Carbon monoxide (CO) poisoning is one of the most common types of poisoning and the leading cause of death by poisoning worldwide. Cardiac injury caused by CO poisoning has been little described despite being a predictor of poor prognosis.
We present the case of a healthy 24-year-old woman, admitted to our emergency room due to an episode of lipothymia without loss of consciousness. She reported holocranial headache for the previous two weeks associated with nausea and vomiting.
Laboratory tests revealed blood gas analysis: pH 7.392, pCO2 32 mmHg, pO2 101 mmHg, lactate 3.5 mmol/l, HCO3 20.8 mmol/l; COHb 29.2%; serial troponin I 1.21→5.25→6.13→3.65 μg/l; myoglobin 1378→964→352 μg/l; and NT-proBNP 1330 pg/l. The electrocardiogram showed sinus rhythm, heart rate 110 bpm, and ST-segment depression of 2 mm in V4 and 1 mm in V5. Transthoracic echocardiography revealed a left ventricle with normal wall motion and preserved ejection fraction.
Given the clinical and epidemiological context, myocardial and central nervous system ischemia due to prolonged CO exposure was assumed and normobaric oxygen therapy was immediately started. In view of evidence of injury to two major organ systems the indication for hyperbaric oxygen therapy was discussed with a specialist colleague, who suggested maintaining conservative treatment with oxygen therapy and in-hospital monitoring for 72 h. The patient was discharged on the third day and was still asymptomatic at 400 days of follow-up.
Besides symptoms and signs of central nervous system dysfunction, myocardial damage should also always be considered in the context of CO poisoning. Hyperbaric therapy is still controversial and the lack of objective data highlights the need for new randomized studies.
A intoxicação por monóxido de carbono (MC) é um dos tipos de intoxicação mais frequente e a principal causa de morte por intoxicação no mundo. A lesão cardíaca provocada pela intoxicação por MC tem sido pouco descrita apesar de ser um fator preditor de mau prognóstico.
Apresentamos o caso de uma mulher de 24 anos, saudável, que recorre ao serviço de urgência por lipotimia sem perda de conhecimento. Referia cefaleia holocraniana associada a náuseas e vómitos com duas semanas de evolução. Analiticamente: gasimetria pH 7,392; pCO2 32 mmHg, pO2 101 mmHg, lactatos 3,5 mmol/L, HCO3 20,8 mmol/L, COHb 29,2%; troponina I seriada 1,21→5,25→6,13→3,65 ug/L, mioglobina 1378→964→352 ug/L, NT-ProBNP 1330 pg/L. Eletrocardiograma: ritmo sinusal, frequência cardíaca 110 bpm, depressão do segmento ST de 2 mm em V4 e 1 mm em V5. Ecocardiograma transtorácico: ventrículo esquerdo sem alterações da cinética segmentar e boa função sistólica global.
Associando-se a clínica ao contexto epidemiológico assumiu-se isquemia do miocárdio e do sistema nervoso central por exposição prolongada ao MC. Iniciou-se prontamente oxigenoterapia normobárica. Perante a evidência de compromisso de dois órgãos nobres, foi discutida com o colega especialista nesta área a indicação para tratamento com oxigénio hiperbárico, sugeriu manter tratamento conservador com oxigenoterapia e vigilância em internamento durante 72 h. Teve alta ao terceiro dia e mantém-se assintomática aos 400 dias de follow-up.
Tal como os sintomas e sinais de disfunção do sistema nervoso central, a lesão do miocárdio deve ser sistematicamente equacionada no contexto de intoxicação por MC. A indicação para terapêutica em câmara hiperbárica permanece controversa e com indicações pouco objetivas, a apelar a novos estudos aleatorizados.
Carbon monoxide (CO) is a colorless, tasteless, odorless and non-irritant but highly toxic gas.1 It binds rapidly to hemoglobin with an affinity 210 times higher than for oxygen, leading to the formation of carboxyhemoglobin (COHb) and tissue hypoxia.
CO poisoning is one of the most common types of poisoning; it is a frequent cause of morbidity,2 and the leading cause of death by poisoning worldwide.3
While not a common cause of hospital admission in Portugal, its incidence is not negligible: 5.86/100000 population over an eight-year period.4
The clinical symptoms of CO poisoning are non-specific and can mimic a wide range of conditions, and diagnosis requires a high index of suspicion.1
Headache is the most common symptom of CO poisoning, reported in 84% of cases, and 50% of patients present fatigue, nausea, mental confusion and dyspnea.1 Less frequent symptoms include abdominal pain, visual disturbances, chest pain and seizures.1
Tissue hypoxia in CO poisoning affects all organs and systems, and involvement of the major organs worsens prognosis.
