A 50-year-old man, with chronic kidney disease and on dialysis, underwent coronary angiography in the context of acute coronary syndrome, which revealed focal lesions (type A) in the proximal left anterior descending and mid circumflex arteries. Ad-hoc angioplasty was performed on both lesions with direct stenting. An immediate drop in arterial blood pressure was observed and the angiogram showed new lesions with reduced flow throughout the coronary tree, progressing to cardiogenic shock and electromechanical dissociation. During cardiopulmonary resuscitation maneuvers, intracoronary verapamil was administered and TIMI 3 flow, sinus rhythm and a rise in blood pressure were obtained. Clinical stability was progressively restored. The patient was discharged medicated with calcium channel blockers and nitrates. During follow-up, he was twice readmitted for unstable angina. Coronary angiography revealed findings that could easily have been interpreted as new obstructive lesions, but these resolved after administration of intracoronary nitrates.
Homem de 50 anos, insuficiente renal crónico em hemodiálise, submetido a cateterismo cardíaco no contexto de síndrome coronária aguda, que revelou lesões estenóticas focais (tipo A) localizadas na descendente anterior proximal e circunflexa média. Efetuou-se angioplastia ad-hoc com implantação direta de stent. Imediatamente depois, observa-se abrupta queda tensional e o angiograma revela «novas» lesões com redução do fluxo em toda a árvore coronária e instalação de choque cardiogénico. Durante as manobras de reanimação, em dissociação eletromecânica, é administrado verapamil intracoronário com obtenção fluxo coronário TIMI 3, ritmo sinusal e pressão arterial. Assistiu-se progressivamente à melhoria e estabilização clínica. Foi implementado tratamento com antagonistas do cálcio e nitratos, registando-se no seguimento mais 2 admissões hospitalares por angor instável. A coronariografia voltou a revelar locais na árvore coronária que poderiam ser facilmente interpretados como novas lesões, mas as «estenoses» angiográficas foram solucionadas após administração de vasodilatadores intracoronários.
Spontaneous coronary vasospasm is associated with changes in autonomic nervous system activity1 (sympathovagal imbalance) and endothelial dysfunction2,3 (reduced nitric oxide bioavailability). It is considered to be the pathophysiological mechanism behind variant or Prinzmetal angina and occurs in 1–5% of diagnostic procedures and percutaneous interventions as these can trigger or aggravate coronary spasm through endothelial injury or trauma.4 Its location, distribution and severity determine the seriousness of the clinical setting, which can include myocardial infarction, severe arrhythmias, cardiogenic shock and even death.5 Treatment in the acute phase is based on coronary artery vasodilators.
Case reportA 50-year-old man, a smoker, hypertensive, with chronic kidney disease on regular dialysis, but no history of heart disease, cocaine use, syncope or cardiovascular events, was admitted for chest pain at rest of short duration that occurred during an evening dialysis session.
He had already been referred for invasive coronary angiography for similar episodes in the previous few months, although no evidence of significant ischemia had been found on myocardial perfusion scintigraphy.
On arrival in the emergency department, he was almost completely asymptomatic (only residual pain) and was admitted for unstable angina (no significant ECG changes and negative markers of myocardial necrosis). Global and segmental left ventricular systolic function was preserved.
Risk stratification for myocardial infarction/death was: (a) GRACE score: 5% in-hospital and 13% at 6 months; (b) TIMI score: 5% at 14 days.
