Platypnea-orthodeoxia syndrome (POS) is an uncommon syndrome characterized by dyspnea and hypoxemia triggered by orthostatism and relieved by recumbency. It is often associated with an interatrial shunt through a patent foramen ovale (PFO). We report the case of a 92-year-old woman initially admitted in the setting of a traumatic femoral neck fracture (successfully treated with hip replacement surgery) in whom a reversible decline in transcutaneous oxygen saturation from 98% (in the supine position) to 84% (in the upright position) was noted early post-operatively. Thoracic multislice computed tomography excluded pulmonary embolism and severe parenchymal lung disease. The diagnosis of POS was confirmed by tilt-table contrast transesophageal echocardiography, which demonstrated a dynamic and position-dependent right-to-left shunt (torrential when semi-upright and minimal in the supine position) through a PFO. The patient underwent percutaneous closure of the PFO with an Amplatzer device, which led to prompt symptom relief and full functional recovery.
A síndrome platipneia-ortodeoxia (SPO) é uma entidade rara caracterizada por dispneia e hipoxemia desencadeadas pelo ortostatismo e aliviadas pelo decúbito. Está frequentemente associada à presença de um shunt inter-auricular através de um foramen ovale patente (FOP). Relata-se o caso de uma mulher de 92 anos, internada inicialmente por fratura traumática do colo do fémur. Foi submetida a artroplastia da anca sem complicações. No período pós operatório inicial observou-se um declínio reversível da saturação de oxigênio de 98% em decúbito dorsal para 84% na posição ortostática. A angio-tomografia computorizada do tórax excluiu trombo-embolia pulmonar e doença grave do parênquima pulmonar. O diagnóstico de SPO foi confirmado por ecocardiografia transesofágica contrastada (soro agitado) com inclinação na mesa de tilt, que demonstrou um shunt direito-esquerdo dinâmico e posicional (torrencial a 45° e mínimo a 0°) através de um FOP. A doente foi submetida a encerramento percutâneo do FOP com dispositivo Amplatzer, que proporcionou alívio sintomático imediato e permitiu uma recuperação funcional total.
Platypnea-orthodeoxia syndrome (POS) is characterized by dyspnea and hypoxemia induced by orthostatism and relieved by the supine position.1 It is a rare but probably underestimated cause of dyspnea that results from the postural accentuation of an intracardiac or pulmonary right-to-left shunt, leading to arterial oxygen desaturation. The most common etiologic association is an interatrial right-to-left shunt through a patent foramen ovale (PFO) or an atrial septal defect.3 Although a right-to-left pressure gradient usually drives the shunt, it can occur in the absence of an elevated right atrial pressure.2,4 In the latter cases, embryonic remnants (such as a prominent persistent Eustachian valve or a Chiari network)5,6 or acquired anatomical features (like pulmonary resection, aortic aneurysm, aortic elongation, pericardial effusion, constrictive pericarditis and kyphoscoliosis3,7) can both direct the flow from the inferior vena cava through the fossa ovalis and distort the normal atrial and septal arrangement. Individually or in association, these can create a specific anatomical and functional condition leading to a right-to-left shunt boosted by orthostatism. Although the ultimate underlying mechanisms are unknown, one possibility is that the upright position might stretch the interatrial defect, allowing streaming of systemic venous blood into the left atrium. The treatment of choice is percutaneous closure of the interatrial communication.8
Case reportA 92-year-old woman was admitted to hospital with a left femoral neck fracture caused by a non-syncopal fall at home.
Relevant medical history included hypertension, dyslipidemia, two previous strokes (at the ages of 75 and 82 years) without significant residual motor or cognitive deficits, osteoporosis and severe kyphoscoliosis. She was on treatment with aspirin, simvastatin and losartan. Within the year prior to the admission the patient's family had noticed a progressive functional decline, with undue fatigue and dyspnea for progressively smaller efforts, which were partially relieved by stooping and squatting.
