolute and relative frequencies, while the continuous variables were described by determining the mean and standard deviation or median and interquartile range, depending on the level of normal distribution in the variables analyzed (assessed using the Kolmogorov-Smirnov test). Whenever comparisons were made between two groups, the chi-square test or Fisher's exact test were used for categorical variables, while the T-test or Mann-Whitney test were favored when comparing two continuous variables.
With regard to inferential statistical analysis, the prognostic impact of the presence of on-site PCI in relation to cardiovascular events and mortality was evaluated according to logistic regression models. These models considered the following variables: On-site PCI, gender, age, diagnosis on admission, cardiovascular risk factors, personal cardiovascular and non-cardiovascular history, Killip class, heart rate, blood pressure, cardiac rhythm, QRS morphology, ST-T segment morphology, coronary angiography (CCTA), coronary lesions and coronary intervention, left ventricular ejection fraction (LVEF) and medication prior to hospital admission.
The stepwise (forward) method, together with the likelihood ratio test, were considered for the selection of variables for inclusion in the present regression models. The adjusted odds ratio, as well as the respective 95% confidence interval (CI 95%), were estimated for each variable included in the regression model. The Hosmer-Lemeshow test was used for the calibration of the regression models. The goodness-of-fit of the logistic regression models was also assessed by determining the area under the curve and its sensitivity and specificity.
Statistical analysis was performed using the Statistical Package for the Social Sciences () 19.0® program, and a significance level of 5% was assumed for the hypothesis tests.
Results- ✓
Study population
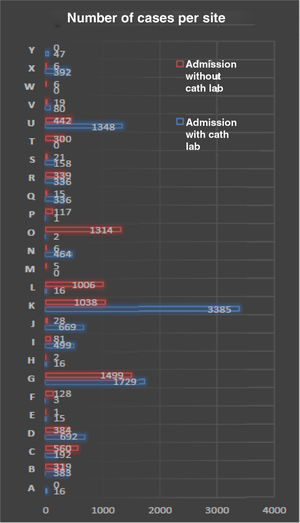
During the inclusion period of the present study (1st October 2010 to 31st December 2018), 28 hospital sites actively participated and their contributions are displayed in Figure 2. Analyzing this in more detail, we find that there are sites with patients admitted simultaneously “with and without on-site PCI”. This is mainly due to three reasons: 1) The existence of hospital sites composed of several hospitals, with only one PCI-capable hospital; 2) transfer of patients from non-PCI hospitals to sites with this capacity, and data entry in the registry was made by the PCI-capable hospital that accepted the patient; 3) the non-PCI hospital gained this capacity during the study time period.
It should also be noted that all PCI-capable hospitals currently operate PCI on a 24 h/day basis, every day of the year, with the exception of one site.
A total of 19 430 patients were registered during the assessment period, and only 17 789 (7698 STE-ACS patients and 10 091 NSTE-ACS) were included in the present analysis after exclusion of those without information on the admission site (PCI/non-PCI-capable). We found a slight predominance of patients admitted to PCI-capable hospitals (STE-ACS: 62.2%; NSTE-ACS: 55.6%).
After application of the PS, the final sample for analysis was 2372 STE patients and 3636 NSTE patients.
- ✓
Baseline characteristics of the population
The mean age of the population was 64 ± 14 years, with a predominance of males (75.4%). Arterial hypertension (61.1%), dyslipidemia (51.6%) and smoking (37%) were the most frequent cardiovascular risk factors in this population. 7.7% had a family history of coronary disease and 10.4% had been hospitalized previously due to ACS. 39.3% of patients traveled to hospital by their own means, the most frequent place of admission being the emergency room (39.7%), followed by the cath lab (30.4%). We also found that pre-hospital transport, by specialized medical staff, was only observed in 27.4% of cases, with the coronary fast track system (FTS) activated in 28.9% of cases. It should also be noted that 3% of coronary FTS cases were transported to non-PCI hospitals. Table 1 displays the baseline characteristics of the population studied. The population comparison, taking into account the presence or absence of PCI capabilities at the admission hospital, shows that in PCI-capable hospitals, a higher proportion of patients arrived via ambulance, and there was a higher prevalence of coronary disease and previous coronary revascularization.
Baseline characteristics of the general population of patients admitted with ST-elevation-acute coronary syndromes.
| General population (n=7698) | Patients in PCI-capable hospitals (n=4787) | Patients in non-PCI hospitals (n=2911) | P-value | |
|---|---|---|---|---|
| Age (years, mean ± standard deviation) | 64 ± 14 | 64 ± 14 | 64 ± 14 | 0.961 |
| BMI (kg/m2, mean ± standard deviation) | 27.1 ± 4.3 | 27.1 ± 4.3 | 27.1 ± 4.2 | 0.920 |
| Male (n, %) | 5806/7698 (75.4%) | 3662/4787 (76.5%) | 2144/2911 (73.7%) | 0.005 |
| Hospital transport (n, %) | ||||
| - Non medical ambulance | 1639/6568 (25%) | 874/4146 (21.1%) | 765/2422 (31.6%) | <0.001 |
| - Emergency response ambulance | 1802/6568 (27.4%) | 1410/4146 (34%) | 392/2422 (16.2%) | <0.001 |
| - Own means | 2579/6568 (39.3%) | 1482/4146 (35.7%) | 1097/2422 (45.3%) | <0.001 |
| Hospital admission site (n, %) | ||||
| - ER | 3050/7651 (39.7%) | 2150/4781 (45%) | 900/2900 (31%) | <0.001 |
| - Cardiac ICU/intermediate care | 2282/7681 (29.7%) | 1080/4781 (22.6%) | 1202/2900 (41.4%) | <0.001 |
| - Cath lab | 2333/7681 (30.4%) | 1540/4781 (32.2%) | 793/2900 (27.3%) | <0.001 |
| - Ward | 7/7681 (0.1%) | 5/4781 (0.1%) | 2/2900 (0.1%) | 0.717 |
| Form of hospital admission (n, %) | ||||
| - Coronary FTS | 2221/7698 (28.9%) | 2133/4787 (44.6%) | 88/2911 (3%) | <0.001 |
| - Emergency | 3431/7698 (44.6%) | 2540/4787 (53.1%) | 891/2911 (30.6%) | <0.001 |
| - Transfer from another hospital | 2031/7698 (26.4%) | 104/4787 (2.2%) | 1927/2911 (66.2%) | <0.001 |
| - Transfer from another service | 15/7698 (0.2%) | 10/4787 (0.2%) | 5/2911 (0.2%) | 0.720 |
| CVRF (n,%) | ||||
| - HTA | 4606/7544 (61.1%) | 2817/4675 (60.3%) | 1789/2869 (62.4%) | 0.069 |
| - Dyslipidemia | 3759/7278 (51.6%) | 2337/4492 (52%) | 1422/2786 (51%) | 0.414 |
| - DM | 1829/7356 (24.3%) | 1089/4677 (23.3%) | 740/2859 (25.9%) | 0.011 |
| - Smoking | 2832/7663 (37%) | 1786/4759 (37.5%) | 1046/2904 (36%) | 0.184 |
| - Family history CHD | 517/6742 (7.7%) | 350/4175 (8.4%) | 167/2567 (6.5%) | 0.005 |
| CV history (n,%) | ||||
| - Previous angina | 1022/7636 (13.4%) | 629/4739 (14.6%) | 330/2897 (11.4%) | <0.001 |
| - Previous AMI | 794/7628 (10.4%) | 528/4732 (11.2%) | 266/2896 (9.2%) | 0.006 |
| - previous CABG | 83/7662 (1.1%) | 49/4762 (1%) | 34/2900 (1.2%) | 0.556 |
| - Previous PCI | 673/7659 (8.8%) | 455/4759 (9.6%) | 218/2900 (7.5%) | 0.002 |
| - PM/ICD | 43/7627 (0.6%) | 24/4729 (0.5%) | 19/2898 (0.7%) | 0.402 |
| - Previous valvulopathy | 91/7596 (1.2%) | 55/4719 (1.2%) | 36/2877 (1.3%) | 0.739 |
| - Previous HF | 165/7652 (2.2%) | 115/4752 (2.4%) | 50/2900 (1.7%) | 0.042 |
| - Peripheral vascular disease | 232/7615 (3%) | 151/4730 (3.2%) | 81/2885 (2.8%) | 0.343 |
| Non-CV history (n,%) | ||||
| - CRD | 251/7584 (3.3%) | 168/4697 (3.6%) | 83/2887 (2.9%) | 0.097 |
| - Neoplasia | 316/7515 (4.2%) | 198/4623 (4.3%) | 118/2892 (4.1%) | 0.670 |
| - COPD | 276/7626 (3.6%) | 174/4737 (3.7%) | 102/2889 (3.5%) | 0.746 |
| - Dementia | 143/6991 (2%) | 105/4466 (2.4%) | 38/2525 (1.5%) | 0.016 |
| - Previous bleeding | 103/7089 (1.5%) | 60/4568 (1.3%) | 43/2521 (1.7%) | 0.187 |
| Previous medication (n,%) | ||||
| - ASA | 1259/7549 (16.7%) | 808/4680 (17.3%) | 451/2869 (15.7%) | 0.080 |
| - Ticagrelor | 54/6167 (0.9%) | 37/3768 (1%) | 17/2399 (0.7%) | 0.261 |
| - Clopidogrel | 422/7543 (5.6%) | 280/4677 (6%) | 142/2866 (5%) | 0.058 |
| - ACEi or ARB II. | 2816/7531 (37.4%) | 1747 (37.4%) | 1069/2857 (37.4%) | 0.972 |
| - Statin | 2043/7548 (27.1%) | 1245/4683 (26.6%) | 798/2865 (27.9%) | 0.229 |
| - Beta-blocker | 1071/7529 (14.2%) | 651/4667 (13.9%) | 420/2862 (14.7%) | 0.381 |
| - Aldosterone antagonist | 94/7600 (1.2%) | 60/4731 (1.3%) | 34/2869 (1.2%) | 0.751 |
| - Digoxin | 64/7602 (0.8%) | 39/4732 (0.8%) | 25/2870 (0.9%) | 0.828 |
| - Amiodarone | 66/7601 (0.9%) | 43/4731 (0.9%) | 23/2870 (0.8%) | 0.624 |
| - Nitrates | 316/7551 (4.2%) | 203/4683 (4.3%) | 113/2868 (3.9%) | 0.406 |
| - Diuretics | 1265/7542 (16.8%) | 799/4675 (17.1%) | 466/2867 (16.3%) | 0.345 |
AHT: arterial hypertension; AMI: acute myocardial infarction; BMI: body mass index; CABG: coronary artery bypass grafting; CHD: coronary heart disease; CV: cardiovascular; CVRF: cardiovascular risk factors; DM: diabetes mellitus; ER: emergency room; ERA: emergency response ambulance; FTS: fast track system; ICD: implantable cardioverter-defibrillator; ICU: intensive care unit; kg: kilogram; n: number of patients who meet the study criteria/number of patients who have information on this criterion; Non-PCI: hospitals without on-site percutaneous coronary intervention capabilities; PCI: percutaneous coronary intervention; PCI-capable: hospitals with on-site percutaneous coronary intervention capabilities; PM: pacemaker.
