Takotsubo syndrome (TTS) is characterized by transient left ventricular (LV) systolic dysfunction.
AimTo characterize a Portuguese population with TTS and to determine their short- and medium-term prognosis.
MethodsWe conducted a multicenter study in Portuguese hospitals that included all patients diagnosed with TTS, initially retrospectively and subsequently prospectively. Short- and medium-term clinical complications and mortality were assessed. Independent predictors of in-hospital complications and prognostic factors were determined.
ResultsA total of 234 patients (210 female, age 68±12 years) were included. During hospitalization, 32.9% of patients had complications: acute heart failure (24.4%), atrial fibrillation (9.0%), ventricular arrhythmias (2.6%), complete atrioventricular block (2.1%), stroke/transient ischemic attack (1.7%), and LV thrombus (1.3%).
Chronic kidney disease (CKD) (p=0.02), coronary artery disease (CAD) (p=0.027), lower LV ejection fraction (LVEF) on admission (p=0.003), and dyspnea at presentation (p=0.019) were predictors of in-hospital complications. In-hospital mortality was 2.2%. At the mean follow-up of 33±33 months, all-cause mortality was 4.4%, cardiovascular mortality was 0.9% and TTS recurrence was 4.4%. Prolonged QTc interval on admission was associated with complications in follow-up (p=0.001).
ConclusionTTS has a good short- and medium-term prognosis. However, the rate of in-hospital complications is high and should not be overlooked. Dyspnea at presentation, CKD, CAD and lower LVEF on admission were independent predictors of in-hospital complications. Prolonged QTc on admission was associated with complications in follow-up.
A síndrome de Takotsubo (TTS) caracteriza-se por disfunção sistólica ventricular esquerda transitória.
ObjetivoCaracterizar uma população portuguesa com TTS e determinar o seu prognóstico a curto e médio prazo.
MétodosEstudo multicêntrico português com inclusão retrospetiva e prospetiva de todos os doentes diagnosticados com TTS. Foram avaliadas as complicações clínicas e a mortalidade a curto e médio prazo. Determinaram-se os preditores independentes de complicações intra-hospitalares e os fatores associados ao prognóstico.
ResultadosForam incluídos 234 doentes (210 mulheres, 68±12 anos). Durante o internamento, 32,9% dos doentes apresentaram complicações clínicas: insuficiência cardíaca (24,4%), fibrilhação auricular (9,0%), arritmias ventriculares (2,6%), bloqueio auriculoventricular completo (2,1%), acidente vascular cerebral/acidente isquémico transitório (1,7%) e trombo no ventrículo esquerdo (1,3%). Doença renal crónica (DRC) (p=0,02), apresentação com dispneia (p=0,019), presença de doença arterial coronária (DAC) (p=0,027) e menor fração de ejeção ventricular esquerda (FEVE) na admissão (p=0,003) foram preditores independentes de complicações intra-hospitalares. A taxa de mortalidade intra-hospitalar foi de 2,2%. No follow-up médio de 33± 33 meses, a taxa de mortalidade global foi de 4,4%, 0,9% de causa cardíaca. A taxa de recorrência de TTS foi 4,4%. O prolongamento do intervalo QTc na admissão associou-se a complicações clínicas no follow-up (p=0,001).
ConclusãoA TTS tem bom prognóstico a curto e a médio prazo. Contudo, a taxa de complicações intra-hospitalares é elevada e não deve ser menosprezada. A DRC, apresentação como dispneia, DAC concomitante e menor FEVE na admissão são preditores de complicações intra-hospitalares. O prolongamento do intervalo QTc na admissão associou-se a complicações no follow-up.
