There are few published data on mortality in anterior ST-segment elevation myocardial infarction (STEMI) in Portugal, particularly in centers with direct access to primary angioplasty. We present the experience of a center with direct access to primary angioplasty in the management of patients admitted with anterior STEMI.
MethodsWe performed a retrospective study of 120 patients admitted with anterior STEMI in 2008 to Faro Hospital (Algarve region, Portugal).
ResultsSignificant coronary artery stenosis was found in 99 patients (82.5%). These patients were predominantly male (79%), and had a mean age of 63 years. Primary angioplasty was performed in the majority of patients within 6hours of symptom onset and median ECG-to-balloon time was 89 minutes. Primary angioplasty was successful in 98% of patients and complete revascularization was achieved in 83%. Radial access was used in 82% of cases. In-hospital and 30-day mortality was 3%.
ConclusionDirect access to primary angioplasty was associated with low mortality in patients admitted with anterior STEMI.
Existem muito poucos dados em Portugal sobre a mortalidade do enfarte agudo do miocárdio com supradesnivelamento do segmento ST (EAMCST) anterior, particularmente em centros com via verde coronária (VVC) e angioplastia primária. O objetivo deste estudo é apresentar os resultados de um centro com VVC e angioplastia primária no tratamento de doentes internados por EAMCST anterior.
MétodosEstudo retrospetivo dos 120 doentes admitidos por EAMCST de localização anterior no ano de 2008 no centro hospitalar de Faro.
ResultadosFoi encontrada doença coronária significativa em 99 doentes (82,5%). Estes doentes eram predominantemente do sexo masculino (79%) e tinham uma idade média de 63 anos. A angioplastia primária foi realizada na maioria dos doentes nas primeiras 6 h após o início dos sintomas, sendo que a mediana do tempo ECG-balão foi de 89 min. A taxa de sucesso da angioplastia primária foi de 98%, sendo que a revascularização foi completa em 83% dos casos. O cateterismo cardíaco foi realizado por via radial em 82% dos doentes. A taxa de mortalidade intra-hospitalar e aos 30 dias foi de 3%.
ConclusãoA implementação da VVC com acesso direto a angioplastia primária associou-se a uma baixa taxa de mortalidade dos doentes admitidos por EAMCST anterior.
Primary angioplasty has been shown to be superior to fibrinolytic therapy in ST-elevation myocardial infarction (STEMI) and is indicated as first-line treatment in the guidelines.1,2
The shorter the time interval between symptom onset (or first medical contact) and angioplasty, the greater its benefit. In order to minimize this interval, a coronary fast-track system (Via Verde Coronária) has been established in the Algarve region of Portugal to provide rapid and efficient transport between the pre-hospital setting and a hospital able to perform primary angioplasty or to transfer a patient from one hospital to another with the necessary facilities. The time from first medical contact to primary angioplasty (medical contact-to-balloon time) should be less than 120 minutes, except in patients presenting with extensive infarction within two hours of symptom onset and with a low bleeding risk, when it should be less than 90 minutes.1
The Portuguese region of the Algarve has a resident population of around 500000, which can increase threefold due to tourism, especially in the summer. Faro Hospital is the only hospital in the region able to provide 24-hour primary angioplasty, and has a coronary care unit (CCU) with the logistic and technical facilities to treat STEMI patients. It is part of a referral network, the coronary fast-track system, which is designed to ensure that all STEMI patients originating from the National Institute for Medical Emergencies (INEM) system or health centers, basic emergency departments or Hospital do Barlavento Algarvio (which does not have primary angioplasty capability) are transferred immediately to Faro Hospital for primary angioplasty.
INEM, basic emergency departments and Hospital do Barlavento Algarvio have 24-hour facilities to perform 12-lead ECG and transmit the data to the CCU in Faro Hospital; the coronary fast-track system is activated by a telephone call from the cardiologist on duty.
The coronary fast-track system began operating in the Algarve in 2002, since when it has been the means of referral for a growing number of STEMI patients. Primary angioplasty has been available in Faro Hospital since 2003 and a large number of procedures are performed every year.