We found that the mean age was slightly higher (67 ± 13 years), with arterial hypertension (74.9%), dyslipidemia (63.8%) and diabetes (35%) being the main cardiovascular risk factors. 6.8% had a family history of coronary disease and 26.2% had been hospitalized previously due to ACS. 52.2% of patients traveled to hospital by their own means, the most frequent admission site being the emergency room (53.4%), followed by intermediate/intensive care units (44.9%)—see Table 2. Also, at PCI-capable hospitals, a higher proportion of patients traveled via ambulance, and there was a greater proportion of associated comorbidities (family history, dyslipidemia, chronic renal disease (CRD) and chronic obstructive pulmonary disease).
Baseline characteristics of the general population of patients admitted with non-ST-elevation-acute coronary syndromes.
| General population (n=10 091) | Patients in PCI-capable hospitals (n=5606) | Patients in non-PCI hospitals (n=4485) | P-value | |
|---|---|---|---|---|
| Age (years, mean ± standard deviation) | 67 ± 13 | 67 ± 13 | 67 ± 13 | 0.002 |
| BMI (kg/m2, mean ± standard deviation) | 27.6 ± 4.3 | 27.5 ± 4.2 | 27.8 ± 4.5 | 0.004 |
| Male (n, %) | 7278/10 091 (72.1%) | 4038/5606 (72%) | 3240/4485 (72.2%) | 0.814 |
| Hospital transport (n, %) | ||||
| - Non medical ambulance | 2650/8967 (29.6%) | 1234/4840 (25.5%) | 1416/4127 (34.3%) | <0.001 |
| - EMA | 1182/8967 (13.2%) | 738/4840 (15.2%) | 444/4127 (10.8%) | <0.001 |
| - Own means | 4679/8967 (52.2%) | 2667/4840 (55.1%) | 2012/4127 (48.8%) | <0.001 |
| Hospital admission site (n, %) | ||||
| - ER | 5374/10 068 (53.4%) | 3593/5593 (64.2%) | 1781/4475 (39.8%) | <0.001 |
| - Cardiac ICU/intermediate care | 4517/10 068 (44.9%) | 1896/5593 (33.9%) | 2621/4475 (58.6%) | <0.001 |
| - Cath lab | 75/10 068 (0.7%) | 35/5593 (0.9%) | 40/4475 (0.9%) | 0.120 |
| - Ward | 78/10 068 (0.8%) | 57/5593 (1%) | 21/4475 (0.1%) | 0.002 |
| Form of hospital admission (n, %) | ||||
| - Coronary VV | 574/10 091 (5.7%) | 558/5606 (10%) | 16/4485 (0.4%) | <0.001 |
| - Emergency | 6818/10 091 (67.6%) | 4829/5606 (86.1%) | 1989/4485 (44.3%) | <0.001 |
| - Transfer from another hospital | 2650/10 091 (26.3%) | 192/5606 (3.4%) | 2458/4485 (54.8%) | <0.001 |
| - Transfer from another service | 49/10 091 (0.5%) | 27/5606 (0.5%) | 22/4485 (0.5%) | 0.949 |
| CVRF (n,%) | ||||
| - HTA | 7473/9979 (74.9%) | 4182/5540 (75.5%) | 3291/4439 (74.1%) | 0.123 |
| - Dyslipidemia | 6180/9693 (63.8%) | 3550/5353 (66.3%) | 2630/4340 (60.6%) | <0.001 |
| - DM | 3491/9957 (35.1%) | 1921/5516 (34.8%) | 1570/4441 (35.4%) | 0.584 |
| - Smoking | 2315/10 043 (23.1%) | 1227/5571 (22%) | 1088/4472 (24.3%) | 0.006 |
| - Family history CHD | 601/8825 (6.8%) | 365/4818 (7.6%) | 236/4007 (5.9%) | 0.002 |
| CV history (n,%) | ||||
| - Previous angina | 3124/10 022 (31.2%) | 1991/5553 (35.9%) | 1133/4469 (25.4%) | <0.001 |
| - Previous AMI | 2615/9990 (26.2%) | 1561/5528 (28.2%) | 1054/4462 (23.6%) | <0.001 |
| - Previous CABG | 749/10 048 (7.5%) | 439/5566 (7.9%) | 310/4482 (6.9%) | 0.066 |
| - Previous PCI | 1898/10 011 (19%) | 1163/5547 (21%) | 735/4464 (16.5%) | <0.001 |
| - PM/ICD | 184/9971 (1.8%) | 116/5491 (2.1%) | 68/4480 (1.5%) | 0.028 |
| - Previous valvulopathy | 430/9957 (4.3%) | 288/5498 (5.2%) | 142/4459 (3.2%) | <0.001 |
| - Previous HF | 754/10 029 (7.5%) | 508/5551 (9.2%) | 246/4478 (5.5%) | <0.001 |
| - Peripheral vascular disease | 731/9974 (7.3%) | 448/5518 (8.1%) | 283/4456 (6.4%) | <0.001 |
| Non-CV history (n,%) | ||||
| - CRD | 759/9947 (7.6%) | 498/5486 (9.1%) | 261/4461 (5.9%) | <0.001 |
| - Neoplasia | 507/9777 (5.2%) | 297/5314 (5.6%) | 210/4463 (4.7%) | 0.050 |
| - COPD | 622/9994 (6.2%) | 372/5529 (6.7%) | 250/4465 (5.6%) | 0.020 |
| - Dementia | 156/9594 (1.6%) | 92/5316 (1.7%) | 64/4278 (1.5%) | 0.366 |
| - Previous bleeding | 194/9783 (2%) | 115/5509 (2.1%) | 79/4274 (1.8%) | 0.400 |
| Previous medication (n,%) | ||||
| - ASA | 3665/9966 (36.8%) | 2144/5520 (38.8%) | 1521/4446 (34.2%) | <0.001 |
| - Ticagrelor | 156/8232 (1.9%) | 90/4362 (2.1%) | 66/3870 (1.7%) | 0.235 |
| - Clopidogrel | 1690/9966 (17%) | 1019/5520 (18.5%) | 671/4446 (15.1%) | <0.001 |
| - ACEi or ARB II. | 5435/9955 (54.6%) | 3059/5514 (55.5%) | 2376/4441 (53.5%) | 0.049 |
| - Statin | 4519/9971 (45.3%) | 2576/5524 (46.6%) | 1943/4447 (43.7%) | 0.003 |
| - Beta-blocker | 3010/9939 (30.3%) | 1709/5497 (31.1%) | 1301/4442 (29.3%) | 0.052 |
| - Aldosterone antagonist | 309/10 016 (3.1%) | 188/5573 (3.4%) | 121/4443 (2.7%) | 0.062 |
| - Digoxin | 147/10 008 (1.5%) | 101/5568 (1.8%) | 46/4440 (1%) | 0.001 |
| - Amiodarone | 213/10 009 (2.1%) | 132/5569 (2.4%) | 81/4440 (1.8%) | 0.060 |
| - Nitrates | 1702/9971 (17.1%) | 1017/5528 (18.4%) | 685/4443 (15.4%) | <0.001 |
| - Diuretics | 2883/9961 (28.9%) | 1708/5522 (30.9%) | 1175/4439 (26.5%) | <0.001 |
AHT: arterial hypertension; AMI: acute myocardial infarction; BMI: body mass index; CABG: coronary artery bypass grafting; CHD: coronary heart disease; CV: cardiovascular; CVRF: cardiovascular risk factors; DM: diabetes mellitus; ER: emergency room; ERA: emergency response ambulance; FTS: fast track system; ICD: implantable cardioverter-defibrillator; ICU: intensive care unit; kg: kilogram; n: number of patients who meet the study criteria/number of patients who have information on this criterion; Non-PCI: hospitals without on-site percutaneous coronary intervention capabilities; PCI: percutaneous coronary intervention; PCI-capable: hospitals with on-site percutaneous coronary intervention capabilities; PM: pacemaker.
After applying the PS, we found results similar to those previously described as shown in Tables 3 and 4. Note that pre-hospital transportation by specialized medical staff was lower in STE-ACS after application of the PS.
- ✓
Clinical, electrocardiographic and angiographic findings of the population
Baseline characteristics of the population with ST-elevation-acute coronary syndromes after application of propensity score.
| General population (n=2372) | Patients in PCI-capable hospitals (n=1186) | Patients in non-PCI hospitals (n=1186) | P-value | |
|---|---|---|---|---|
| Age (years, mean ± standard deviation) | 64 ± 14 | 64 ± 14 | 63 ± 14 | 0.134 |
| BMI (kg/m2, mean ± standard deviation) | 27.1 ± 4.3 | 27.1 ± 4.4 | 27 ± 4 | 0.373 |
| Male (n, %) | 1749/2372 (73.7%) | 874/1186 (73.7%) | 875/1186 (73.8%) | 0.963 |
| Hospital transport (n, %) | ||||
| - Non-medical ambulances | 692/2372 (29.2%) | 322/1186 (27.2%) | 370/1186 (31.2%) | 0.030 |
| - EMA | 246/1186 (20.7%) | 238/1186 (20.1%) | 0.684 | |
| - Own means | 1014/2372 (42.7%) | 507/1186 (42.7%) | 507/1186 (42.7%) | 1 |
| Hospital admission site (n, %) | ||||
| - ER | 929/2367 (39.2%) 713/2367 (30.1%) | 510/1186 (43.0%) | 419/1181 (35.5%) 433/1181 (36.7%) | <0.001 |
| - Cardiac ICU/intermediate care | 720/2367 (30.4%) | 280/1186 (23.6%) 393/1186 (33.1%) | 327/1181 (27.7%) 1/1181 (0.1%) | <0.001 |
| - Cath lab | 4/2367 (0.2%) | 3/1186 (0.3%) | 0.004 | |
| - Ward | 0.625 | |||
| Form of hospital admission (n, %) | ||||
| - Coronary VV | 496/2372 (20.9%) | 447/1186 (37.7%) | 49/1186 (4.1%) | <0.001 |
| - Emergency | 1186/2372 (50.0%) | 720/1186 (60.7%) | 466/1186 (39.3%) | <0.001 |
| - Transfer from another hospital | 685/2372 (28.9%) | 18/1186 (1.5%) | 667/1186 (56.2%) | <0.001 |
| - Transfer from another service | 5/2372 (0.2%) | 1/1186 (0.1%) | 4/1186 (0.3%) | 0.218 |
| CVRF (n,%) | ||||
| - HTA | 1397/2372 (58.9%) | 702/1186 (59.2%) | 695/1186 (58.6%) | 0.770 |
| - Dyslipidemia | 1142/2372 (48.1%) | 569/1186 (48.0%) | 573/1186 (48.3%) | 0.869 |
| - DM | 524/2372 (22.1%) | 264/1186 (22.3%) | 260/1186 (21.9%) | 0.843 |
| - Smoking | 861/2372 (36.3%) | 425/1186 (35.8%) | 436/1186 (36.8%) | 0.639 |
| - Family history CHD | 137/2372 (5.8%) | 62/1186 (5.2%) | 75/1186 (6.3%) | 0.253 |
| CV history (n,%) | ||||
| - Previous angina | 274/2372 (11.6%) | 136/1186 (11.5%) | 138/1186 (11.6%) | 0.898 |
| - Previous AMI | 225/2372 (9.5%) | 115/1186 (9.7%) | 110/1186 (9.3%) | 0.726 |
| - Previous CABG | 22/2372 (0.9%) | 11/1186 (0.9%) | 11/1186 (0.9%) | 1 |
| - Previous PCI | 181/2372 (7.6%) | 93/1186 (7.8%) | 88/1186 (7.4%) | 0.699 |
| - PM/ICD | 12/2372 (0.5%) | 6/1186 (0.5%) | 6/1186 (0.5%) | 1 |
| - Previous valvulopathy | 27/2372 (1.1%) | 17/1186 (1.4%) | 10/1186 (0.8%) | 0.175 |
| - Previous HF | 45/2372 (1.9%) | 21/1186 (1.8%) | 24/1186 (2.0%) | 0.652 |
| - Peripheral vascular disease | 76/2372 (3.2%) | 37/1186 (3.1%) | 39/1186 (3.3%) | 0.816 |
| Non-CV history (n,%) | ||||
| - CRD | 70/2372 (3.0%) | 32/1186 (2.7%) | 38/1186 (3.2%) | 0.467 |
| - Neoplasia | 118/2372 (5.0%) | 65/1186 (5.5%) | 53/1186 (4.5%) | 0.257 |
| - COPD | 82/2372 (3.5%) | 42/1186 (3.5%) | 40/1186 (3.4%) | 0.822 |
| - Dementia | 43/2372 (1.8%) | 20/1186 (1.7%) | 23/1186 (1.9%) | 0.644 |
| - Previous bleeding | 41/2372 (1.7%) | 21/1186 (1.8%) | 20/1186 (1.7%) | 0.875 |
| Previous medication (n,%) | ||||
| - ASA | 374/2372 (15.8%) | 190/1186 (16%) | 184/1186 (15.5%) | 0.735 |
| - Ticagrelor | 9/1943 (0.5%) | 5/935 (0.5%) | 4/1008 (0.4%) | 0.746 |
| - Clopidogrel | 126/2372 (5.3%) | 63/1186 (5.3%) | 63/1186 (5.3%) | 1 |
| - ACEi or ARB II. | 860/2372 (36.3%) | 431/1186 (36.3%) | 429/1186 (36.2%) | 0.932 |
| - Statin | 634/2372 (26.7%) | 314/1186 (26.5%) | 320/1186 (27.0%) | 0.781 |
| - Beta-blocker | 321/2372 (13.5%) | 160/1186 (13.5%) | 161/1186 (13.6%) | 0.952 |
| - Aldosterone antagonist | 34/2372 (1.4%) | 17/1186 (1.4%) | 17/1186 (1.4%) | 1 |
| - Digoxin | 20/2372 (0.8%) | 8/1186 (0.7%) | 12/1186 (1.0%) | 0.369 |
| - Amiodarone | 21/2372 (0.9%) | 9/1186 (0.8%) | 12/1186 (1.0%) | 0.511 |
| - Nitrates | 103/2372 (4.3%) | 53/1186 (4.5%) | 50/1186 (4.2%) | 0.762 |
| - Diuretics | 399/2372 (16.8%) | 200/1186 (16.9%) | 199/1186 (16.8%) | 0.956 |
AHT: arterial hypertension; AMI: acute myocardial infarction; BMI: body mass index; CABG: coronary artery bypass grafting; CHD: coronary heart disease; CV: cardiovascular; CVRF: cardiovascular risk factors; DM: diabetes mellitus; ER: emergency room; ERA: emergency response ambulance; FTS: fast track system; ICD: implantable cardioverter-defibrillator; ICU: intensive care unit; kg: kilogram; n: number of patients who meet the study criteria/number of patients who have information on this criterion; Non-PCI: hospitals without on-site percutaneous coronary intervention capabilities; PCI: percutaneous coronary intervention; PCI-capable: hospitals with on-site percutaneous coronary intervention capabilities; PM: pacemaker.