Takotsubo syndrome (TTS) was first described in the Japanese population in the early 1990s. It takes its name from the Japanese octopus trap named takotsubo because the left ventricle in systole takes a similar shape to the trap.1
The syndrome is characterized by transient left ventricular (LV) systolic dysfunction, electrocardiographic changes that mimic acute myocardial infarction and minimal release of myocardial necrosis enzymes, in the absence of obstructive coronary artery disease (CAD).2 It has been estimated to account for 1-2% of cases of suspected acute coronary syndrome (ACS).3 However, this figure is probably an underestimate.4
In other series, 90% of patients were female and aged over 50 years. In about two-thirds of cases, there was an emotional or physical triggering factor.2
The underlying mechanism of TTS is not fully understood. However, the most commonly accepted theory is of catecholamine-induced cardiotoxicity in response to an emotional or physical stimulus.5
Clinical presentation is very similar to an ACS, and TTS needs a differential workup to distinguish between the two entities. To establish a diagnosis of TTS, coronary angiography is needed to exclude obstructive CAD as the cause of LV dysfunction.4
The most commonly used diagnostic criteria for TTS are those proposed by the Mayo Clinic.7 The Heart Failure Association of the European Society of Cardiology recently published updated diagnostic criteria4 that distinguish between primary and secondary TTS. In the primary subtype, cardiac symptoms are the primary reason for seeking medical care, while in the secondary subtype the patient has an underlying primary disease that precipitated TTS.
Therapy is supportive, usually consisting of vasodilators, beta-blockers and diuretics.8
Although the syndrome has previously been described as benign, more recent series have revealed a significant rate of in-hospital complications, and the short- and medium-term prognosis may be less favorable than previously described.6
The aim of this study was to characterize a Portuguese population with TTS and to determine their short- and medium-term prognosis.
MethodsPatient populationIn this observational multicenter study involving 12 Portuguese hospitals, all patients diagnosed with TTS from 2002 to 2016 were included, retrospectively until 2012 and prospectively since 2012.
Patients were selected according to the Mayo Clinic diagnostic criteria: transient abnormality in LV wall motion beyond a single epicardial coronary artery perfusion territory; absence of obstructive CAD or angiographic evidence of acute plaque rupture; new electrocardiographic abnormalities or modest elevation in cardiac troponin levels; and the absence of pheochromocytoma or myocarditis.7
An exception to these criteria was the inclusion of patients who died during the acute phase, prior to complete recovery of myocardial function.
Data collectionThe data were collected by consulting the clinical records of patients diagnosed with TTS, retrospectively before 2012 and prospectively after 2012.
Demographic data, personal history, cardiovascular risk factors, triggering factors, clinical presentation, electrocardiographic findings, coronary angiography findings and complications during hospitalization were collected. Coronary angiography was performed in all patients.
TTS was classified as apical, midventricular, basal or focal according to the LV ballooning pattern on the transthoracic echocardiogram.6
Chronic kidney disease (CKD) was defined as glomerular filtration rate <60 ml/min for at least three months.9
QT interval was measured by each patient's cardiologist. Corrected QT interval (QTc) was calculated using Bazett's formula and was defined as prolonged if >450 ms for males and >470 ms for females.10
Transthoracic echocardiography was performed on admission, at discharge and during follow-up. Complete echocardiographic recovery was defined as the normalization of regional wall motion abnormalities present on the initial transthoracic echocardiogram.
The in-hospital complications included were acute heart failure, cardiogenic shock, new-onset atrial fibrillation (AF), ventricular fibrillation/ventricular tachycardia, complete atrioventricular block, stroke/transient ischemic attack (TIA), LV thrombus and death from any cause.
Acute heart failure was defined as the presence of dyspnea, pulmonary edema and/or oxygen desaturation requiring drug therapy and/or mechanical support.
Cardiogenic shock was defined as systolic blood pressure <90 mmHg with signs of tissue hypoperfusion requiring inotropic agents and/or fluid therapy.
Follow-up data were obtained from clinical visits, medical records and telephone interviews.
The follow-up analysis included all-cause mortality, cardiovascular mortality and major cardiovascular events (stroke/TIA, myocardial infarction and recurrence of TTS).
Cardiovascular mortality was defined as death caused by heart failure, arrhythmia, myocardial infarction, cerebrovascular disease, pulmonary embolism or sudden cardiac death. Any death not covered by these definitions was defined as non-cardiovascular mortality.
Myocardial infarction was defined using the criteria of the third universal definition of myocardial infarction.11
Statistical analysisA descriptive analysis was carried out to characterize the sample profile. Continuous variables are presented as means and standard deviation and categorical variables are presented as percentages.