With the exception of the Algarve region, fewer than 6% of STEMI patients in Portugal treated by primary angioplasty are referred directly by local fast-track systems.
In patients with anterior STEMI it is particularly important to select and implement the appropriate treatment as rapidly as possible in order to reduce their high mortality. Figures in the literature vary, but 30-day mortality is over 6%.4–6 In Portugal no outcome data have been published for anterior STEMI in centers with primary angioplasty facilities linked to a coronary fast-track system.
The aim of this study was to analyze and present the results of a center with direct access to primary angioplasty and with several years’ experience of a coronary fast-track system in the management of patients admitted with anterior STEMI in 2008.
MethodsStudy populationThe study included 120 patients admitted with anterior STEMI to Faro Hospital in 2008.
The diagnosis of anterior STEMI was based on 12-lead ECG, using the criteria of ST-segment elevation ≥0.1mV in DI and aVL or ≥0.2mV in two or more contiguous precordial leads from V1 to V5. All patients who met the ECG criteria and presented sustained chest pain of less than 12 hours’ duration were included. The diagnosis of anterior STEMI was established by a physician from INEM, a health center, basic emergency departments, the Emergency Department of Hospital do Barlavento Algarvio or the Emergency Department of Faro Hospital.
Coronary fast-track system and treatment protocolThe coronary fast-track system functions as follows:
- -
Patients who used the national medical emergency number (112) and whose diagnosis was established by an INEM physician were transported directly to the catheterization and interventional cardiology laboratory (LHCI) of Faro Hospital, the CCU physician having been contacted by telephone.
- -
Patients who went to health centers, basic emergency departments, or the Emergency Department of Hospital do Barlavento Algarvio underwent ECG, which was transmitted via the Lifenet system to the CCU in Faro Hospital; telephone contact was immediately established between the receiving institution and the cardiologist on duty at the CCU, and transfer of the patient to the LHCI, accompanied by a physician from INEM or the receiving institution, was arranged.
- -
Patients who went directly to the Emergency Department of Faro Hospital were immediately transferred under medical supervision to the LHCI (or to the CCU while awaiting access to the LHCI) after contact between the emergency department physician and the cardiologist on duty at the CCU. These patients were not considered to have been admitted via the fast-track system.
- -
Irrespective of how the fast-track system was activated, the cardiologist on duty at the CCU immediately contacted the catheterization team to ensure that they would be available when the patient arrived in the department.
During transfer of patients to the LHCI, 250mg of aspirin and oxygen therapy were administered. Clopidogrel was not usually administered, but depending on symptoms and in the absence of contraindications, opioids, metoclopramide, diazepam or nitrates could be given. Hemodynamically unstable patients were given fluids and inotropic agents at the discretion of the accompanying physician. Arrhythmias were treated in accordance with established practice with amiodarone or electrical cardioversion. Patients suffering cardiopulmonary arrest (CPA) were resuscitated in accordance with international guidelines.
Radial access was used by preference in the LHCI after administration of 5000U of unfractionated heparin. A single 20-mg bolus of eptifibatide was administered during the procedure. Stenting was used in most cases, the type of stent being at the discretion of the interventional cardiologist, who also decided whether intracoronary thrombus aspiration was required. Following the intervention, 600mg of clopidogrel was administered.
Patients were then transferred to the CCU and treated according to international guidelines for STEMI.1
After clinical stabilization, patients were transferred to the cardiology ward under continuous telemetric ECG monitoring until discharge. During hospitalization patients were enrolled in the Cardiology Department's cardiac rehabilitation program.
Data collection and processingData were collected retrospectively by consulting the LHCI database, the Cardiology Department's acute coronary syndromes database, and the medical support system of Faro Hospital. The medical records of individual patients were also consulted when necessary.
Demographic data, personal history, cardiovascular risk factors, clinical presentation, method of activation of the fast-track system, time intervals, type of access, results of coronary angiography and types of stent used were recorded.
The following time intervals were defined:
- -
Pain-to-diagnosis (from onset of pain to first ECG);
- -
Pain-to-balloon (from onset of pain to first balloon inflation);
- -
Diagnosis-to-balloon (from first ECG to first balloon inflation);
- -
Door-to-balloon (from arrival at Faro Hospital to first balloon inflation).