The neurological sequelae of CO poisoning have been amply described in the literature, but cardiovascular repercussions have only been presented in occasional case reports.5,6
Cardiac injury results from the binding of CO to hemoglobin and myoglobin and inhibition of mitochondrial cytochrome oxidase, resulting in tissue hypoxia and reduced adenosine triphosphate synthesis.7
The most common cardiac manifestations are ischemia leading to elevated myocardial necrosis markers, electrocardiographic (ECG) alterations, particularly ST-segment depression, myocardial infarction and conduction disturbances such as atrial fibrillation and ventricular arrhythmias.8
The authors present a case of CO poisoning with cardiac compromise with the aim of highlighting the seriousness of this complication, which is frequently overlooked, and the need for thorough investigation and monitoring in all cases of CO poisoning. The indication for hyperbaric therapy is also discussed in this context.
Case reportA 27-year-old woman, with no relevant clinical history or cardiovascular risk factors and not taking any medication, was admitted to the emergency room (ER) due to an episode of lipothymia, during which she was unable to move for around two hours following a bath. She denied loss of consciousness, tonic–clonic movements, loss of sphincter control, chest pain or palpitations. She reported holocranial headache for the previous two weeks, which she quantified as 6 on a scale of 1 to 10, associated with nausea and vomiting.9
From an epidemiological standpoint, the patient was accompanied by two other women who lived in the same building and had similar symptoms. They also reported that a dog living in the same place was suffering from collapse and vomiting. There was no other relevant history.
On physical examination, the patient was conscious, cooperative, and oriented in time and space, with blood pressure 109/69 mmHg, regular heart rate (HR) 109 bpm, and no other significant alterations.
Blood gas analysis on room air revealed pH 7.392, pCO2 32 mmHg, pO2 101 mmHg, HCO3 20.8 mmol/l, COHb 29.2% and lactate 3.5 mmol/l.
Table 1 shows changes in laboratory values over the patient's three-day hospital stay. Of note are the rises in markers of myocardial necrosis (peak troponin 6.13 μg/l, 9 h after the event), and in NT-proBNP, which normalized on the third day.
Changes in laboratory values during hospital stay.
| H0 | H6 | H9 | H20 | D1 | D2 | D3 | |
|---|---|---|---|---|---|---|---|
| Hemoglobin (g/dl) | 14.0 | 12.7 | – | – | 12.5 | 13.4 | – |
| Leukocytes (×109/l)/neutrophils (%) | 25.8/93.8 | 17.6/13.1 | – | – | 10.1/47.7 | 9.8/5.7 | – |
| C-reactive protein (mg/dl) | <0.29 | – | – | 0.55 | 0.38 | <0.5 | – |
| Creatininemia (mg/dl) | 0.61 | – | – | – | 0.53 | 0.67 | – |
| Troponinemia (μg/l) | 1.21 | 5.25 | 6.13 | 3.65 | 2.69 | 1.46 | 0.62 |
| Creatine kinase (U/l) | – | – | 2164 | – | 3058 | – | 791 |
| Myoglobinemia (μg/l) | – | 1378 | 964 | 352 | 96 | 19 | 24 |
| NT-proBNP (pg/ml) | – | – | – | 1330 | – | 384 | 48 |
D1: one day after event; D2: two days after event; D3: three days after event; H0: at emergency room admission; H6: 6 h after event; H9: 9 h after event; H20: 20 h after event.
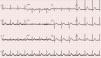
The ECG on admission to the ER (Figure 1) showed sinus rhythm, HR 110 bpm, normal P-wave amplitude and duration, with a 1:1 A/V ratio, PR interval 131 ms, QRS duration 90 ms, and ST-segment depression of 2 mm in V4 and 1 mm in V5.
The ECG 15 h after ER admission (Figure 2) showed sinus rhythm and normal HR of 78 bpm.
Transthoracic echocardiography showed no left ventricular dilatation, hypertrophy or wall motion abnormalities, good global systolic function and ejection fraction of 65%; good right ventricular systolic function and tricuspid annular plane systolic excursion of 16 mm; the other cardiac chambers were normal. There were no valve abnormalities, pericardial effusion or intracavitary masses.
Given the clinical and epidemiological context, myocardial and central nervous system ischemia due to CO poisoning following prolonged exposure was assumed. Normobaric oxygen therapy was started while the indication for hyperbaric oxygen therapy was discussed with the specialist responsible for the hyperbaric chamber, who suggested maintaining conservative treatment and monitoring for 72 h.