The chi-square test was used to analyze associations between categorical variables, and the Student's, Mann-Whitney and Kruskal-Wallis tests were applied to continuous variables. The Kolmogorov-Smirnov test was used to verify normality of distribution.
Binary logistic regression was used to measure predictors of in-hospital and follow-up events.
A p-value <0.05 (significance level of 95%) was considered statistically significant. The statistical analysis was performed using IBM SPSS version 24.0.
ResultsBaseline characteristics of the study populationThe baseline characteristics of the study population are shown in Table 1.
Baseline characteristics of patients with Takotsubo syndrome (n=234).
| Demographic data | |
| Age, years | 68±12 |
| Female gender | 210 (89.7) |
| Women aged over 50 years | 192 (91.3) |
| Postmenopausal women | 168 (80.0) |
| Cardiovascular risk factors | |
| Hypertension | 159 (67.9) |
| Dyslipidemia | 127 (54.3) |
| Diabetes | 44 (18.8) |
| Smoking | 33 (14.1) |
| Personal history | |
| Angina | 19 (8.1) |
| CKD | 15 (6.4) |
| COPD | 11 (4.7) |
| Anemia | 8 (3.4) |
| Heart failure | 6 (2.6) |
| Valvular disease | 6 (2.6) |
| MI | 4 (1.7) |
| Triggering factor | 152 (65) |
| Emotional stress | 109 (46.6) |
| Physical stress | 43 (18.4) |
| Clinical presentation | |
| Chest pain | 204 (87.2) |
| Dyspnea | 51 (21.8) |
| Syncope | 13 (5.6) |
| Killip class ≥2 | 47 (21.4) |
| Electrocardiogram | |
| Sinus rhythm | 216 (92.3) |
| Negative T waves | 94 (40.2) |
| ST-segment elevation | 42 (17.9) |
| Pathological Q waves | 42 (17.9) |
| Prolonged QTc | 24 (10.3) |
| ST-segment depression | 21 (9.0) |
| LBBB | 11 (4.7) |
| Elevated troponin | 208 (89.7) |
| No significant CAD | 195 (87.1) |
| TTE | |
| LVEF, % | 43±11 |
| Significant (grade 3-4) mitral regurgitation | 9 (3.8) |
| LVOT obstruction | 7 (3.0) |
| Classification | |
| Apical | 182 (77.8) |
| Midventricular | 37 (15.8) |
| Basal | 11 (4.7) |
| Focal | 4 (1.7) |
| Hospital stay, days | 6±5 |
CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; LBBB: left bundle branch block; LVEF: left ventricular ejection fraction; LVOT: left ventricular outflow tract; MI: myocardial infarction; QTc: corrected QT interval; TTE: transthoracic echocardiogram.
Information presented as mean ± standard deviation or n (%).
A total of 234 patients with TTS were included, 210 (89.7%) female, mean age 68±12 years. In 65% of the patients a triggering factor was identified, emotional stress in 46.6% and physical stress in 18.4%. On admission, chest pain was the most frequent symptom (87.2%), followed by dyspnea (21.8%) and syncope (5.6%). The admission electrocardiogram (ECG) revealed negative T waves in 40.2%, ST-segment elevation in 17.9% and prolonged QTc in 10.3%.
In 12.9% of the patients, coronary angiography identified significant CAD in myocardial areas not corresponding to the wall motion abnormalities found on the transthoracic echocardiogram.
Regarding the classification of TTS, the apical form was the most frequent (77.8%), followed by midventricular (15.8%).
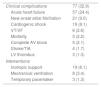
Clinical complications during hospitalizationComplications and interventions during hospitalization are presented in Table 2.
Clinical complications and interventions during hospitalization (n=234).
| Clinical complications | 77 (32.9) |
| Acute heart failure | 57 (24.4) |
| New-onset atrial fibrillation | 21 (9.0) |
| Cardiogenic shock | 19 (8.1) |
| VT/VF | 6 (2.6) |
| Mortality | 5 (2.2) |
| Complete AV block | 5 (2.1) |
| Stroke/TIA | 4 (1.7) |
| LV thrombus | 3 (1.3) |
| Interventions | |
| Inotropic support | 19 (8.1) |
| Mechanical ventilation | 8 (3.4) |
| Temporary pacemaker | 3 (1.3) |
AV: atrioventricular; LV: left ventricular; TIA: transient ischemic attack; VF ventricular fibrillation; VT: ventricular tachycardia.