Baseline characteristics of the population with non-ST-elevation-acute coronary syndromes after application of PS.
| General population (n=3636) | Patients in PCI-capable hospitals (n=1818) | Patients in non-PCI hospitals (n=1818) | P-value | |
|---|---|---|---|---|
| Age (years, mean ± standard deviation) | 66 ± 13 | 66 ± 13 | 66 ± 13 | 0.972 |
| BMI (kg/m2, mean ± standard deviation) | 27.6 ± 4.6 | 27.3 ± 4.2 | 27.9 ± 4.9 | <0.001 |
| Male (n, %) | 2629/3636 (72.3%) | 1317/1818 (72.4%) | 1312/1818 (72.2%) | 0.853 |
| Hospital transport (n, %) | ||||
| - Non-medical ambulan | 1134/3636 (31.2%) | 508/1818 (27.9%) | 626/1818 (34.4%) | <0.001 |
| - EMA | 477/3636 (13.1%) | 234/1818 (12.9%) | 243/1818 (13.4%) | 0.658 |
| - Own means | 1867/3636 (51.3%) | 1008/1818 (55.4%) | 859/1818 (47.2%) | <0.001 |
| Hospital admission site (n, %) | ||||
| - ER | 1722/3631 (47.4%) | 1038/1816 (57.2%) | 684/1815 (37.7%) | <0.001 |
| - Cardiac ICU/intermediate care | 1838/3631 (50.6%) | 735/1816 (40.5%) | 1103/1815 (60.8%) | <0.001 |
| - Cath lab | 27/3631 (0.7%) | 10/1816 (0.6%) | 17/1815 (0.9%) | 0.176 |
| - Ward | 38/3631 (1.0%) | 29/1816 (1.6%) | 9/1815 (0.5%) | 0.001 |
| Form of hospital admission (n, %) | ||||
| - Coronary VV | 192/3636 (5.3%) | 183/1818 (10.1%) | 9/1818 (0.5%) | <0.001 |
| - Emergency | 2482/3636 (68.3%) | 1566/1818 (86.1%) | 916/1818 (50.4%) | <0.001 |
| - Transfer from another hospital | 944/3636 (26.0%) | 61/1818 (3.4%) | 883/1818 (48.6%) | <0.001 |
| - Transfer from another service | 18/3636 (0.5%) | 8/1818 (0.4%) | 10/1818 (0.6%) | 0.637 |
| CVRF (n,%) | ||||
| - AHT | 2675/3636 (73.6%) | 1341/1818 (73.8%) | 1334/1818 (73.4%) | 0.792 |
| - Dyslipidemia | 2149/3636 (59.1%) | 1076/1818 (59.2%) | 1073/1818 (59.0%) | 0.919 |
| - DM | 1228/3636 (33.8%) | 599/1818 (32.9%) | 629/1818 (34.6%) | 0.293 |
| - Smoking | 861/3636 (23.7%) | 429/1818 (23.6%) | 432/1818 (23.8%) | 0.907 |
| - Family history CHD | 223/3636 (6.1%) | 98/1818 (5.4%) | 125/1818 (6.9%) | 0.062 |
| CV history (n,%) | ||||
| - Previous angina | 1079/3636 (29.7%) | 549/1818 (30.2%) | 530/1818 (29.2%) | 0.490 |
| - Previous AMI | 933/3636 (25.7%) | 480/1818 (26.4%) | 453/1818 (24.9%) | 0.305 |
| - Previous CABG | 263/3636 (7.2%) | 131/1818 (7.2%) | 132/1818 (7.3%) | 0.949 |
| - Previous PCI | 697/3636 (19.2%) | 362/1818 (19.9%) | 335/1818 (18.4%) | 0.255 |
| - PM/ICD | 78/3636 (2.1%) | 44/1818 (2.4%) 55/1818 (3.0%) | 34/1818 (1.9%) | 0.252 |
| - Previous valvulopathy | 122/3636 (3.4%) | 130/1818 (7.2%) | 67/1818 (3.7%) | 0.269 |
| - Previous HF | 252/3636 (6.9%) | 103/1818 (5.7%) | 122/1818 (6.7%) | 0.601 |
| - Peripheral vascular disease | 219/3636 (6.0%) | 116/1818 (6.4%) | 0.365 | |
| Non-CV history (n,%) | ||||
| - CRD | 252/3636 (6.9%) | 124/1818 (6.8%) | 128/1818 (7.0%) | 0.794 |
| - Neoplasia | 174/3636 (4.8%) | 78/1818 (4.3%) | 96/1818 (5.3%) | 0.162 |
| - COPD | 213/3636 (5.9%) | 102/1818 (5.6%) | 111/1818 (6.1%) | 0.525 |
| - Dementia | 51/3636 (1.4%) | 28/1818 (1.5%) | 23/1818 (1.3%) | 0.481 |
| - Previous bleeding | 64/3636 (1.8%) | 30/1818 (1.7%) | 34/1818 (1.9%) | 0.614 |
| Previous medication (n,% | ||||
| - ASA | 1288/3636 (35.4%) | 643/1818 (35.4%) | 645/1818 (35.5%) | 0.945 |
| - Ticagrelor | 55/3039 (1.8%) | 31/1416 (2.2%) | 24/1623 (1.5%) | 0.143 |
| - Clopidogrel | 607/3636 (16.7%) | 310/1818 (17.1%) | 297/1818 (16.3%) | 0.563 |
| - ACEi or ARB II. | 1985/3636 (54.6%) | 1015/1818 (55.8%) | 970/1818 (53.4%) | 0.134 |
| - Statin | 1603/3636 (44.1%) | 808/1818 (44.4%) | 795/1818 (43.7%) | 0.664 |
| - Beta-blocker | 1081/3636 (29.7%) | 557/1818 (30.6%) | 524/1818 (28.8%) | 0.231 |
| - Aldosterone antagonist | 117/3636 (3.2%) | 57/1818 (3.1%) | 60/1818 (3.3%) | 0.778 |
| - Digoxin | 48/3636 (1.3%) | 26/1818 (1.4%) | 22/1818 (1.2%) | 0.561 |
| - Amiodarone | 73/3636 (2.0%) | 34/1818 (1.9%) | 39/1818 (2.1%) | 0.554 |
| - Nitrates | 626/3636 (17.2%) | 317/1818 (17.4%) | 309/1818 (17.0%) | 0.725 |
| - Diuretics | 1044/3636 (28.7%) | 530/1818 (29.2%) | 514/1818 (28.3%) | 0.558 |
AHT: arterial hypertension; AMI: acute myocardial infarction; BMI: body mass index; CABG: coronary artery bypass grafting; CHD: coronary heart disease; CV: cardiovascular; CVRF: cardiovascular risk factors; DM: diabetes mellitus; ER: emergency room; ERA: emergency response ambulance; FTS: fast track system; ICD: implantable cardioverter-defibrillator; ICU: intensive care unit; kg: kilogram; n: number of patients who meet the study criteria/number of patients who have information on this criterion; Non-PCI: hospitals without on-site percutaneous coronary intervention capabilities; PCI: percutaneous coronary intervention; PCI-capable: hospitals with on-site percutaneous coronary intervention capabilities; PM: pacemaker.
Most patients presented with Killip class I (85.3%). Inferior infarctions predominated (50.5%). Most patients presented a significant lesion of only one vessel (53.3%), with the most frequently found culprit lesion at the level of the anterior descending artery (45.9%). Table 5 summarizes in more detail the findings described here. In comparing the subgroups, the study found that in PCI-capable hospitals there is a greater proportion of coronary disease of between one and three vessels, and the common trunk is involved more frequently.
