Isolated left ventricular non-compaction is a rare disease classified as a primary genetic cardiomyopathy and is characterized by heart failure, systemic embolism and ventricular arrhythmias. The diagnosis is established by Doppler echocardiography. We report the case of an asymptomatic young adult, with no history of heart disease, who underwent preoperative assessment for low-risk orthopedic surgery. The electrocardiogram showed left bundle branch block, which prompted further investigation with Doppler echocardiography, cardiac computed tomography angiography and cardiac magnetic resonance imaging. A diagnosis of isolated left ventricular non-compaction and pulmonary embolism was made. Some aspects of preoperative assessment in low-risk surgical patients are discussed.
A cardiomiopatia não compactada isolada do ventrículo é uma doença rara, classificada como uma cardiomiopatia genética primária. A doença é caracterizada por insuficiência cardíaca, embolia sistémica e arritmias ventriculares. O diagnóstico é estabelecido pelo ecodopplercardiograma. Relata-se o caso de adulto jovem assintomático, sem história prévia de cardiopatia, que realizou avaliação pré-operatória para cirurgia ortopédica de baixo risco. Eletrocardiograma apresentou bloqueio do ramo esquerdo, que suscitou investigação complementar com ecodopplercardiograma, angiotomografia do tórax e ressonância cardíaca. Concluiu-se pelo diagnóstico de cardiopatia não compactada isolada do ventrículo e embolia pulmonar. Discutem-se aspetos da avaliação pré-operatória em pacientes de baixo risco cirúrgico.
Isolated left ventricular non-compaction (LVNC) was described for the first time by Chin et al. in 1990.1 It is a rare disease classified as a primary genetic cardiomyopathy by the American Heart Association.2 LVNC is attributed to intrauterine arrest of compaction of the meshwork of the fetal myocardium.3
The prevalence of LVNC in the general population is unknown. Existing information is mainly derived from patients undergoing Doppler echocardiography. A Swiss review identified 34 cases, corresponding to 0.014% of all echocardiograms performed over a period of 15 years.4 The prevalence of LVNC in patients with heart failure (HF) has been estimated as 3–4%.5 It appears to affect predominantly males, as shown in the four main series on LVNC patients.1,4,6,7
A family history of LVNC is described in 12–50% of case reports.8 Autosomal dominant inheritance is more common than X-linked or autosomal recessive inheritance.9 There is growing recognition of a considerable overlap in the genetic loci involved in the pathogenesis of the main cardiomyopathies. Phenotypic expression of different cardiomyopathies may be found in the same patient, including LVNC and hypertrophic cardiomyopathy,10 although LVNC is more commonly associated with congenital heart disease and Wolff-Parkinson-White syndrome.11
Preoperative assessment provides an opportunity for the physician to identify silent conditions and to optimize treatment of known cardiovascular disease. In recent years, in an attempt to avoid wasting resources on unnecessary medical exams, medical societies have established protocols for requests for preoperative exams. An editorial by the Cleveland Clinic,12 which is in agreement with the II Preoperative Guideline of the Brazilian Society of Cardiology (SBC),13 questions the value of the electrocardiogram (ECG) in preoperative assessment of asymptomatic individuals scheduled for low-risk surgery.
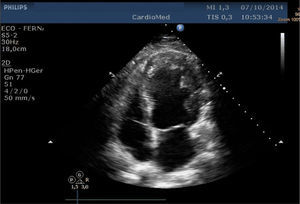
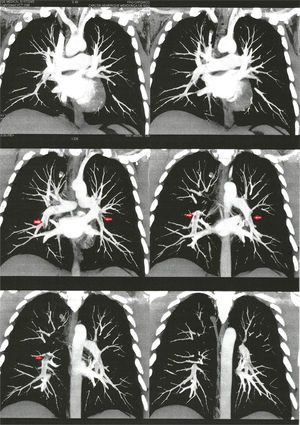
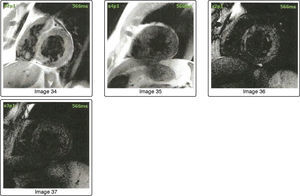
Case reportA 35-year-old man with partial rupture of the left Achilles tendon caused by a sports accident was referred by the surgeon for preoperative assessment. He had no cardiovascular symptoms or history of heart disease, was not taking prescription medication and did not smoke. Physical examination revealed blood pressure of 135/78 mmHg and heart rate of 89 bpm and no relevant alterations. He had a walking boot on his left leg. The chest X-ray was normal, and complete blood panel, blood glucose, plasma creatinine, urea and international normalized ratio were within reference values. The ECG showed complete left bundle branch block (LBBB). Tissue Doppler imaging (TDI) revealed left ventricular (LV) ejection fraction (LVEF) of 61%, left atrial volume index of 22 ml/m2, and LV mass index of 94.9 g/m2. Alterations in LV relaxation (E′=6 cm/s) and increased filling pressures (E/E′=16) were observed. TDI showed hypertrabeculation of the mid anterolateral wall and apical region (Figure 1). As the differential diagnosis of LVNC includes other forms of cardiomyopathy, the patient was referred for computed tomography coronary angiography, which showed signs of bilateral pulmonary embolism (Figure 2). D-dimers were 2310 ng/ml. Doppler echocardiography of the venous system of the left leg demonstrated hypoechogenic material in the popliteal and posterior tibial veins, partially obstructing the lumen. Cardiac magnetic resonance imaging (Figure 3) showed LV hypertrophy and marked mid-apical subendocardial trabeculation (estimated at 22% of total myocardial mass), myocardial late enhancement indicative of mid anteroseptal and basal mid inferoseptal myocardial fibrosis, and moderate global LV dysfunction, with LVEF estimated at 38%, confirming the diagnosis of LVNC.