Information presented as n (%).
During hospitalization, 32.9% of the patients had complications, of which acute heart failure was the most frequent (24.4%).
Regarding intensive care measures, 8.1% of patients received inotropic support and 3.4% underwent mechanical ventilation.
During hospitalization, 49.1% of patients completely recovered LV function, while five (2.2%) died.
Factors associated with complications were history of heart failure (p<0.001), CKD (p=0.001), physical stress as triggering factor (p=0.036), presentation without chest pain (p=0.001), presentation with dyspnea (p<0.001), presence of atherosclerotic lesions in the epicardial coronary arteries (p=0.013), and lower left ventricular ejection fraction (LVEF) on admission transthoracic echocardiography (p<0.001) (Table 3).
Variables associated with clinical complications during hospitalization.
| No complications | Complications | p | Unadjusted OR (95% CI) | |
|---|---|---|---|---|
| History of heart failure | 0% | 7.8% | <0.001 | - |
| CKD | 2.5% | 14.3% | 0.001 | 6.4 (1.96-20.75) |
| Physical stress | 14.6% | 26.0% | 0.036 | 2.0 (1.04-4.01) |
| Chest pain | 92.4% | 76.6% | 0.001 | 0.27 (0.12-0.60) |
| Dyspnea | 12.1% | 41.6% | <0.001 | 5.2 (2.67-9.99) |
| Atherosclerotic coronary lesions | 9.2% | 21.1% | 0.013 | 2.7 (1.21-5.87) |
| LVEF on admission, % | 46±10% | 38±10% | <0.001 | (3.98-11.05) |
CI: confidence interval; CKD: chronic kidney disease; LVEF: left ventricular ejection fraction; OR: odds ratio.
In multivariate analysis, the presence of atherosclerotic lesions in the coronary arteries (p=0.027), lower LVEF on admission (p=0.003), CKD (p=0.02) and clinical presentation with dyspnea (p=0.019) were independent predictors of in-hospital clinical complications (Table 4).
Predictors of in-hospital clinical complications.
| p | Adjusted OR (95% CI) | |
|---|---|---|
| CKD | 0.02 | 7.99 (1.39-45.79) |
| Dyspnea | 0.019 | 3.82 (1.25-11.7) |
| Atherosclerotic coronary lesions | 0.027 | 3.87 (1.17- 12.76) |
| LVEF on admission | 0.003 | 0.93 (0.89-0.98) |
CI: confidence interval; CKD: chronic kidney disease; LVEF: left ventricular ejection fraction; OR: odds ratio.
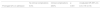
At the mean follow-up of 33±33 months, 12.2% of the patients had complications.
In 4.4% of patients there was recurrence of TTS, 3.1% had stroke/TIA and 0.4% had myocardial infarction. All-cause mortality was 4.4% and cardiovascular mortality was 0.9% (Table 5).
Clinical complications at follow-up (n=229).
| All-cause mortality | 10 (4.4) |
| Non-cardiovascular mortality | 8 (3.5) |
| Cardiovascular mortality | 2 (0.9) |
| TTS recurrence | 10 (4.4) |
| Stroke/TIA | 7 (3.1) |
| Myocardial infarction | 1 (0.4) |
TIA: transient ischemic attack; TTS: Takotsubo syndrome.
Information presented as n (%).
Prolonged QTc on the admission ECG was associated with clinical complications at follow-up (p=0.001) (Table 6).
DiscussionOur multicenter study of TTS patients is one of the largest and its follow-up is among the longest.
Baseline characteristicsThe baseline characteristics of our study population were similar to other series with respect to mean age of diagnosis (68±12 years) and the predominance of female gender (90%). TTS more frequently affects women over 50 years of age.6,12–14
Regarding cardiovascular risk factors, hypertension was the most prevalent (68%), followed by dyslipidemia (54%). The prevalence of these factors is in line with that expected for the age group of patients with TTS.