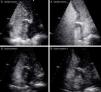
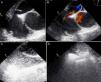
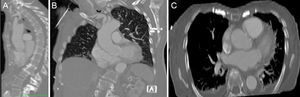
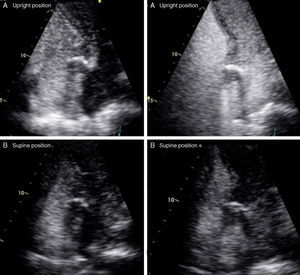
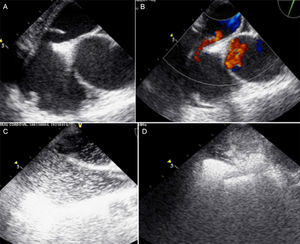
Following admission, hip replacement surgery was undertaken on day 3 of hospital stay, with no relevant complications. During routine early post-surgical observation in the intensive care unit, she was found to be hypoxic when sitting for the first time after the intervention. Physical examination was unremarkable, but interestingly the observed breathlessness and desaturation improved after lying flat and were reproducible on subsequent mobilizations. Blood chemistry, coagulation panel and blood cell count were normal. NT-proBNP level was within the age-adjusted normal range (326 pg/dl). Blood gas analysis, taken in the upright position, showed normal pH and PaCO2 (7.41 and 42 mmHg, respectively) and reduced PaO2 (42 mmHg). The chest X-ray revealed a tortuous proximal aorta with clear lung fields. Given the clinical setting, a contrast-enhanced chest computed tomography scan was performed, which excluded both pulmonary embolism and parenchymal lung disease as potential causes. However, severe kyphosis, aortic elongation and a grossly distorted relationship of the aortic root and proximal ascending aorta with the right atrium were noticed (Figure 1). A transthoracic echocardiogram showed normal left and right ventricular systolic function and chamber dimensions, mild left ventricular diastolic dysfunction, normal sized atria, no significant valve disease and no signs of pulmonary hypertension (pulmonary artery systolic pressure of 32 mmHg). A bubble contrast study revealed a mild right-to-left atrial shunt in the supine position without Valsalva maneuver, which increased significantly when sitting (Figure 2). In order to further assess the relationship between body position and the intensity of the shunt, a tilt-table assisted transesophageal echocardiogram was subsequently performed. While the patient was lying flat, the interatrial septum was redundant and tended to bow towards the left atrium; a small separation of the septum primum and septum secundum was seen, increasing significantly to 4 mm at 45°, unmasking a large shunt by color Doppler flow (Figure 3). There was no evidence of embryonic remnants, including a prominent persistent Eustachian valve or a Chiari network. The contrast study confirmed a minimal right-to-left shunt through the PFO while lying flat, which became significantly larger in the semi-upright position (Figure 3). During the tilt-table assisted echocardiographic imaging, right and left atrial pressures were studied. Central venous pressure was measured directly in the right atrium through an indwelling jugular catheter, while left atrial pressure was estimated indirectly using the Nagueh formula9 (taking into account mitral flow velocity by pulsed Doppler and myocardial tissue velocity at the level of the lateral mitral annulus by tissue Doppler imaging on transthoracic echocardiography). A positive right-to-left pressure gradient of 7 mmHg became evident at 45°.
Based on the echocardiographic findings and the 30% decline in arterial partial pressure of oxygen and oxygen saturation in the supine position, a diagnosis of PFO-related POS was established.
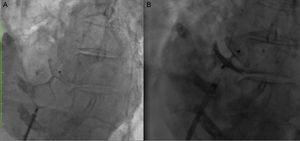
Subsequently, the patient underwent percutaneous closure of the PFO with a 25 mm Amplatzer® cribriform occluder device (Figure 4). The procedure was uneventful, with no evidence of residual right-to-left shunt at the final angiogram. Clinical follow-up has been favorable, with the patient free from breathlessness and desaturation episodes, thus enabling a full functional recovery from hip surgery.