The patient's clinical course was favorable and she was discharged, asymptomatic, on the third day. Laboratory tests revealed a fall in markers of myocardial necrosis and normalization of NT-proBNP (Table 1). Blood gas analysis on room air showed pH 7.436, pCO2 35 mmHg, pO2 120 mmHg, COHb 0.5% and HCO3 23 mmol/l.
DiscussionThe case presented describes a less common complication of CO poisoning – myocardial and central nervous system ischemia. The former is often overlooked, with few and conflicting reports in the literature on the therapeutic approach to adopt.
A search in Medline for articles on this subject published since January 1st, 2000 produced 299 articles with the search term “carbon monoxide poisoning”, 18 articles with “carbon monoxide poisoning and neurological effects” and 12 articles with “carbon monoxide poisoning and myocardial injury”, which demonstrates the low level of attention paid to this subject.
A study based on autopsies performed by the Portuguese National Institute of Legal Medicine over a six-year period from 2005 to 2011 recorded 111 deaths from CO poisoning – 55 in the North region, 12 in the Central region and 44 in the South region. Most deaths were the result of accidents in the home with open fires, charcoal braziers and gas water heaters, as was the case with our patient.10 The study did not specify the degree of injury to different organs.
Hampson et al. demonstrated that there was no significant difference in short-term mortality from CO poisoning between patients treated with normobaric or hyperbaric oxygen therapy, the aim of the latter being to prevent permanent organ damage.11 The indications for hyperbaric oxygen therapy remain the subject of debate and are currently restricted (Table 2).
Indications for hyperbaric oxygen therapy.12
| Loss of consciousness |
| Neurological deficits |
| Ischemic cardiac changes |
| Metabolic acidosis |
| Carboxyhemoglobin >25% |
According to the latest international guidelines hyperbaric oxygen therapy should be used in all patients with severe CO poisoning, severity being assessed on indicators of organ damage rather than simply on levels of COHb (Table 2).12,1 The myocardial ischemia observed in our patient is one of these indicators.
Satran et al. demonstrated that myocardial injury is common in moderate to severe CO poisoning. In a prospective study between January 1, 1994 and January 1, 2002, with follow-up to November 11, 2005, they reviewed the cardiovascular manifestations of 230 consecutive patients admitted for moderate to severe CO poisoning to a hospital with facilities for hyperbaric oxygen therapy. Mean age was 47.2 years and 72% were male. Of the total study population, 37% (85 patients) had myocardial injury assessed by ECG or biomarkers despite a low incidence of cardiac risk factors, as was the case in our patient. The study showed that cardiac damage is often underestimated in CO poisoning: serial assessment of cardiac biomarkers was not performed in 20% of patients and echocardiograms were performed in only 53 of those with positive markers.13
Henry et al. assessed long-term mortality (follow-up 3–11 years) in the same population of 85 patients admitted for CO poisoning with associated myocardial injury. Of these, 38% died, compared to 15% of those with no myocardial injury (odds ratio 2.1; 95% confidence interval 1.2–3.7; p=0.009). They concluded that the risk of mortality in patients with CO poisoning and cardiac involvement is twice that of patients without myocardial injury and three times that of controls with no history of CO poisoning.14
In the case presented, prolonged CO exposure, elevated markers of myocardial necrosis and loss of consciousness, indicators of central nervous system and myocardial damage, led us to classify the CO poisoning as severe and to consider hyperbaric oxygen therapy. However, the severity of organ damage is based on the assessment of a specialist in hyperbaric medicine, who in this case, given the patient's clinical stability, advised maintaining normobaric oxygen therapy and close monitoring.
The clinical course was favorable on high flow oxygen therapy, and the patient survived and was still asymptomatic in cardiovascular terms at 400 days of follow-up.
Despite the scarcity of data in the literature, CO poisoning is common. Prognosis can be poor, and appears to be dictated by the extent of involvement of the myocardium as well as of the central nervous system. There have been few studies and the guidelines, as their authors acknowledge, are unclear due to lack of evidence, particularly concerning the benefits of hyperbaric oxygen therapy and its indications.
Cardiac involvement is often underdiagnosed or overlooked, which highlights the need to raise awareness of this complication among health professionals, and of its implications for prognosis.
New randomized studies are required to establish evidence-based guidelines.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cardiga R, Proença M, Carvalho C, et al. Intoxicação por monóxido de carbono com compromisso cardíaco: o que sabemos? Rev Port Cardiol. 2015;34:557.e1–557.e5.