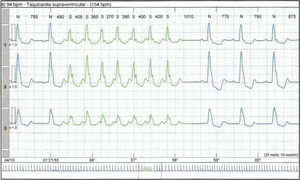
Outpatient Holter 24-hour electrocardiographic monitoring showed an episode of paroxysmal supraventricular tachycardia and ventricular extrasystoles (Figure 4), but the patient remained asymptomatic.
DiscussionLVNC is a rare disease characterized by excessive trabeculation of the LV wall and intratrabecular recesses communicating with the LV chamber. In most cases it is diagnosed in infancy, but symptoms may not appear until adulthood. Its incidence is estimated at 0.05% in the adult population.2
LVNC is usually associated with other congenital heart disease such as atrial and septal defects. Isolated LVNC (in the absence of other congenital defects) is even rarer.14
The diagnostic criteria proposed by Jenni et al.15 are designed to distinguish isolated LVNC from other forms of LV hypertrophy. The criteria are (1) at least four prominent trabecula and deep intertrabecular recesses; (2) blood flow in the recesses demonstrable with color Doppler; (3) the non-compacted segments mainly involve the apex and the inferior and mid portions of the LV wall; (4) the non-compacted segments typically have a two-layer structure with a ratio between the subendocardial non-compacted layer and the subepicardial compacted layer of >2:1; (5) coexisting cardiac abnormalities are absent.15
Diagnosis of LVNC in adults is challenging due to its similarity to more common conditions such as dilated hypertensive heart disease, infiltrative cardiomyopathy, apical hypertrophic cardiomyopathy and endomyocardial eosinophilic disease. Early diagnosis is important because of the high risk of HF, fatal ventricular arrhythmias and embolism.6
Prognosis is poor and the treatment for end-stage HF is cardiac transplantation. Life-threatening ventricular arrhythmias are an indication for an implantable cardioverter-defibrillator. The main mechanisms of death in LVNC are sudden death and refractory HF.16
The patient presented here, although asymptomatic, was classified as having stage B HF according to the American College of Cardiology/American Heart Association guidelines,17 as he presented structural and functional alterations, including systolic dysfunction. Such patients are at high risk of developing symptomatic HF and so prompt treatment is indicated.17
The pulmonary embolism diagnosed in our patient appears to have been due to immobilization of the left leg and unrelated to LVNC, which increases risk for arterial thromboembolism and hence stroke.18
Cardiologists are routinely called upon to assess patients’ preoperative risk. The aim is to identify undiagnosed conditions that could increase risk for perioperative morbidity and mortality and to suggest ways to reduce the risk.19,20 Assessment is always multifactorial and risk factors for postoperative cardiac events include the type of procedure and factors specific to the patient.21 Routine ECG assessment is not recommended for patients at low cardiac risk about to undergo low-risk surgery, since it could delay the operation unnecessarily, increase costs and increase patient anxiety.12 Some guidelines do suggest a preoperative ECG, but such recommendations are generally based on low-level evidence and the opinion of specialists.22
The SBC recommends preoperative ECG in selected cases, but considers routine ECG a class III recommendation, level of evidence C, for asymptomatic individuals undergoing low-risk surgery.13
In the case presented, the ECG requested by the surgeon showed complete LBBB, and since LBBB has prognostic significance even in asymptomatic individuals, or those without known heart disease,23 it was decided to perform TDI, which led to a diagnosis of LVNC.
ConclusionThe ECG is a low-cost and accessible tool for identifying myocardial disease and arrhythmias. A routine ECG in preoperative assessment may help identify conditions that, although asymptomatic, could increase perioperative risk. In the case presented the early diagnosis of LVNC, a condition that can lead to HF, thromboembolic events, ventricular tachyarrhythmias and death, enabled the patient to receive a better quality of care. The recommendation in the SBC guidelines not to perform ECG routinely in preoperative assessment is based on the opinion of specialists, and the question should be settled definitively by means of methodologically robust studies.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThere was no external funding for this article.
Academic linksThis article is part of the heart failure research component of the Post-Graduate Course in Cardiovascular Science at Universidade Federal Fluminense.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Antonio José AJ, do Couto AA, Mesquita ET, Ribeiro ML, de Souza Junior CV, de Andrade Martins W. Duas surpresas potencialmente fatais em avaliação pré-operatória de adulto jovem assintomático. Rev Port Cardiol. 2016;35:309.e1–309.e6.