DiscussionTo our knowledge, this is the oldest patient ever reported in the medical literature diagnosed with PFO-related POS successfully treated by percutaneous closure, with a subsequent full functional recovery from orthopedic surgery, making this case unique.2
POS is an uncommon cause of dyspnea that requires a very high index of suspicion to be recognized; for this reason, it is probably underdiagnosed and its prevalence is likely to be underestimated. It can be associated with cardiac, pulmonary and liver disease,10 but the most common cause is an intracardiac right-to-left shunt, caused by some type of interatrial communication, that is enhanced by orthostatism.3 Typically patients have normal pulmonary artery pressure.2
At least two factors must coexist to cause this syndrome: first the presence of an anatomical bypass to the pulmonary circulation, which in the present case was a PFO; second, one or more dynamic factors with a functional impact on intracardiac blood flow patterns – in this case kyphosis and aortic elongation – that can cause or increase the right-to-left shunt in the upright position.
According to case series and anecdotal reports in the literature, most patients are over 60 years old by the time a diagnosis of POS is established.2,4,11–13 The most common anatomical interatrial communication is a PFO, followed by true atrial septal defect and fenestrated atrial septal aneurysm.3 Contributing factors that have been identified as implicated in the pathogenesis of this condition are pneumectomy, right lower or mid lobe resection, aortic dilatation/elongation, localized or circumferential pericardial effusion, constrictive pericarditis, skeletal deformity (kyphosis, scoliosis) and right diaphragmatic paralysis.3,7,13 In the majority of cases with a PFO, POS was considered to be the first manifestation of a previously clinically silent PFO that became apparent as a consequence of one or more of the aforementioned conditions, most of which are age-related. Several anatomic and functional changes that occur with aging can create the hemodynamic conditions that facilitate right-to-left shunting through a PFO.7 Progressive increase in PFO size may favor a larger shunt,14 while increased right ventricular stiffness will increase filling and right atrial pressures; aortic dilatation and elongation7 and thinning of intervertebral discs and vertebral bodies (by accentuating kyphosis)15 can lead to atrial chamber and/or septal deformation, potentially changing the anatomical relationship between the atrial septum and the inferior vena cava and creating a dynamic right-to-left pressure gradient, that may ultimately be related to respiratory and vascular movements.
In the present case, symptoms arose several months before the diagnosis, and a causal relationship to the trauma that determined the initial hospital admission cannot be definitely ruled out. We consider that the effect of an elongated aortic root lying on the top of the right atrium and compressing the chamber and stretching the septum (Figure 1), and severe kyphosis modifying thoracic architecture and thus facilitating abnormal anatomical relationships between intrathoracic structures, are likely to have been contributing or precipitating factors.
Contrast transthoracic echocardiography is the most useful tool for screening right-to-left shunts, in view of its widespread availability, low cost, safety and sensitivity.2 On the other hand, transesophageal echocardiography on the tilt table is better suited for assessing atrial, septal, inferior vena cava and aortic anatomy, as well as the dynamic interactions between these structures and their positional dependency.2 In parallel with imaging, serial positional oxygen measurements should be taken to estimate shunt magnitude. Cardiac catheterization with direct measurement of oxygen saturation in the left atrium and pulmonary veins remains the gold standard for the diagnosis of POS related to intracardiac shunting. However, in daily practice, non-invasive workup is usually sufficient.2
The definitive treatment for platypnea-orthodeoxia syndrome related to atrial shunting is closure of the atrial defect.8 The decision to treat should be guided by patient disability rather than shunt magnitude. Percutaneous closure has shown to be effective in patients of all ages,8 avoiding the mortality, morbidity and costs associated with open-heart surgery.
ConclusionsPOS is an uncommon and multifaceted phenomenon that should be suspected in the presence of unexplained positional hypoxemia.
Contrast transthoracic echocardiography is a useful screening test when POS is suspected, and the diagnosis can be safely and definitely established by tilt-table transesophageal echocardiography.
Percutaneous closure of a PFO is safe and effective even in nonagenarians with this condition.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.