Only 18% of our patients had been diagnosed with diabetes, which is in agreement with the prevalence reported by other series (5-25%).6,12–17 Patients with TTS have a lower prevalence of diabetes compared to patients with acute coronary syndrome.18 It is not known whether the presence of diabetes is a protective factor for TTS, but this is possible in view of the hypothesis that the autonomic neuropathy of diabetes may influence the myocardial response to an adrenergic storm.18
Clinical presentationChest pain is the most common form of clinical presentation of TTS. In our cohort, 87% of the patients presents with chest pain, as in the series by Eitel et al.19 (88%) and Núñez-Gil et al.20 (90.2%). Other series reported slightly lower rates, between 69% and 81%.6,13,14,17,21 Dyspnea is the second most frequent symptom associated with TTS, with a wide range of prevalences ranging between 8% and 47%.6,13,14,17,21–24 In our cohort, dyspnea was the predominant symptom in 21.8% of the patients.
As for the triggering factor, emotional stress was the most common (46.6%), as also observed in the studies by Yayehd et al.14 (45%) and Prevital et al.23 (36%). However, other studies found that physical factors were more important than emotional factors.6,12,13,19,25 In about one third of our patients, no triggering factor was identified, as in several published studies.6,12,13,23,25
ElectrocardiogramNegative T waves were the most frequent finding on the admission ECG (40.2%). Other series reported similar rates.6,19,20,23 However, there are some differences between our data and the literature with regard to ST-segment elevation. In our study, only 17.9% of patients had ST-segment elevation, but other series reported higher rates (38-44%).6,19,23 In our cohort, 17.9% of the patients had pathological Q waves on the admission ECG, while in Yayehd et al.14 and Schneider et al.21 this figure was 29%. In the study by Schneider et al.,21 pathological Q waves were a predictor of complications during hospitalization. However, further studies are needed to understand their prognostic impact in TTS patients.
Prolonged QTc was found in 10.3% of our patients on the initial ECG. Some studies have reported an association between TTS and prolonged QTc, however the prevalence of this association is unknown.26–29
Electrocardiographic changes in TTS are dynamic and differences in time from symptom onset to admission may explain the discrepancies between studies.
Biomarkers of myocardial necrosisThe majority of our TTS patients had troponin elevation during hospitalization (89.7%), which is in line with other published series, although these use different types of troponin with different units of measurement, which hampers comparisons of the extent of elevation and consequently the interpretation of its clinical significance.6,14,16,17,19,23,24
Left ventricular ejection fractionTTS is characterized by the presence of LV systolic dysfunction at hospital admission.7
In our population, mean LVEF on admission was similar to other series (43±11%).6,14,17,20,23,30 This suggests that patients with TTS suffer myocardial stunning of similar magnitude, regardless of differences in other clinical variables.
At hospital discharge, 49.1% of the patients showed recovery of myocardial function, which was complete in all patients at follow-up, in accordance with the diagnostic criteria of TTS.
Classification of Takotsubo syndromeConcerning the classification of TTS, the apical type was the most frequent (77.8%) followed by midventricular (15.8%) and basal (1.7%), similar findings to those in other series.6,24,30
Coronary artery diseaseTTS and CAD are not mutually exclusive. Given the mean age at diagnosis and the prevalence of cardiovascular risk factors, CAD can coexist with TTS.31 In our cohort, 12.9% of patients had concomitant CAD. In the literature, reported rates are between 9.8% and 19%.6,25,31–34
Clinical complications during hospitalizationInitially, TTS was described as a benign condition.2 However, more recent series have shown high rates of in-hospital complications that should not be overlooked (21.8-52%).6,21,22,30,35,36
In our population, 32.9% of patients presented complications, of which acute heart failure was the most common (24.4%). In fact, acute heart failure is the main clinical complication in TTS, with rates reported in the literature between 16% and 44%.15–17,20,25,35,37
In the heart failure spectrum, cardiogenic shock is the most severe manifestation. In our study, this complication occurred in 8.1% of patients, while other studies report rates between 4.7% and 12.4%.6,13,15,30,34,36 Due to the reversibility of LV dysfunction, it could be expected that cardiogenic shock in TTS would have a lower prognostic impact than in ACS, but Stiermaier et al.30 demonstrated that it is associated with higher short- and long-term mortality.