The TIMI risk score for STEMI was calculated for each patient to determine predicted mortality.
Patients were followed at 30 days through consultations or telephone interviews.
Statistical analysisSPSS version 13.0 was used for the statistical analysis. The Kolmogorov–Smirnov test was used to assess data normality, and the variables were analyzed accordingly. Descriptive variables are presented as median or mean±standard deviation as appropriate. Mortality was compared using Pearson's correlation coefficient, with a level of significance of p<0.05.
ResultsCharacteristics of the study populationDuring 2008, 120 patients were admitted to the Cardiology Department of Faro Hospital with a diagnosis of anterior STEMI. Of these, 21 (17.5%) did not present significant coronary stenosis, and the following data refer to the 99 patients who did have significant coronary disease.
Of these 99 patients, 79 were male and 20 female.
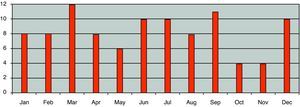
The mean number of patients with anterior STEMI admitted per month was eight, ranging between four in October and November and 12 in March (Figure 1).
Their mean age was 63±13 years (33–85); 29% were aged between 65 and 79 and 14% were aged ≥80.
Patients’ clinical histories are shown in Table 1.
Personal clinical histories and cardiovascular risk factors of patients with anterior STEMI.
| Personal history | No. of patients |
| Hypertension | 53 |
| Hypercholesterolemia | 49 |
| Diabetes | 23 |
| Smoking | 36 |
| Angina | 45 |
| MI | 16 |
| Coronary angioplasty | 16 |
| CABG | 2 |
| PVD | 3 |
| Stroke | 6 |
CABG: coronary artery bypass grafting; MI: myocardial infarction; PVD: peripheral vascular disease.
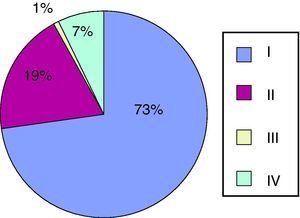
Six patients suffered CPA before hospital arrival requiring resuscitation maneuvers, and seven presented with cardiogenic shock (defined as systolic blood pressure <90mmHg and/or need for inotropic support), but most (71%) were in Killip class I at admission (Figure 2).
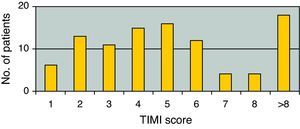
Most patients (55%) had a TIMI risk score for STEMI of >4 (Figure 3).
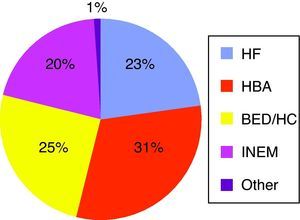
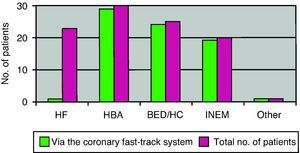
Patient originFigure 4 shows the origin of patients, the largest proportion coming from Hospital Barlavento Algarvio (31%) and basic emergency departments/health centers (25%).
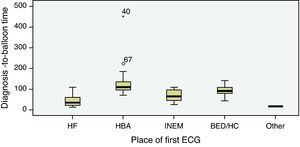
Time intervals following symptom onsetMedian pain-to-diagnosis time was 162 minutes (<3hours), median diagnosis-to-balloon time was 89 minutes and median door-to-balloon time was 15 minutes (Table 2).
Time intervals between symptom onset and treatment (presented as medians and interquartile range) of patients with anterior STEMI.
| Time interval (min) | Median (interquartile range) |
| Pain-to-balloon | 240 (180–360) |
| Pain-to-diagnosis | 162 (109–272) |
| Diagnosis-to-balloon | 89 (57–108) |
| Door-to-balloon | 15 (12–20) |
Most patients underwent primary angioplasty within six hours of symptom onset (36% within three hours and 46% between three and six hours).
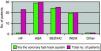
Diagnosis-to-balloon time was <120 minutes in 80% of patients but was longer in patients arriving via Hospital Barlavento Algarvio (Figure 5).