Clinical, electrocardiographic and angiographic findings in patients with ST-elevation-acute coronary syndromes.
| General population (n=7698) | Patients in PCI-capable hospitals (n=4787) | Patients in non-PCI hospitals (n=2911) | P-value | |
|---|---|---|---|---|
| HP On admission | ||||
| - HR (bpm, mean ± SD) | 78 ± 20 | 77 ± 20 | 78 ± 20 | 0.881 |
| - SBP (mmHg, mean ± SD) | 134 ± 30 | 133 ± 30 | 136 ± 30 | <0.001 |
| - DBP (mmHg, mean ± SD) | 79 ± 18 | 79 ± 18 | 80 ± 18 | 0.001 |
| Killip class (n, %) | ||||
| I | 6535/7657 (85.3%) | 4064/4762 (85.3%) | 2471/2895 (85.4%) | 0.989 |
| II + III + IV. | 1122/7657 (14.7%) | 698/4762 (14.7%) | 424/2895 (14.6%) | 0.989 |
| Electrocardiographic findings | ||||
| - Cardiac rhythm (n,%) | ||||
| Sinus | 7127/7687 (92.7%) | 4417/4779 (92.4%) | 2710/2908 (93.2%) | 0.210 |
| AF: | 413/7657 (5.4%) | 256/4779 (5.4%) | 157/2908 (5.4%) | 0.937 |
| - QRS (n, %) | ||||
| Normal | 6812/7651 (89%) | 4200/4748 (88.5%) | 2612/2903 (90%) | <0.001 |
| Pacemaker | 18/7651 (0.2%) | 9/4748 (0.2%) | 9/2903 (0.291%) | 0.420 |
| CLBBB: | 140/7651 (1.8%) | 100/4748 (2.1%) | 40/2903 (1.4%) | 0.021 |
| CRBBB: | 410/7651 (5.4%) | 268/4748 (5.6%) | 142/2903 (4.9%) | 0.156 |
| - Location of the infarction (n,%) | ||||
| Anterior | 3729/7697 (48.4%) | 2332/4786 (48.7%) | 1397/2911 (48%) | 0.531 |
| Inferior | 3888/7697 (50.5%) | 2395/4786 (50%) | 1493/2911 (51.3%) | 0.289 |
| New CLBBB | 80/7697 (1%) | 59/4786 (1.2%) | 21/2911 (0.7%) | 0.032 |
| Vessels with stenosis >50% (n,%) | ||||
| - No vessels | 123/6055 (2%) | 71/3906 (1.8%) | 52/2149 (2.4%) | 0.112 |
| - One vessel | 3227/6055 (53.3%) | 2151/3906 (55.1%) | 1076/2149 (50.1%) | <0.001 |
| - Two vessels | 1694/6055 (28%) | 1095/3906 (28%) | 599/2149 (27.9%) | 0.894 |
| - Three vessels | 1011/6055 (16.7%) | 589/3906 (15.1%) | 422/2149 (19.6%) | <0.001 |
| Culprit vessel (n, %) | ||||
| - Common trunk | 50/6449 (0.8%) | 43/4016 (1.1%) | 7/2433 (0.3%) | <0.001 |
| - Anterior descending | 2927/6449 (45.4%) | 1830/4016 (45.6%) | 1097/2433 (45.1%) | 0.708 |
| - Circumflex | 766/6449 (11.9%) | 452/4016 (11.3%) | 314/2433 (12.9%) | 0.047 |
| - Right coronary | 2375/6449 (36.8%) | 1457/4016 (36.3%) | 918/2433 (37.7%) | 0.242 |
| - Bypass | 23/6449 (0.4%) | 12/4016 (0.3%) | 11/2433 (0.5%) | 0.317 |
| - Not identified | 308/6449 (4.8%) | 222/4016 (5.5%) | 86/2433 (3.5%) | <0.001 |
AF: atrial fibrillation; AMI: acute myocardial infarction; bpm: beats per minute; CLBBB: complete left bundle branch block; CRBBB: complete right bundle branch block; DBP: diastolic blood pressure; H.P.: hemodynamic profile; HR: heart rate; n: number of patients who meet studied criteria / number of patients who have information about this criterion; SD: standard deviation; SBP: systolic blood pressure.
A predominance of Killip class I was observed (85.5%), as in the STE-ACS group. 90.9% of our patients presented sinus rhythm, with ST-segment depression being the most frequent finding (32.7%) in both groups. Most patients presented a significant lesion of only one vessel (35.4%), with the most frequently found culprit lesion at the level of the anterior descending artery (32.7%). Table 6 summarizes in more detail the findings described here. Once again, the proportion of common trunk involvement is greater in PCI-capable hospitals.
Clinical, electrocardiographic and angiographic findings in patients with non-ST-elevation-acute coronary syndromes.
| General population (n=10091) | Patients in PCI-capable hospitals (n=5606) | Patients in non-PCI hospitals (n=4485) | P-value | |
|---|---|---|---|---|
| HP On admission | ||||
| - HR (bpm, mean ± SD) | 77 ± 19 | 77 ± 18 | 78 ± 19 | 0.015 |
| - SBP (mmHg, mean ± SD) | 142 ± 28 | 142 ± 27 | 142 ± 29 | 0.404 |
| - DBP (mmHg, mean ± SD) | 80 ± 16 | 79 ± 16 | 80 ± 16 | 0.448 |
| Killip class (n, %) | ||||
| I | 8587/10041 (85.5%) | 4743/5569 (85.2%) | 3844/4472 (86%) | 0.264 |
| II + III + IV. | 1454/10041 (14.5%) | 826/5569 (14.8%) | 628/4472 (14%) | 0.264 |
| Electrocardiographic findings | ||||
| - Cardiac rhythm (n,%) | ||||
| Sinus | 9149/10070 (90.9%) | 5024/5588 (89.9%) | 4125/4482 (92%) | <0.001 |
| AF: | 801/10070 (8%) | 480/5588 (8.6%) | 321/4482 (7.2%) | 0.008 |
| - QRS (n, %) | ||||
| Normal | 8463/10022 (84.4%) | 4613/5544 (83.2%) | 3850/4478 (86%) | <0.001 |
| Pacemaker | 89/10022 (0.9%) | 53/5544 (1%) | 36/4478 (0.8%) | 0.420 |
| CLBBB: | 200/10022 (2%) | 117/5544 (2.1%) | 83/4478 (1.9%) | 0.361 |
| CRBBB: | 739/10022 (7.4%) | 413/5544 (7.4%) | 326/4478 (7.3%) | 0.747 |
| - ST-T segment (n,%) | ||||
| Transient ST-segment elevation | 526/10021 (5.2%) | 281/5551 (5.1%) | 245/4470 (5.5%) | 0.350 |
| ST depression | 3281/10021 (32.7%) | 1836/5551 (33.1%) | 1445/4470 (32.3%) | 0.427 |
| Negative T wave | 2435/10021 (24.3%) | 1319/5551 (23.8%) | 1116/4470 (25%) | 0.162 |
| Normal | 3187/10021 (31.8%) | 1825/5551 (32.9%) | 1362/4470 (30.5%) | 0.010 |
| Vessels with stenosis >50% (n,%) | ||||
| - No vessels | 823/7721 (10.7%) | 484/4115 (11.8%) | 339/3606 (9.4%) | <0.001 |
| - One vessel | 2734/7721 (35.4%) | 1424/4115 (34.6%) | 1310/3606 (36.3%) | 0.114 |
| - Two vessels | 2068/7721 (26.8%) | 1102/4115 (26.8%) | 966/3606 (26.8%) | 0.993 |
| - Three vessels | 2096/7721 (27.1%) | 1105/4115 (26.9%) | 991/3606 (27.5%) | 0.535 |
| Culprit vessel (n, %) | ||||
| - Common trunk | 172/6762 (2.5%) | 103/3533 (2.9%) | 69/3229 (2.1%) | 0.042 |
| - Anterior descending | 2176/6762 (32.2%) | 1154/3533 (32.7%) | 1022/3229 (31.7%) | 0.373 |
| - Circumflex | 1397/6762 (20.7%) | 709/3533 (20.1%) | 688/3229 (21.3%) | 0.209 |
| - Right coronary | 1318/6762 (19.5%) | 672/3533 (19%) | 646/3229 (20%) | 0.307 |
| - Bypass | 147/6762 (2.2%) | 76/3533 (2.2%) | 71/3229 (2.2%) | 0.893 |
| - Not identified | 1552/6762 (23%) | 819/3533 (23.2%) | 733/3229 (22.7%) | 0.639 |
AF: atrial fibrillation; AMI: acute myocardial infarction; bpm: beats per minute; CLBBB: complete left bundle branch block; CRBBB: complete right bundle branch block; DBP: diastolic blood pressure; H.P.: hemodynamic profile; HR: heart rate; n: number of patients who meet studied criteria / number of patients who have information about this criterion; SD: standard deviation; SBP: systolic blood pressure.
After applying the PS, we found results similar to those described for the general population, as shown in Tables 7 and 8.
- ✓
Times until reperfusion in acute coronary syndrome
Clinical, electrocardiographic and angiographic findings in patients with ST-elevation-acute coronary syndromes after application of propensity score.
| General population (n=2372) | Patients in PCI-capable hospitals (n=1186) | Patients in non-PCI hospitals (n=1186) | P-value | |
|---|---|---|---|---|
| HP On admission | ||||
| - HR (bpm, mean ± SD) | 77 ± 20 | 77 ± 20 | 77 ± 20 | 0.946 |
| - SBP (mmHg, mean ± SD) | 135 ± 30 | 135 ± 31 | 134 ± 29 | 0.396 |
| - DBP (mmHg, mean ± SD) | 79 ± 18 | 80 ± 18 | 79 ± 17 | 0.674 |
| Killip class (n, %) | ||||
| I | 2053/2372 (86.6%) | 1025/1186 (86.4%) | 1028/1186 (86.7%) | 0.857 |
| II + III + IV. | 319/2372 (13.4%) | 161/1186 (13.6%) | 158/1186 (13.3%) | 0.857 |
| Electrocardiographic findings | ||||
| - Cardiac rhythm (n,%) | ||||
| Sinus | 2206/2370 (93.1%) | 1095/1185 (92.4%) | 1111/1185 (93.8%) | 0.195 |
| AF: | 127/2370 (5.4%) | 63/1185 (5.3%) | 64/1185 (5.4%) | 0.927 |
| - QRS (n, %) | ||||
| Normal | 2096/2360 (88.8%) | 1029/1176 (87.5%) | 1067/1184 (90.1%) | 0.044 |
| Pacemaker | 5/2360 (0.2%) | 4/1176 (0.3%) | 1/1184 (0.1%) | 0.217 |
| CLBBB: | 41/2360 (1.7%) | 23/1176 (2.0%) | 18/1184 (1.5%) | 0.418 |
| CRBBB: | 133/2360 (5.6%) | 71/1176 (6.0%) | 62/1184 (5.2%) | 0.399 |
| - Location of the infarction (n,%) | ||||
| Anterior | 1135/2372 (47.8%) | 572/1186 (48.2%) | 563/1186 (47.5%) | 0.711 |
| Inferior | 1212/2372 (51.1%) | 601/1186 (50.7%) | 611/1186 (51.5%) | 0.681 |
| New CLBBB | 25/2372 (1.1%) | 13/1186 (1.1%) | 12/1186 (1.0%) | 0.841 |
| Vessels with stenosis >50% (n,%) | ||||
| - No vessels | 43/1998 (2.2%) | 21/1014 (2.1%) | 22/984 (2.2%) | 0.800 |
| - One vessel | 1114/1998 (55.8%) | 583/1014 (57.5%) | 531/984 (54.0%) | 0.112 |
| - Two vessels | 533/1998 (26.7%) | 263/1014 (25.9%) | 270/984 (27.4%) | 0.448 |
| - Three vessels | 308/1998 (15.4%) | 147/1014 (14.5%) | 161/984 (16.4%) | 0.248 |
| Culprit vessel (n, %) | ||||
| - Common trunk | 13/1980 (0.7%) | 9/1004 (0.9%) | 4/976 (0.4%) | 0.180 |
| - Anterior descending | 884/1980 (44.6%) | 451/1004 (44.9%) | 433/976 (44.4%) | 0.804 |
| - Circumflex | 217/1980 (11.0%) | 102/1004 (10.2%) | 115/976 (11.8%) | 0.248 |
| - Right coronary | 752/1980 (38.0%) | 369/1004 (36.8%) | 383/976 (39.2%) | 0.254 |
| - Bypass | 9/1980 (0.5%) | 5/1004 (0.5%) | 4/976 (0.4%) | 1 |
| - Not identified | 105/1980 (5.3%) | 68/1004 (6.8%) | 37/976 (3.8%) | 0.003 |
AF: atrial fibrillation; AMI: acute myocardial infarction; bpm: beats per minute; CLBBB: complete left bundle branch block; CRBBB: complete right bundle branch block; DBP: diastolic blood pressure; H.P.: hemodynamic profile; HR: heart rate; n: number of patients who meet studied criteria / number of patients who have information about this criterion; SD: standard deviation; SBP: systolic blood pressure.