AF was the most common arrhythmia in our cohort, being found in 15% of our patients, with other series reporting rates between 6% and 15%.13,21,24,38,39 El-Battrawy et al.39 demonstrated that the presence of previously known or first diagnosed AF is associated with higher mortality, both in-hospital and in long-term follow-up.
In our population, 2.6% of the patients had ventricular arrhythmias, a lower figure than in other series, such as Citro et al.37 (4.5%) and Schneider et al.21 (8%).
Complete atrioventricular block, stroke and LV thrombus are less frequent clinical complications, with rates ranging from 0.6% to 3.8%.6,15,21,23,37,40
Predictors of in-hospital clinical complicationsIn our cohort, a history of CKD (p=0.02), clinical presentation with dyspnea (p=0.019), atherosclerotic lesions in the epicardial coronary arteries, and lower LVEF on admission (p=0.003) were predictors of in-hospital clinical complications.
CKD is known to be associated with worse cardiovascular prognosis.41 However, to our knowledge, this association has not yet been reported in TTS.
To our knowledge, our work is the first to identify CAD as a predictor of in-hospital complications in patients with TTS. Parodi et al.31 found no differences in short- and medium-term prognosis in patients with CAD, whereas Bill et al.33 identified this factor as a predictor of medium-term all-cause mortality.
LV systolic dysfunction would be expected to be associated with a worse outcome. In the study by Citro et al.,24 LVEF was a predictor of heart failure, and in series by Schneider et al.21 and Ribeiro et al.,22 LVEF of ≤30% and ≤35%, respectively, predicted in-hospital complications.
Templin et al.,6 studying 1750 patients, identified LVEF on admission, physical stress, troponin level and neurological or psychiatric disease as predictors of complications.
Other series, with significantly smaller numbers of patients, have identified other predictors, such as the presence of pathological Q waves on admission,21 age ≥75 years,37 brain natriuretic peptide and white blood cell count,25 heart rate, and sum of ST-segment elevation on the 12-lead ECG.25
Differences in sample sizes and in the characteristics of study populations result in the identification of different predictors of complications. This makes it difficult to accurately stratify in-hospital risk for TTS patients.
Our series constitutes the second largest series of TTS patients in which predictors of in-hospital complications are identified.
In-hospital mortalityIn-hospital mortality in our population was 2.2%, a relatively low figure considering the high rate of acute complications. Other studies report rates between 0% and 12.2%.6,13–16,21,24,25,32,42,43
Asian series25,32,42,43 have higher mortality (8.4-12.2%), probably due to differences in the baseline characteristics of the included patients, such as higher percentages of male gender and physical stress as a triggering factor. In support of this hypothesis, Sobue et al.42 identified male gender and physical stress as predictors of in-hospital mortality. Beyond these factors, it has been demonstrated that in-hospital mortality is associated with underlying serious illness such as sepsis, acute renal injury, respiratory failure and cancer.15,42
Prognosis in follow-upThe medium and long-term prognosis of TTS patients is described as favorable, with rapid and complete recovery of LV systolic function.7,19,44
Patients in our study had a good prognosis at the mean follow-up of 33±33 months, with all-cause mortality of 4.4%. Other studies, with different follow-up times, reported all-cause mortality between 2.9% and 24.7%.13,16,17,22,43,45–47 In our study, most deaths were from non-cardiac causes (3.5% of the sample). Other series have also shown that medium- and long-term mortality of TTS patients is more often due to non-cardiac causes than to the syndrome itself. Thus, comorbidities significantly affect the prognosis of these patients.13,40,45
The recurrence rate of TTS was 4.4%. Other series have reported rates between 0% and 11.4%.6,13,14,16,17,23,47 Elesber et al.,17 in a study of 100 patients with TTS, observed recurrence in 11.4% at four years of follow-up. Lower rates are reported by series with shorter follow-up.13,14,23
Regarding cardiovascular and cerebrovascular events, in our study 3.1% of patients had stroke/TIA and 0.4% had myocardial infarction. In Templin et al.,6 the rate of major cardiovascular and cerebrovascular events was 9.9%/year and the rate of stroke/TIA was 1.7%/year.