The coronary fast-track system was obviously not activated for patients who went directly to the Emergency Department of Faro Hospital. Of those who did not, the fast-track system was not activated in only three cases (4%) (Figure 6.)
Distribution of anterior STEMI patients according to origin (presented as absolute numbers of cases and numbers in which the fast-track system was activated). BED/HC: basic emergency departments/health centers; HBA: Hospital Barlavento Algarvio; HF: Emergency Department of Faro Hospital; INEM: Institute for Medical Emergencies.
Radial access was used in 82% of cases. Multivessel coronary disease was detected in 50% of patients. Complete revascularization was achieved in the initial procedure in 83% of cases. A mean of 2.1 stents were used, with drug-eluting stents being used in 81% of patients (Table 3).
Percentages of patients according to type of access, location of coronary lesions, complete revascularization in the initial procedure, and use of drug-eluting stents.
| Radial access | 82% |
| Femoral access | 18% |
| 1-vessel disease | 50% |
| 2-vessel disease | 35% |
| 3-vessel disease | 15% |
| Complete revascularization | 83% |
| Drug-eluting stent | 81% |
The failure rate of primary angioplasty was 2%.
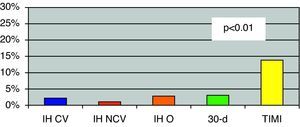
Mortality and reinfarctionDuring hospital stay there were two deaths from cardiovascular causes and one non-cardiovascular death (from septicemia secondary to acute cholecystitis). Overall mortality was thus 3% (Figure 7). The patients who died during hospital stay had a TIMI risk score for STEMI of ≥7.
Mortality in anterior STEMI patients. 30-d: 30-day mortality; IH CV: in-hospital cardiovascular mortality; IH NCV: in-hospital non-cardiovascular mortality; IH O: overall in-hospital mortality; TIMI: mortality predicted by the TIMI risk score for STEMI. p<0.01: statistical significance comparing observed 30-day mortality and that predicted by the TIMI risk score for STEMI.
No other deaths occurred during follow-up and thus 30-day mortality was 3%. The predicted mortality based on the TIMI risk score was 14%, considerably higher than observed (p<0.01) (Figure 7).
Mortality was higher in women (5% vs. 2.5%), although without statistical significance. In patients who presented with cardiogenic shock mortality was significantly higher (28.6%) (p<0.01), as it was in very elderly patients (aged ≥80) (p<0.01) (Table 4).
Radial access was associated with significantly lower mortality (1.2% vs. 11.1%, p=0.03), while complete revascularization did not increase mortality (2.4% vs. 5.9%, p=NS).
There were no instances of reinfarction during hospital stay.
DiscussionPrimary angioplasty is indicated as a priority in patients with STEMI and should be performed as early as possible. Fibrinolytic therapy has similar results to primary angioplasty when administered within 120 minutes of pain onset, but is associated with considerably higher risk of bleeding, particularly hemorrhagic stroke.7,8 Prompt transfer to a hospital with facilities for primary angioplasty avoids exposing patients to the risk of fibrinolysis, which should only be considered when there is no possibility of primary angioplasty within 120 minutes. According to the American and European guidelines, the interval between diagnosis and balloon angioplasty should not exceed 120 minutes and ideally should be less than 90 minutes.1–3
However, the first relevant time interval – between symptom onset and first medical contact – basically depends on the patient. In our study, the median pain-to-diagnosis time of 162 minutes is longer than reported in the registries presented by Flesch et al. (Cologne)10 and Le May et al.,11 which highlights the need for public education programs to encourage earlier use of the medical emergency telephone number.
The benefit of a coronary fast-track system is mainly a function of its ability to transfer patients diagnosed with STEMI to a hospital with facilities for primary angioplasty. Analysis of the graph showing diagnosis-to-balloon times according to patient origin (Figure 5) reveals that the longest time was for patients from Hospital Barlavento Algarvio, which can be explained by its distance from Faro Hospital (over 60km) and the fact that INEM does not transfer patients between hospitals. However, this problem is mitigated by the round-the-clock availability of an on-site ambulance and team prepared for immediate interhospital transfer. Although they could be improved, our diagnosis-to-balloon times were shorter than those reported in other registries of urban areas with several hospitals with facilities for primary angioplasty.10,11 The fact that 80% of patients were treated within the time limits recommended in the guidelines shows that it is possible to develop an efficient system to transfer patients for primary angioplasty.