Clinical, electrocardiographic and angiographic findings in patients with non-ST-elevation-acute coronary syndromes after application of propensity score.
| General population (n=3636) | Patients in PCI-capable hospitals (n=1818) | Patients in non-PCI hospitals (n=1818) | P-value | |
|---|---|---|---|---|
| HP On admission | ||||
| - HR (bpm, mean ± SD) | 77 ± 18 | 77 ± 18 | 77 ± 19 | 0.855 |
| - SBP (mmHg, mean ± SD) | 143 ± 28 | 143 ± 28 | 144 ± 29 | 0.170 |
| - DBP (mmHg, mean ± SD) | 80 ± 16 | 79 ± 16 | 80 ± 17 | 0.182 |
| Killip class (n, %) | ||||
| I | 3163/3636 (87.0%) | 1578/1818 (86.8%) | 1585/1818 (87.2%) | 0.730 |
| II + III + IV. | 473/3636 (13.0%) | 240/1818 (13.2%) | 233/1818 (12.8%) | 0.730 |
| Electrocardiographic findings | ||||
| - Cardiac rhythm (n,%) | ||||
| Sinus | 3322/3633 (91.4%) | 1642/1815 (90.5%) | 1680/1818 (92.4%) | 0.037 |
| AF: | 273/3633 (7.5%) | 151/1815 (8.3%) | 122/1818 (6.7%) | 0.066 |
| - QRS (n, %) | ||||
| Normal | 3119/3622 (86.1%) | 1544/1805 (85.5%) | 1575/1817 (86.7%) | 0.321 |
| Pacemaker | 36/3622 (1.0%) | 14/1805 (0.8%) | 22/1817 (1.2%) | 0.187 |
| CLBBB: | 65/3622 (1.8%) | 30/1805 (1.7%) | 35/1817 (1.9%) | 0.549 |
| CRBBB: | 246/3622 (6.8%) | 126/1805 (7.0%) | 120/1817 (6.6%) | 0.653 |
| - ST-T segment (n,%) | ||||
| Transient ST-segment elevation | 208/3621 (5.7%) | 103/1805 (5.7%) | 105/1816 (5.8%) | 0.922 |
| ST depression | 1177/3621 (32.5%) | 592/1805 (32.8%) | 585/1816 (32.2%) | 0.780 |
| Negative T wave | 880/3621 (24.3%) | 422/1805 (23.4%) | 458/1816 (25.2%) | 0.197 |
| Normal | 1149/3621 (31.7%) | 602/1805 (33.4%) | 547/1816 (30.1%) | 0.037 |
| Vessels with stenosis >50% (n,%) | ||||
| - No vessels | 300/2871 (10.4%) | 158/1394 (11.3%) | 142/1477 (9.6%) | 0.132 |
| - One vessel | 1076/2871 (37.5%) | 529/1394 (37.9%) | 547/1477 (37.0%) | 0.613 |
| - Two vessels | 800/2871 (27.9%) | 378/1394 (27.1%) | 422/1477 (28.6%) | 0.385 |
| - Three vessels | 695/2871 (24.2%) | 329/1394 (23.6%) | 366/1477 (24.8%) | 0.461 |
| Culprit vessel (n, %) | ||||
| - Common trunk | 61/2490 (2.4%) | 35/1213 (2.9%) | 26/1277 (2.0%) | 0.171 |
| - Anterior descending | 824/2490 (33.1%) | 406/1213 (33.5%) | 418/1277 (32.7%) | 0.696 |
| - Circumflex | 524/2490 (21.0%) | 238/1213 (19.6%) | 286/1277 (22.4%) | 0.089 |
| - Right coronary | 468/2490 (18.8%) | 227/1213 (18.7%) | 241/1277 (18.9%) | 0.919 |
| - Bypass | 60/2490 (2.4%) | 29/1213 (2.4%) | 31/1277 (2.4%) | 0.952 |
| - Not identified | 553/2490 (22.2%) | 278/1213 (22.9%) | 275/1277 (21.5%) | 0.406 |
AF: atrial fibrillation; AMI: acute myocardial infarction; bpm: beats per minute; CLBBB: complete left bundle branch block; CRBBB: complete right bundle branch block; DBP: diastolic blood pressure; H.P.: hemodynamic profile; HR: heart rate; n: number of patients who meet studied criteria / number of patients who have information about this criterion; SD: standard deviation; SBP: systolic blood pressure.
ST-elevation acute coronary syndrome The median time from first medical contact to reperfusion was 112 [68;175] min, with non-PCI hospitals result 69 min higher than PCI-capable hospitals (Table 9). In general, non-PCI hospitals presented a longer delay in the times assessed. However, there were still considerable delays in patients admitted to PCI-capable hospitals.
Assessment of times until intervention according to admission hospital.
| STEMI | General population (n=7698) | Patients in PCI-capable hospitals (n=4787) | Patients in non-PCI hospitals (n=2911) | P-value |
|---|---|---|---|---|
| Times (minutes, median, (P25;P75)) | ||||
| - Symptoms ➔ reperfusion | 248 (169;402) | 220 (152;354) | 300 (210;480) | <0.001 |
| - First medical contact ➔reperfusion | 112 (68;175) | 87 (55;135) | 156 (111; 232) | <0.001 |
| - Door ➔reperfusion | 67 (26;142) | 40 (20;80) | 140 (89;213) | <0.001 |
| NSTEMI | General population (n=10091) | Patients in PCI-capable hospitals (n=5606) | Patients in non-PCI hospitals (n=4485) | P-value |
|---|---|---|---|---|
| Times (minutes, median, (P25;P75)) | ||||
| - Hospital admission to catheterization | 0 (0;2) | 0 (0;1) | 1 (0;2) | <0.001 |
AMI: acute myocardial infarction; h: hours; m: minutes; Non-PCI: hospital without percutaneous coronary intervention capabilities; P25: 25th percentile 25; P75: 75th percentile 75; PCI-capable: hospital with percutaneous coronary intervention capabilities.
After applying PS, we observed a slight worsening of the median “first medical contact to reperfusion” time. We also found that the time was 72 min longer in non-PCI hospitals than PCI-capable hospitals (p<0.001). This is shown in Table 10, with a breakdown of the times under study.
Assessment of times until intervention according to admission hospital after application of propensity score.
| STEMI | General population (n=2372) | Patients in PCI-capable hospitals (n=1186) | Patients in non-PCI hospitals (n=1186) | P-value |
|---|---|---|---|---|
| Times (minutes, median, (P25;P75)) | ||||
| - Symptoms ➔ reperfusion | 259 (178;405) | 225 (157; 361) | 293.5 (210;448) | <0.001 |
| - First medical contact ➔reperfusion | 120 (72;190) | 86 (52;140.5) | 158 (110; 226) | <0.001 |
| - Door ➔reperfusion | 78.5 (30;155) | 42 (20;81) | 132 (81.5;203.5) | <0.001 |
| NSTEMI | General population (n=3636) | Patients in PCI-capable hospitals (n=1818) | Patients in non-PCI hospitals (n=1818) | P-value |
|---|---|---|---|---|
| Times (minutes, median, (P25;P75)) | ||||
| - Hospital admission to catheterization | 0 (0;2) | 0 (0;0) | 1 (0;2) | <0.001 |
AMI: acute myocardial infarction; h: hours; m: minutes; Non-PCI: hospital without percutaneous coronary intervention capabilities; P25: 25th percentile 25; P75: 75th percentile 75; PCI-capable: hospital with percutaneous coronary intervention capabilities.
The median time from hospital admission to coronary reperfusion was less than one day, with the non-PCI hospital result higher (one day) than PCI-capable hospitals (Table 9).
After applying PS, we found that the time gap between the two groups is maintained (Table 10).
- ✓
Therapeutic intervention
92.7% of the population underwent CCTA, with 86.9% undergoing angioplasty. A slight predominance of catheterization (93.7% vs. 91%, p<0.001) and angioplasties (88.5% vs. 84.2%, p<0.001) is worthy of note in patients admitted to PCI-capable hospitals. A residual percentage (0.3%) of the population underwent coronary-aortic revascularization surgery. dRegarding medication during hospitalization and on discharge, we found that, despite a high adherence, drugs for secondary prevention in these patients are still not always routinely prescribed (Table 11), with beta-blockers being prescribed more on discharge in non-PCI hospitals (83.2% vs. 80.5%, p=0.004). Finally, we highlight the higher percentage of fibrinolysis (12.9% versus 2.1%, p-value <0.001) in patients admitted to non-PCI hospitals.
Therapeutic intervention during hospital admission on ST-elevation-acute coronary syndromes patients.