The observed variability in mortality and clinical complications is related to the number of patients included and the follow-up times in the different series.
In our study, prolonged QTc on admission was associated with events in follow-up (p=0.001). Some studies have observed an association between TTS and prolonged QTc, but there is little evidence on its prognostic impact.26,28,43
Song et al.43 found that patients with long QTc presented a higher prevalence of cardiogenic shock and ventricular arrhythmias and lower LVEF compared to the group with normal QT interval. Similarly, Imran et al.28 demonstrated that prolonged QTc was associated with in-hospital clinical complications.
LimitationsCertain limitations should be borne in mind when assessing our results. This was a retrospective observational study and as such is subject to inherent bias. However, it is a multicenter study with a significant number of patients. The small number of events at follow-up meant it was not possible to identify predictors of medium-term prognosis or of in-hospital and follow-up mortality. In this study, treatment administered on admission and during follow-up was not analyzed, which is a limitation. The centers participating in the study did not routinely use laboratory hormone tests or imaging to exclude pheochromocytoma or myocarditis. The degree of coronary stenosis was not assessed by fractional flow reserve, nor were atherosclerotic plaques characterized by intravascular ultrasound or optical coherence tomography.
ConclusionOur study confirms the low mortality associated with TTS. However, the high rate of in-hospital complications shows that TTS is not as benign as previously described. In our study, CKD, clinical presentation with dyspnea, CAD and lower LVEF on admission were predictors of in-hospital clinical complications.
In the medium term, TTS has a good prognosis, with low rates of mortality, stroke and recurrence. Mortality at follow-up is predominantly due to non-cardiac causes. Prolonged QTc on admission was associated with complications at follow-up.
Conflicts of interestSUNSHINE is supported by BIAL, MSD, Shire, Pfizer, BMS and Trigenius.
SUNSHINE group investigators:
Ana Marques1; Ana Pereira1; Andreia Pereira2; Bebiana Faria3; Bruno Piçarra4; Carolina Négrier5; Catarina Gomes1; Clara Cordeiro6,7; Daniela Silva6,8; Davide Moreira9; Emanuel Correia9; Fernando Sá5, Hugo Antunes9; Inês Cruz1; Joana Chin10; Joana Silva5; João Bispo6,8; João Guedes6,8; João Português3; Júlio Pereira9; Lucy Calvo3; Luís Abreu9; Luís Lopes1; Luís Morais11; Luis Puga5; Luísa Gonçalves9; Margarida Oliveira3; Maria Vieira12; Micaela Neto2, Miguel Alves12; Nuno Craveiro5; Pedro Azevedo6,8; Pedro Daniel1; Pedro Magalhães13; Pedro von Hafe3; Renata Gomes14; Rogério Teixeira5; Rúben Ramos; Samuel Almeida12; Sílvia Leão13; Sofia Alegria9; Sofia Carvalho13.
1 Cardiology Department, Hospital Garcia de Orta, Almada, Portugal
2 Cardiology Department, Hospital Dr. Nélio Mendonça, Funchal, Portugal
3 Cardiology Department, Hospital da Senhora da Oliveira, Guimarães, Portugal
4 Cardiology Department, Hospital do Espírito Santo, Évora, Portugal
5 Cardiology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
6 Algarve Biomedical Center, Faro, Portugal
7 Departamento de Ciências Biomédicas e Medicina, Universidade do Algarve, Faro, Portugal
8 Cardiology Department, Centro Hospitalar Universitário do Algarve, Faro, Portugal
9 Cardiology Department, Centro Hospitalar Tondela-Viseu, Portugal
10 Cardiology Department, Centro Hospitalar Barreiro-Montijo, Montijo, Portugal
11 Cardiology Department, Hospital de Santa Marta, Centro Hospitalar Lisboa Central, Lisboa, Portugal
12 Cardiology Department, Hospital de Santarém, Santarém, Portugal
13 Cardiology Department, Centro Hospitalar de Trás-os-Montes e Alto Douro, Vila Real, Portugal
14Cardiology Department, Hospital de Santo Espírito da Ilha Terceira, Angra do Heroísmo, Portugal