Our door-to-balloon times were also shorter than those in other studies and registries,10–12 proof of the excellent organization of the LHCI and the technical skills of the angioplasty team, in which the experience of the interventional cardiologist (who performs around 200 primary angioplasties a year) is a key factor.
The rate of activation of the fast-track system was high (74% of all anterior STEMI patients), which reflects the continuing improvements to the system over the several years it has been operating. The fact that 23% of patients still went directly to the Emergency Department of Faro Hospital may indicate that further campaigns to raise public awareness are required.
The distribution of patients over the course of the year was relatively constant, with a slight increase in the months when more tourists come to the Algarve (summer, Easter and New Year). The characteristics of the study population are similar to those found in other studies;10,11 the high percentage of elderly patients (43% aged over 65), the number who suffered CPA (seven) and the number presenting with cardiogenic shock (six) should be noted. A TIMI risk score of ≥4 in 55% of patients is a clear indication of the high risk of patients with anterior STEMI.13 This percentage is higher than found in other studies, which may be related to the fact that the analysis focused solely on anterior STEMI.10,11
A radial approach was used in a higher percentage (82% of the study population) than reported in other registries, even in those of highly experienced centers such as in Ruzsa et al.14 Radial access is generally considered to be better for angioplasty due to the lower rate of bleeding complications.15 It has, however, frequently been pointed out that it should only be used in centers with considerable experience in angiography and elective angioplasty using this approach, so as to avoid delays in revascularizing patients with STEMI. The LHCI at Faro Hospital has performed a large number of procedures using radial access and thus conforms to this recommendation. The fact that the median time from arrival at the LHCI to first balloon inflation was 15 minutes is clear evidence of the center's efficiency in this technique.
Another interesting finding was that despite the competence of those interpreting the ECGs, 20% of patients did not present significant coronary stenosis on angiography. This figure is higher than found in other registries analyzing coronary fast-track systems.9
The presence of multivessel disease in half of the patients is not unexpected given the characteristics of the study population. There is still disagreement concerning whether to perform complete revascularization in such patients, although some studies have shown that it is safe in primary angioplasty.16 In our study the interventional cardiologist opted for complete revascularization in 83% of cases, and no complications occurred in the short term, which appears to confirm its safety.
Drug-eluting stents were used in most patients. Randomized trials on these stents have shown their non-inferiority compared to bare-metal stents in primary angioplasty.17 There is even more reason to use drug-eluting stents in anterior STEMI due to the large area of myocardium affected.
Mortality in this study, both in-hospital and at 30 days (3%), was lower than reported in the literature for anterior STEMI4–6 and significantly lower than predicted by the TIMI risk score (14%).
A limitation of the study is that it was not designed to determine the underlying causes of this lower mortality, although the authors consider that it may be related to various factors, including:
- -
the pre-hospital emergency network, which enables rapid and efficient transport of STEMI patients via the coronary fast-track system accompanied by medical staff trained to provide advance life support;
- -
the high rate of activation of the coronary fast-track system;
- -
optimized organization of the LHCI;
- -
quality of care in the CCU;
- -
quality of care in the cardiology ward, with continuous telemetric monitoring and enrolment in cardiac rehabilitation programs.
The factors associated with the observed mortality were cardiogenic shock and age over 80, as found in other studies and registries.10,11
ConclusionDirect access to primary angioplasty was associated with low mortality in patients admitted with anterior STEMI.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Marques N, et al. Impacto da Via Verde Coronária e da Angioplastia Primária na redução da mortalidade associada ao enfarte com elevação do segmento ST anterior. A experiência Algarvia. Rev Port Cardiol. 2012. http://dx.doi.org/10.1016/j.repc.2012.07.005.