| General population (n=7698) | Patients in PCI-capable hospitals (n=4787) | Patients in non-PCI hospitals (n=2911) | P-value | |
|---|---|---|---|---|
| Fibrinolysis (n, %) | 384/6321 (6.1%) | 84/4004 (2.1%) | 300/2317 (12.9%) | <0.001 |
| Coronary angiography performed (n,%) | 7135/7698 (92.7%) | 4487/4787 (93.7%) | 2648/2911 (91%) | <0.001 |
| Angioplasty performed (n,%) | 6683/7693 (86.9%) | 4233/4784 (88.5%) | 2450/2909 (84.2%) | <0.001 |
| CABG (n,%) | 21/7691 (0.3%) | 12/4783 (0.3%) | 9/2908 (0.3%) | 0.633 |
| Medication in hospital (n,%) | ||||
| - ASA | 7491/7639 (98.1%) | 4617/4731 (97.6%) | 2874/2908 (98.8%) | <0.001 |
| - Ticagrelor | 1609/5933 (27.1%) | 1023/3675 (27.8%) | 586/2258 (26%) | 0.113 |
| - Clopidogrel | 6122/7670 (79.8%) | 3789/4764 (79.5%) | 2333/2906 (80.3%) | 0.428 |
| - ACEi or ARB II. | 6537/7672 (85.2%) | 4013/4768 (84.2%) | 2524/2904 (86.9%) | 0.001 |
| - Statin | 7246/7680 (94.3%) | 4529/4772 (94.9%) | 2717/2908 (93.4%) | 0.007 |
| - Beta-blocker | 6053/7668 (78.9%) | 3656/4765 (76.7%) | 2397/2903 (82.6%) | <0.001 |
| - A. aldosterone | 1036/7629 (13.6%) | 634/4737 (13.4%) | 402/2892 (13.9%) | 0.523 |
| - Digoxin | 106/7611 (1.4%) | 63/4725 (1.3%) | 43/2886 (1.5%) | 0.572 |
| - Amiodarone | 608/7613 (8%) | 382/4727 (8.1%) | 226/2886 (7.8%) | 0.696 |
| - Nitrates | 2163/7622 (28.4%) | 1089/4733 (23%) | 1074/2889 (37.2%) | <0.001 |
| Medication on discharge (n,%) | ||||
| - ASA | 6792/7118 (95.4%) | 4299/4488 (95.8%) | 2493/2630 (94.8%) | 0.052 |
| - Ticagrelor | 1400/5499 (25.5%) | 902/3451 (26.1%) | 498/2048 (24.3%) | 0.134 |
| - Clopidogrel | 5165/7102 (72.7%) | 3222/4477 (72%) | 1943/2625 (74%) | 0.061 |
| - ACEi or ARB II. | 6162/7107 (86.7%) | 3859/4480 (86.1%) | 2303/2627 (87.7%) | 0.067 |
| - Statin | 6766/7117 (95.1%) | 4276/4489 (95.3%) | 2490/2628 (94.7%) | 0.341 |
| - Beta-blocker | 5783/7096 (81.5%) | 3598/4471 (80.5%) | 2185/2625 (83.2%) | 0.004 |
| - A. aldosterone | 871/7077 (12.3%) | 543/4459 (12.2%) | 328/2618 (12.5%) | 0.664 |
| - Digoxin | 46/7070 (0.7%) | 27/4455 (0.6%) | 19/2615 (0.7%) | 0.543 |
| - Amiodarone | 217/7070 (3.1%) | 152/4455 (3.4%) | 65/2615 (2.5%) | 0.029 |
| - Nitrates | 687/7070 (%) | 444/4455 (10%) | 243/2615 (9.3%) | 0.356 |
A.aldosterone: aldosterone antagonist; ACEi: angiotensin-converting enzyme inhibitor; ARA II: angiotensin II receptor antagonists; ASA: acetylsalicylic acid; CABG: coronary artery bypass grafting; n: number of patients who meet studied criteria/number of patients who have information on this criterion.
After applying PS, we found similar results to those previously described (Table 12), but we continue to see a higher number of angioplasties performed (87.8% vs. 81.8%, p-value <0.001). It should also be noted that prescription of acetylsalicylic acid (96.5% vs. 94.4%, p=0.018) and statin (96.1% vs. 93.8%, p=0.013) is slightly higher in patients admitted to PCI-capable hospitals.
Therapeutic intervention during hospital admission on ST-elevation-acute coronary syndromes patients after application of propensity score.
| General population (n=2372) | Patients in PCI-capable hospitals (n=1186) | Patients in non-PCI hospitals (n=1186) | P-value | |
|---|---|---|---|---|
| Fibrinolysis (n, %) | 121/1885 (6.4%) | 19/988 (1.9%) | 102/897 (11.4%) | <0.001 |
| Coronary angiography performed (n,%) | 2154/2372 (90.8%) | 1102/1186 (92.9%) | 1052/1186 (88.7%) | <0.001 |
| Angioplasty performed (n,%) | 2009/2370 (84.8%) | 1040/1185 (87.8%) | 969/1185 (81.8%) | <0.001 |
| CABG (n,%) | 6/2372 (0.3%) | 4/1186 (0.3%) | 2/1186 (0.2%) | 0.453 |
| Medication in hospital (n,%) | ||||
| - ASA | 2343/2369 (98.9%) | 1172/1185 (98.9%) | 1171/1184 (98.9%) | 0.998 |
| - Ticagrelor | 535/1913 (28.0%) | 275/915 (30.1%) | 260/998 (26.1%) | 0.051 |
| - Clopidogrel | 1853/2364 (78.4%) | 930/1181 (78.7%) | 923/1183 (78.0%) | 0.699 |
| - ACEi or ARB II. | 2039/2366 (86.2%) | 998/1182 (84.4%) | 1041/1184 (87.9%) | 0.014 |
| - Statin | 2207/2369 (93.2%) | 1113/1184 (94.0%) | 1094/1185 (92.3%) | 0.105 |
| - Beta-blocker | 1875/2367 (79.2%) | 904/1182 (76.5%) | 971/1185 (81.9%) | 0.001 |
| - A. aldosterone | 347/2353 (14.7%) | 159/1174 (13.5%) | 188/1179 (15.9%) | 0.100 |
| - Digoxin | 29/2350 (1.2%) | 9/1174 (0.8%) | 20/1176 (1.7%) | 0.040 |
| - Amiodarone | 195/2351 (8.3%) | 79/1175 (6.7%) | 116/1176 (9.9%) | 0.006 |
| - Nitrates | 806/2352 (34.3%) | 286/1174 (24.4%) | 520/1178 (44.1%) | <0.001 |
| Medication on discharge (n,%) | ||||
| - ASA | 2087/2186 (95.5%) | 1077/1116 (96.5%) | 1010/1070 (94.4%) | 0.018 |
| - Ticagrelor | 467/1768 (26.4%) | 241/860 (28.0%) | 226/908 (24.9%) | 0.135 |
| - Clopidogrel | 1573/2182 (72.1%) | 819/1113 (73.6%) | 754/1069 (70.5%) | 0.112 |
| - ACEi or ARB II. | 1906/2183 (87.3%) | 973/1114 (87.3%) | 933/1069 (87.3%) | 0.964 |
| - Statin | 2076/2185 (95.0%) | 1073/1116 (96.1%) 890/1112 (80.0%) | 1003/1069 (93.8%) | 0.013 |
| - Beta-blocker | 1759/2181 (80.7%) | 133/1109 (12.0%) | 869/1069 (81.3%) | 0.458 |
| - A. aldosterone | 273/2173 (12.6%) | 2/1108 (0.2%) | 140/1064 (13.2%) | 0.413 |
| - Digoxin | 13/2173 (0.6%) | 34/1109 (3.1%) | 11/1065 (1.0%) | 0.010 |
| - Amiodarone | 68/2174 (3.1%) | 109/1108 (9.8%) | 34/1065 (3.2%) | 0.865 |
| - Nitrates | 233/2173 (10.7%) | 124/1065 (11.6%) | 0.174 |
A. aldosterone: aldosterone antagonist; ACEi: angiotensin-converting enzyme inhibitor; ARA II: angiotensin II receptor antagonists; ASA: acetylsalicylic acid; CABG: coronary artery bypass grafting; n: number of patients who meet studied criteria/number of patients who have information on this criterion.
84.2% of the population underwent CCTA, with 52.3% undergoing angioplasty. There is also a slight predominance of catheterization (86.8% vs. 82.2%, p<0.001) and angioplasties (54.6% vs. 50.4%, p<0.001) performed in non-PCI hospitals. A residual percentage (1%) of the population underwent aortic coronary revascularization surgery. As regards medication during hospitalization and discharge, we found that, as in STE-ACS, drugs for secondary prevention in these patients are still not always routinely prescribed. Note the higher prescription of beta-blockers (BB) (80.5% vs 77.1%, p<0.001) and angiotensin-converting enzyme inhibitors (ACEi)/angiotensin II receptor antagonists (ARA II) (85.1% versus 82.6%, p<0.001) in non-PCI hospitals (Table 13).
Therapeutic intervention during hospital admission on non-ST-elevation-acute coronary syndromes patients.
| General population (n=10091) | Patients in PCI-capable hospitals (n=5606) | Patients in non-PCI hospitals (n=4485) | P-value | |
|---|---|---|---|---|
| Coronary angiography performed (n,%) | 8498/10090 (84.2%) | 4605/5605 (82.2%) | 3893/4485 (86.8%) | <0.001 |
| Angioplasty performed (n,%) | 5263/10070 (52.3%) | 2817/5594 (50.4%) | 2446/4476 (54.6%) | <0.001 |
| CABG (n,%) | 78/10080 (0.8%) | 51/5600 (0.9%) | 27/4480 (0.6%) | 0.079 |
| Medication in hospital (n,%) | ||||
| - ASA | 9730/10032 (97%) | 5300/5549 (95.5%) | 4430/4483 (98.8%) | <0.001 |
| - Ticagrelor | 1452/8109 (17.9%) | 729/4137 (16.9%) | 723/3792 (19.1%) | 0.011 |
| - Clopidogrel | 7810/10040 (77.8%) | 4211/5566 (75.7%) | 3599/4474 (80.4%) | <0.001 |
| - ACEi or ARB II. | 8793/10051 (87.5%) | 4771/5577 (85.5%) | 4022/4474 (89.9%) | <0.001 |
| - Statin | 9643/10059 (95.9%) | 5332/5581 (95.5%) | 4311/4478 (96.3%) | 0.067 |
| - Beta-blocker | 8313/10033 (82.9%) | 4456/5566 (80.1%) | 3857/4467 (86.3%) | <0.001 |
| - A. aldosterone | 912/9988 (9.1%) | 500/5529 (9%) | 412/4459 (9.2%) | 0.735 |
| - Digoxin | 165/9991 (1.7%) | 104/5535 (1.9%) | 61/4456 (1.4%) | 0.047 |
| - Amiodarone | 644/9994 (6.4%) | 379/5538 (6.8%) | 265/4456 (5.9%) | 0.070 |
| - Nitrates | 5507/10002 (55.1%) | 2952/5542 (53.3%) | 2555/4460 (57.3%) | <0.001 |
| Medication on discharge (n,%) | ||||
| - ASA | 8551/9332 (91.6%) | 4758/5215 (91.2%) | 3793/4117 (92.1%) | 0.122 |
| - Ticagrelor | 1272/7513 (16.9%) | 656/4018 (16.3%) | 616/3495 (17.6%) | 0.134 |
| - Clopidogrel | 6205/9300 (66.7%) | 3396/5197 (65.3%) | 2809/4103 (68.5%) | 0.002 |
| - ACEi or ARB II. | 7809/9328 (83.7%) | 4301/5208 (82.6%) | 3508/4120 (85.1%) | <0.001 |
| - Statin | 8708/9333 (93.3%) | 4887/5217 (93.7%) | 3821/4119 (92.8%) | 0.065 |
| - Beta-blocker | 7319/9316 (78.6%) | 4009/5203 (77.1%) | 3310/4113 (80.5%) | <0.001 |
| - A. aldosterone | 756/9260 (8.2%) | 413/5163 (8%) | 343/4097 (8.4%) | 0.515 |
| - Digoxin | 85/9255 (0.9%) | 54/5161 (1%) | 31/4094 (0.8%) | 0.148 |
| - Amiodarone | 346/9264 (3.7%) | 229/5166 (4.4%) | 117/4098 (2.9%) | <0.001 |
| - Nitrates | 2663/9271 (28.7%) | 1635/5170 (31.6%) | 1028/4101 (25.1%) | <0.001 |
A.aldosterone: aldosterone antagonist; ACEi: angiotensin-converting enzyme inhibitor; ARA II: angiotensin II receptor antagonists; ASA: acetylsalicylic acid; CABG: coronary artery bypass grafting; n: number of patients who meet studied criteria/number of patients who have information on this criterion.
After applying PS, we found an absence of statistical significance between hospitals with and without PCI capabilities in relation to the number of catheterizations and angioplasties performed. We also observed an absence of differences regarding secondary prevention medication, namely ACEi/ARA and BBs (Table 14).
- ✓
Cardiovascular complications and in-hospital mortality
Therapeutic intervention during hospital admission on non-ST-elevation-acute coronary syndromes patients after application of propensity score.
| General population (n=3636) | Patients in PCI-capable hospitals (n=1818) | Patients in non-PCI hospitals (n=1818) | P-value | |
|---|---|---|---|---|
| Coronary angiography performed (n,%) | 3041/3636 (83.6%) | 1509/1818 (83.0%) | 1532/1818 (84.3%) | 0.303 |
| Angioplasty performed (n,%) | 1909/3631 (52.6%) | 948/1815 (52.2%) | 961/1816 (52.9%) | 0.678 |
| CABG (n,%) | 28/3635 (0.8%) | 15/1818 (0.8%) | 13/1817 (0.7%) | 0.705 |
| Medication in hospital (n,%) | ||||
| - ASA | 3561/3633 (98.0%) | 1771/1815 (97.6%) | 1790/1818 (98.5%) | 0.056 |
| - Ticagrelor | 583/3010 (19.4%) | 258/1397 (18.5%) | 325/1613 (20.1%) | 0.245 |
| - Clopidogrel | 2726/3627 (75.2%) | 1326/1812 (73.2%) | 1400/1815 (77.1%) | 0.006 |
| - ACEi or ARB II. | 3138/3629 (86.5%) | 1539/1813 (84.9%) | 1599/1816 (88.1%) | 0.005 |
| - Statin | 3460/3632 (95.3%) | 1727/1815 (95.2%) | 1733/1817 (95.4%) | 0.749 |
| - Beta-blocker | 3018/3623 (83.3%) | 1455/1813 (80.3%) | 1563/1810 (86.4%) | <0.001 |
| - A. aldosterone | 303/3615 (8.4%) | 148/1804 (8.2%) | 155/1811 (8.6%) | 0.700 |
| - Digoxin | 59/3612 (1.6%) | 35/1803 (1.9%) | 24/1809 (1.3%) | 0.145 |
| - Amiodarone | 208/3611 (5.8%) | 105/1802 (5.8%) | 103/1809 (5.7%) | 0.864 |
| - Nitrates | 2170/3616 (60.0%) | 1027/1805 (56.9%) | 1143/1811 (63.1%) | <0.001 |
| Medication on discharge (n,%) | ||||
| - ASA | 3055/3342 (91.4%) | 1550/1694 (91.5%) | 1505/1648 (91.3%) | 0.855 |
| - Ticagrelor | 516/2767 (18.6%) | 235/1295 (18.1%) | 281/1472 (19.1%) | 0.525 |
| - Clopidogrel | 2236/3332 (67.1%) | 1138/1689 (67.4%) | 1098/1643 (66.8%) | 0.736 |
| - ACEi or ARB II. | 2771/3342 (82.9%) | 1391/1693 (82.2%) | 1380/1649 (83.7%) | 0.242 |
| - Statin | 3102/3342 (92.8%) | 1584/1693 (93.6%) | 1518/1649 (92.1%) | 0.092 |
| - Beta-blocker | 2616/3337 (78.4%) | 1308/1690 (77.4%) | 1308/1647 (79.4%) | 0.156 |
| - A. aldosterone | 253/3325 (7.6%) | 120/1684 (7.1%) | 133/1641 (8.1%) | 0.287 |
| - Digoxin | 33/3320 (1.0%) | 18/1681 (1.1%) | 15/1639 (0.9%) | 0.651 |
| - Amiodarone | 102/3320 (3.1%) | 56/1681 (3.3%) | 46/1639 (2.8%) | 0.381 |
| - Nitrates | 974/3327 (29.3%) | 550/1684 (32.7%) | 424/1643 (25.8%) | <0.001 |
A.aldosterone: aldosterone antagonist; ACEi: angiotensin-converting enzyme inhibitor; ARA II: angiotensin II receptor antagonists; ASA: acetylsalicylic acid; CABG: coronary artery bypass grafting; n: number of patients who meet studied criteria/number of patients who have information on this criterion.
In analyzing cardiovascular events (Table 15), we concluded that PCI-capable hospitals presented more cases of cardiogenic shock (7.1% vs. 5.7%, p=0.013) and cardiorespiratory arrest (6.2% vs. 24.9%, p=0.015), while non-PCI hospitals presented more episodes of mechanical complications (1.7% vs. 1.1%, p=0.029).
Cardiovascular complications and in-hospital mortality of patients admitted with ST--elevation acute coronary syndromes.
| General population (n=7698) | Patients in PCI-capable hospitals (n=4787) | Patients in non-PCI hospitals (n=2911) | P-value | OR (95% CI) | |
|---|---|---|---|---|---|
| LVEF (%, mean ± standard deviation) | 50 ± 12 | 51 ± 12 | 48 ± 12 | <0.001 | – |
| Re-infarction (n,%) | 63/7680 (0.8%) | 37/4771 (0.8%) | 26/2909 (0.9%) | 0.557 | 1.15 (0.7–1.91) |
| CHF (n,%) | 1386/7680 (18%) | 881/4771 (18.5%) | 505/2909 (17.4%) | 0.222 | 0.93 (0.82–1.05) |
| Cardiogenic shock (n,%) | 501/7652 (6.5%) | 337/4751 (7.1%) | 164/2901 (5.7%) | 0.013 | 0.78 (0.65–0.95) |
| AF (n,%) | 483/7680 (6.3%) | 297/4771 (6.2%) | 186/2909 (6.4%) | 0.767 | 1.03 (0.85–1.24) |
| Mechanical complications (n,%) | 99/7680 (1.3%) | 51/4771 (1.1%) | 48/2909 (1.7%) | 0.029 | 1.55 (1.04–2.31) |
| AV block (n,%) | 403/7678 (5.2%) | 253/4769 (5.3%) | 150/2909 (5.2%) | 0.777 | 0.97 (0.79–1.19) |
| Sustained VT (n,%) | 218/7680 (2.8%) | 129/4771 (2.7%) | 89/2909 (3.1%) | 0.363 | 1.14 (0.86–1.49) |
| CRA (n,%) | 441/7680 (5.7%) | 298/4771 (6.2%) | 143/2909 (4.9%) | 0.015 | 0.78 (0.63–0.95) |
| Major bleeding (n,%) | 164/7679 (2.1%) | 111/4770 (2.3%) | 53/2909 (1.8%) | 0.137 | 0.78 (0.56–1.08) |
| Death (n,%) | 393/7697 (5.1%) | 254/4787 (5.3%) | 139/2910 (4.8%) | 0.306 | 0.90 (0.72–1.11) |
| Days admitted (minutes, median, (P25;P75)) | 4 (3;5) | 4 (3;5) | 4 (3;6) | 0.002 | – |
95%CI: 95% confidence interval; AF: atrial fibrillation; AV block: auriculus-ventricular block; CHF: congestive heart failure; CRA: cardiorespiratory arrest; LVEF: left ventricular ejection fraction; n: number of patients who meet the criteria studied/number of patients who have information about this criterion; Non-PCI: hospitals without percutaneous coronary intervention capabilities; OR: odds ratio; PCI-capable: hospitals with percutaneous coronary intervention capabilities; VT: ventricular tachycardia.
A PS was applied to our population (Table 16), and we found that patients admitted to non-PCI hospitals had more episodes of sustained ventricular tachycardia (3.7% vs. 1.8%, p<0.001), with more cases of compromised (<50%) left ventricular ejection fraction (48.1% vs. 39.4%, p<0.001). A longer stay in non-PCI hospitals was identified, but no differences were observed between the two groups relating to in-hospital mortality.
Cardiovascular complications and in-hospital mortality of patients admitted with ST--elevation acute coronary syndromes after application of propensity score.
| General population (n=2372) | Patients in PCI-capable hospitals (n=1186) | Patients in non-PCI hospitals (n=1186) | P-value | OR (95% CI) | |
|---|---|---|---|---|---|
| LVEF (%, mean ± standard deviation) | 50 ± 12 | 52 ± 12 | 49 ± 12 | 0.002 | – |
| Re-infarction (n,%) | 23/2371 (1.0%) | 12/1185 (1.0%) | 11/1186 (0.9%) | 0.832 | 0.92 (0.40–2.08) |
| CHF (n,%) | 395/2371 (16.7%) | 198/1185 (16.7%) | 197/1186 (16.6%) | 0.949 | 0.99 (0.80–1.23) |
| Cardiogenic shock (n,%) | 129/2366 (5.5%) | 70/1182 (5.9%) | 59/1184 (5.0%) | 0.314 | 0.83 (0.58–1.19) |
| AF (n,%) | 152/2371 (6.4%) | 68/1185 (5.7%) | 84/1186 (7.1%) | 0.182 | 1.25 (0.90–1.74) |
| Mechanical complications (n,%) | 26/2371 (1.1%) | 12/1185 (1.0%) | 14/1186 (1.2%) | 0.695 | 1.17 (0.54–2.54) |
| AV block (n,%) | 125/2370 (5.3%) | 65/1184 (5.5%) | 60/1186 (5.1%) | 0.639 | 0.92 (0.64–1.32) |
| Sustained VT (n,%) | 65/2371 (2.7%) | 21/1185 (1.8%) | 44/1186 (3.7%) | 0.004 | 2.14 (1.26–3.61) |
| CRA (n,%) | 132/2371 (5.6%) | 75/1185 (6.3%) | 57/1186 (4.8%) | 0.106 | 0.75 (0.52–1.06) |
| Major bleeding (n,%) | 39/2371 (1.6%) | 24/1185 (2.0%) | 15/1186 (1.3%) | 0.145 | 0.62 (0.32–1.19) |
| Death (n,%) | 105/2371 (4.4%) | 56/1186 (4.7%) | 49/1185 (4.1%) | 0.487 | 0.87 (0.59–1.29) |
| Days admitted (minutes, median, (P25;P75)) | 4 (3;5) | 4 (3;5) | 4 (3;6) | 0.179 | – |
95%CI: 95% confidence interval; AF: atrial fibrillation; AV block: auriculus-ventricular block; CHF: congestive heart failure; CRA: cardiorespiratory arrest; LVEF: left ventricular ejection fraction; n: number of patients who meet the criteria studied/number of patients who have information about this criterion; Non-PCI: hospitals without percutaneous coronary intervention capabilities; OR: odds ratio; PCI-capable: hospitals with percutaneous coronary intervention capabilities; VT: ventricular tachycardia.
Regarding this population (Table 17), we found that PCI-capable hospitals had more cases of CHF (14.6% vs. 11.7%, p<0.001), while non-PCI hospitals had more episodes of sustained VT (0.7% vs. 1.1%, p=0.020).
Cardiovascular complications and in-hospital mortality of patients admitted with non-ST-elevation-acute coronary syndromes.
| General population (n=10091) | Patients in PCI-capable hospitals (n=5606) | Patients in non-PCI hospitals (n=4485) | P-value | OR (95% CI) | |
|---|---|---|---|---|---|
| LVEF (%, mean ± standard deviation) | 53 ± 12 | 54 ± 12 | 52 ± 12 | <0.001 | – |
| Re-infarction (n,%) | 118/10053 (1.2%) | 61/5568 (1.1%) | 57/4485 (1.3%) | 0.417 | 1.16 (0.81–1.67) |
| CHF (n,%) | 1335/10054 (13.3%) | 812/5569 (14.6%) | 523/4485 (11.7%) | <0.001 | 0.77 (0.69–0.87) |
| Cardiogenic shock (n,%) | 173/10022 (1.7%) | 95/5544 (1.7%) | 78/4478 (1.7%) | 0.914 | 1.02 (0.75–1.38) |
| AF (n,%) | 392/10053 (3.9%) | 224/5568 (4%) | 168/4485 (3.7%) | 0.475 | 0.93 (0.76–1.14) |
| Mechanical complications (n,%) | 27/10053 (0.3%) | 14/5568 (0.3%) | 13/4485 (0.3%) | 0.711 | 1.15 (0.54–2.46) |
| AV block (n,%) | 134/10054 (1.3%) | 79/5569 (1.4%) | 55/4485 (1.2%) | 0.403 | 0.86 (0.61–1.22) |
| Sustained VT (n,%) | 88/10052 (0.9%) | 38/5567 (0.7%) | 50/4485 (1.1%) | 0.021 | 1.64 (1.07–2.51) |
| CRA (n,%) | 113/10054 (1.1%) | 60/5569 (1.1%) | 53/4485 (1.2%) | 0.622 | 1.10 (0.76–1.59) |
| Major bleeding (n,%) | 124/10054 (1.2%) | 84/5569 (1.5%) | 40/4485 (0.9%) | 0.005 | 0.59 (0.40–0.86) |
| Death (n,%) | 219/10091 (2.2%) | 115/5606 (2.1%) | 104/4485 (2.3%) | 0.360 | 1.13 (0.87–1.48) |
| Days admitted (minutes, median, (P25;P75)) | 4 (3;6) | 4 (2;6) | 4 (3;7) | <0.001 | – |
95%CI: 95% confidence interval; AF: atrial fibrillation; AV block: auriculus-ventricular block; CHF: congestive heart failure; CRA: cardiorespiratory arrest; LVEF: left ventricular ejection fraction; n: number of patients who meet the criteria studied/number of patients who have information about this criterion; Non-PCI: hospitals without percutaneous coronary intervention capabilities; OR: odds ratio; PCI-capable: hospitals with percutaneous coronary intervention capabilities; VT: ventricular tachycardia.
After application of PS, a higher incidence of CHF (12.3% vs. 10%, p=0.003) was observed in patients admitted to PCI-capable hospitals (Table 13). A longer stay in non-PCI hospitals was identified, but no differences were observed between the two groups relating to in-hospital mortality (Table 18).
Cardiovascular complications and in-hospital mortality of patients admitted with non-ST-elevation-acute coronary syndromes after application of propensity score.
| General population (n=3636) | Patients in PCI-capable hospitals (n=1818) | Patients in non-PCI hospitals (n=1818) | P-value | OR (95% CI) | |
|---|---|---|---|---|---|
| LVEF (%, mean ± standard deviation) | 54 ± 12 | 55 ± 12 | 53 ± 12 | <0.001 | – |
| Re-infarction (n,%) | 46/3625 (1.3%) | 20/1807 (1.1%) | 26/1818 (1.4%) | 0.385 | 1.30 (0.72–2.33) |
| CHF (n,%) | 404/3625 (11.1%) | 222/1807 (12.3%) | 182/1818 (10.0%) | 0.030 | 0.79 (0.65–0.98) |
| Cardiogenic shock (n,%) | 60/3616 (1.7%) | 31/1801 (1.7%) | 29/1815 (1.6%) | 0.771 | 0.93 (0.56–1.54) |
| AF (n,%) | 110/3625 (3.0%) | 56/1807 (3.1%) | 54/1818 (3.0%) | 0.821 | 0.96 (0.65–1.40) |
| Mechanical complications (n,%) | 10/3625 (0.3%) | 4/1807 (0.2%) | 6/1818 (0.3%) | 0.754 | 1.49 (0.42–5.30) |
| AV block (n,%) | 42/3626 (1.2%) | 19/1808 (1.1%) | 23/1818 (1.3%) | 0.547 | 1.21 (0.65–2.22) |
| Sustained VT (n,%) | 33/3624 (0.9%) | 11/1806 (0.6%) | 22/1818 (1.2%) | 0.057 | 2.00 (0.97–4.13) |
| CRA (n,%) | 39/3626 (1.1%) | 19/1808 (1.1%) | 20/1818 (1.1%) | 0.886 | 1.05 (0.56–1.97) |
| Major bleeding (n,%) | 41/3625 (1.1%) | 24/1807 (1.3%) | 17/1818 (0.9%) | 0.263 | 0.70 (0.38–1.31) |
| Death (n,%) | 80/3636 (2.2%) | 38/1818 (2.1%) | 42/1818 (2.3%) | 0.651 | 1.11 (0.71–1.74) |
| Days admitted (minutes, median, (P25;P75)) | 4 (2;6) | 3 (2;6) | 4 (3;7) | <0.001 | – |
95%CI: 95% confidence interval; AF: atrial fibrillation; AV block: atrio-ventricular block; CHF: congestive heart failure; CRA: cardiorespiratory arrest; LVEF: left ventricular ejection fraction; n: number of patients who meet the criteria studied/number of patients who have information about this criterion; Non-PCI: hospitals without percutaneous coronary intervention capabilities; OR: odds ratio; PCI-capable: hospitals with percutaneous coronary intervention capabilities; VT: ventricular tachycardia.
Time-to-myocardial reperfusion is crucial for the prognosis of patients admitted in the context of ACS.7,11 However, we continue to deal with numerous logistical difficulties, which lead to avoidable delays both at the pre-hospital and hospital level,5,12,13 and it is difficult to meet the times defined in the most recent ESC guidelines.3,4 It should also be noted that despite reinforced awareness campaigns in the media, with the international literature presenting contradictory results as to the applicability of these measures,14,15 the Portuguese population is still not fully aware of the prognostic impact that the delay until revascularization can have.
In our analysis, there is marked asymmetry, in relation to STE-ACS, between hospitals with and without on-site PCI capabilities, with the latter presenting a time until revascularization of about 69 min longer (72 min after applying PS). Nevertheless, we observed that even in PCI-capable hospitals, the first contact-to-balloon time for STE-ACS is 27 min (26 min after applying PS) higher than that defined in international recommendations, as well as a fibrinolysis rate of 2.1% (1.9% after PS). This shows that the time delay problem applies to any hospital scenario. However, the particular situations that justify this delay in PCI-capable hospitals are unknown, and could include delays in patient admission, unavailability of the cath lab, or a patient presenting without vascular access. This requires analysis beyond the information contained in the registry.
With regard to NSTE-ACS, some studies have shown that the geographic location of an ACS occurrence is associated with temporal barriers16–19 that may impact access to the most appropriate medical intervention and, consequently, lead to an increase in mortality. However, the association between admission to hospitals with/without PCI and cardiovascular events remains uncertain, especially in patients whose time window for intervention is wider, except in high-risk cases. Analyzing the times recorded in our registry, we encountered the existence of a temporal asymmetry between the two groups, with the non-PCI hospital group presenting a longer time period, partially justified by the physical distance to the cath lab and logistical situations, such as the availability of transportation and medical transport staff. However, in the present analysis, it was not possible to stratify the risk in NSTE-ACS, as the presence of a reliable association between the time until catheterization and the occurrence of cardiovascular complications could not be assessed.
Our study also found that more than 1/3 of the population continue to travel to hospital by their own means and only 27.4% (20.4% post-PS) of patients with STE-ACS were transported by a pre-hospital medical team. These data become even more worrying when we consider that approximately 1/5 of the population had already presented with a previous coronary event and that in 3% (4.1% post-PS) of transfers via the coronary FTS, the patients were transferred to a non-PCI hospital. These data may justify a more detailed assessment in order to understand whether the implementation of new health measures and policies is justified, both for the general public and directed at the health professionals themselves, in a pre-hospital and hospital environment.
The identified asymmetry with regard to the access to coronary revascularization and consequent disadvantage for patients admitted to non-PCI hospitals may be reflected in worse cardiovascular events and increased in-hospital mortality.11,20–22
In fact, we found that most patients underwent CCTA and more than half underwent PCI. Regarding the occurrence of major cardiovascular events, in the recording and analysis undertaken on patients with STE-ACS, PCI-capable hospitals were shown to present a higher number of patients with cardiogenic shock and aborted cardio-respiratory arrest. These findings can be explained mainly by the fact that the most unstable patients are transferred/transported to hospitals with immediate coronary intervention capability. There was also a predominance of mechanical complications in non-PCI hospitals, which may be explained by the longer “symptoms to reperfusion” time. However, this asymmetry between populations with different degrees of severity makes extrapolating any conclusions difficult. Thus, we applied a PS to homogenize the populations under study, despite the clear limitation of removing very serious patients from the most severe group and the healthier patients from the least severe group. We observed, after use of the PS, that non-PCI hospitals presented more arrhythmic events. This can be explained by the fact that patients admitted to this type of hospital have a higher median “admission to catheterization” time, and this is an arrhythmogenic substrate and myocardial injury that cannot be disregarded.5,23,24
It should also be noted that, after using logistic regression, it was found that admission to a non-PCI hospital does not in itself represent an independent predictive factor for prognosis in these patients, as other factors, such as time until revascularization, play a more important role in this context.
For NSTE-ACS, at admission, there was a higher percentage of patients with CHF in PCI-capable hospitals, even after the application of PS, which may be explained by the immediate admission or transfer of more severe patients to these sites, with the presence of CHF being a criterion for earlier intervention. The higher percentage of patients with ventricular arrhythmias in non-PCI hospitals could be justified by them being exposed to a longer period of ischemia. Nevertheless, after homogenization of the two groups, no differences in dysrhythmic events were observed.
Study limitationsThe present study is an observational study based on data from a retrospective and non-randomized registry. Despite the inclusion of a significant number of sites, the current registry does not include all sites in Portugal with cardiology departments, which could lead to a potential selection bias of the data analyzed.
Two other potential sources of selection bias were the non-inclusion of patients admitted to departments other than cardiology, and patients who died before admission to a cardiology department, neither of which are included in the National Registry.
The impossibility of categorizing NSTE-ACS according to clinical indication (emergent, urgent or up to 72 h), due to the absence of some variables in the national registry, is an important limitation in this group. It does not allow the impact to be assessed for each subgroup, and only one overall assessment is possible in the present study.
Applying a PS is in itself a limitation, as by pairing the total sample, very seriously ill patients are removed from the most severe group and the healthier patients from the least severe group.
In conclusion, the objective of our study was to assess cardiovascular events and short-term mortality, and as such it is not possible to extrapolate data to the medium and long term.
ConclusionOur analysis based on a clinical registry of ACS in Portugal shows that the treatment of ACS is in line with the most recent scientific recommendations, although there are time delays even in hospitals with cath labs. As a result, continuous in-hospital monitoring of all episodes of ACS and protocol reinforcement among pre-hospital teams, emergency services and inter-hospital transport networks, together with public awareness campaigns, are crucial to improving care for these patients.
ThanksThe authors would like to thank all the researchers at the National Registry of Acute Coronary Syndromes for their support in the preparation of this article. The authors would also like to thank Dr Adriana Belo (Head of the Statistics Department of the Portuguese Society of Cardiology) for the preparation of this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Miranda H, Sousa C, Santos H, Almeida I, Chin J, Almeida S, et al. Qual o verdadeiro impacto da intervenção coronária percutânea on-site? Análise de score de propensão de doentes admitidos por síndrome coronária aguda. Rev Port Cardiol. 2021;40:169–188.