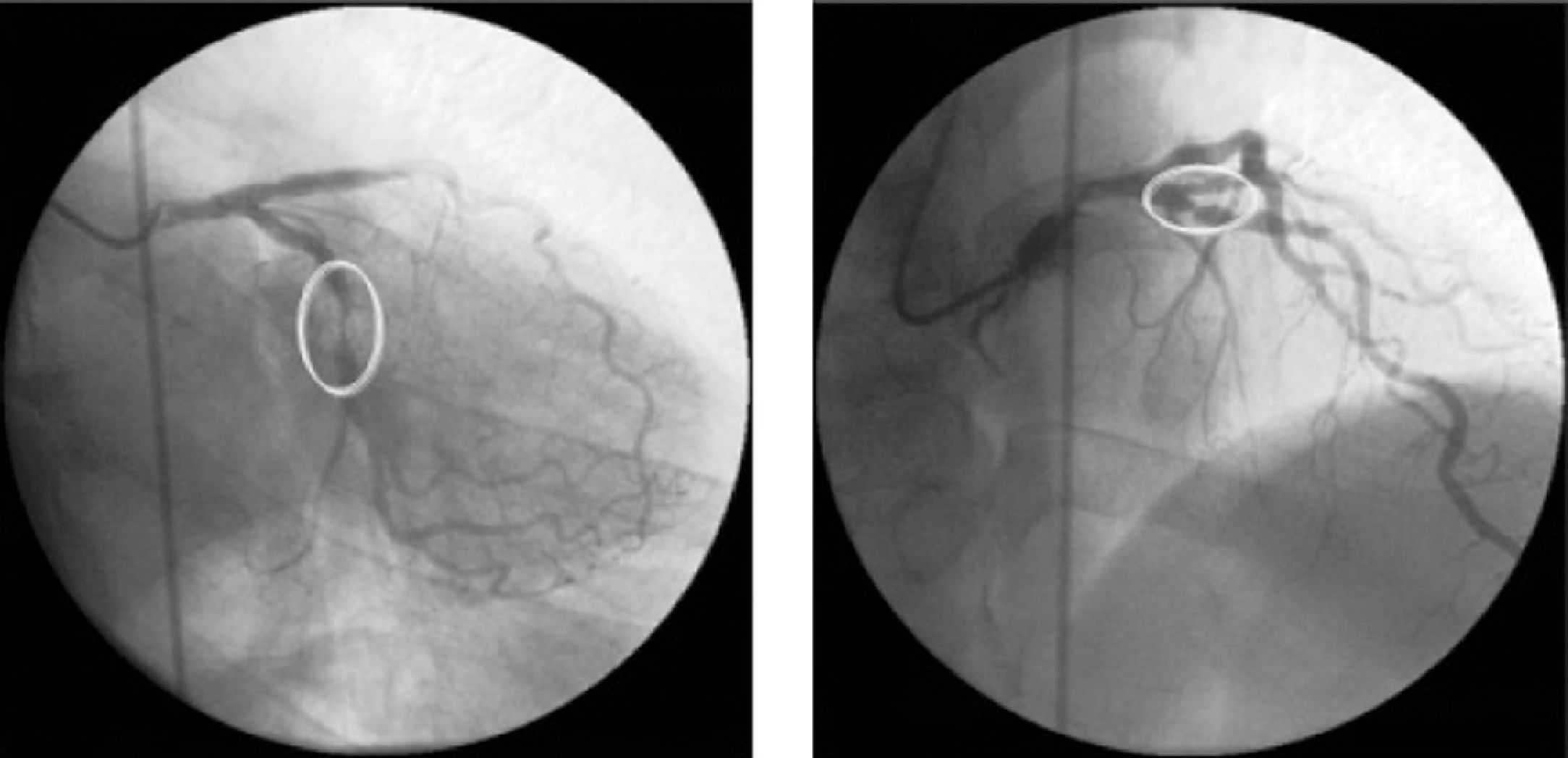
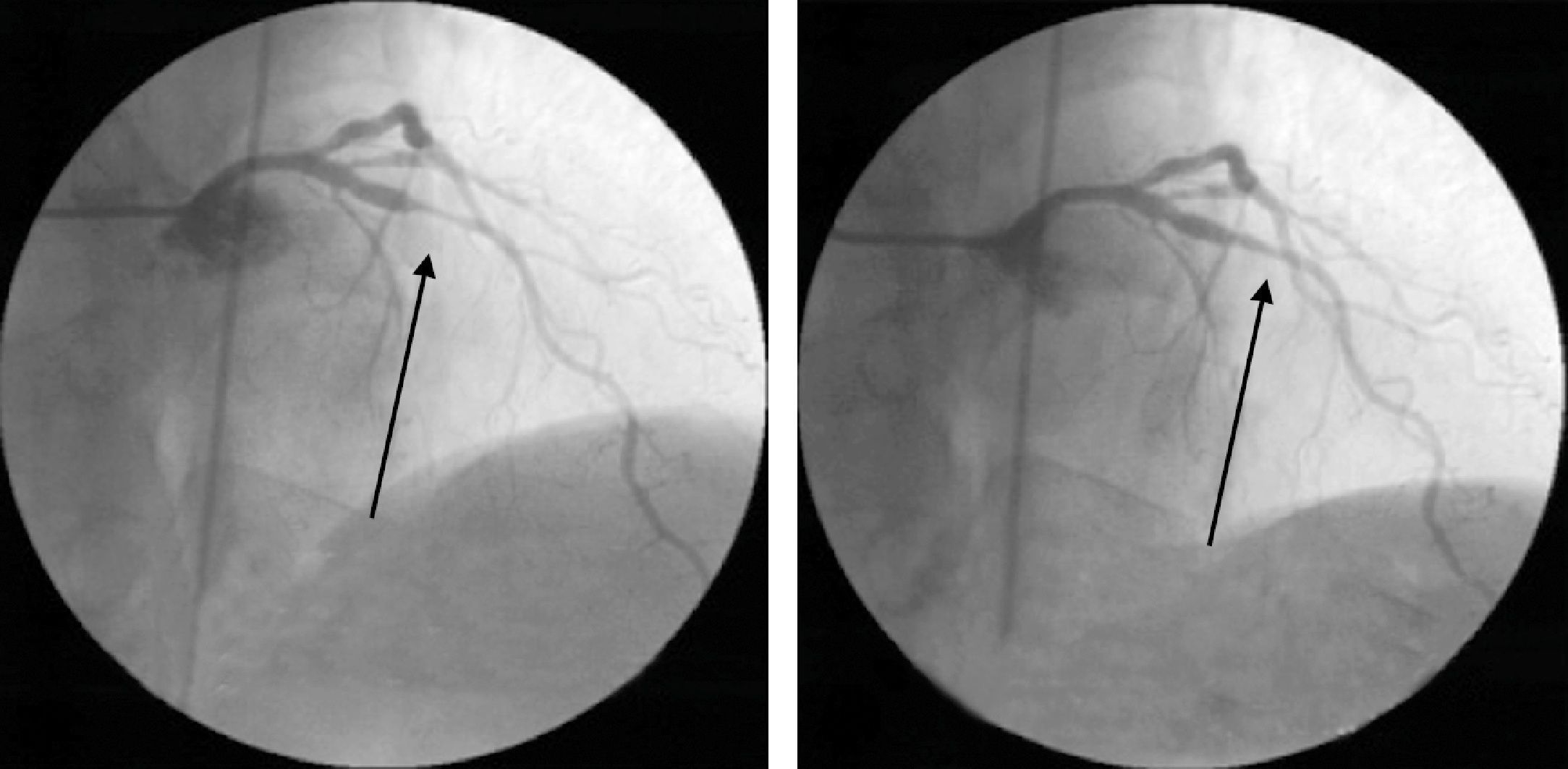
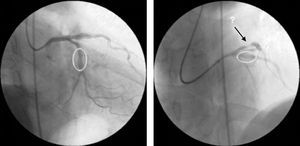
Cardiac catheterization was performed the following day, which revealed focal type A lesions in the proximal left anterior descending artery (LAD) and mid circumflex artery (Fig. 1).
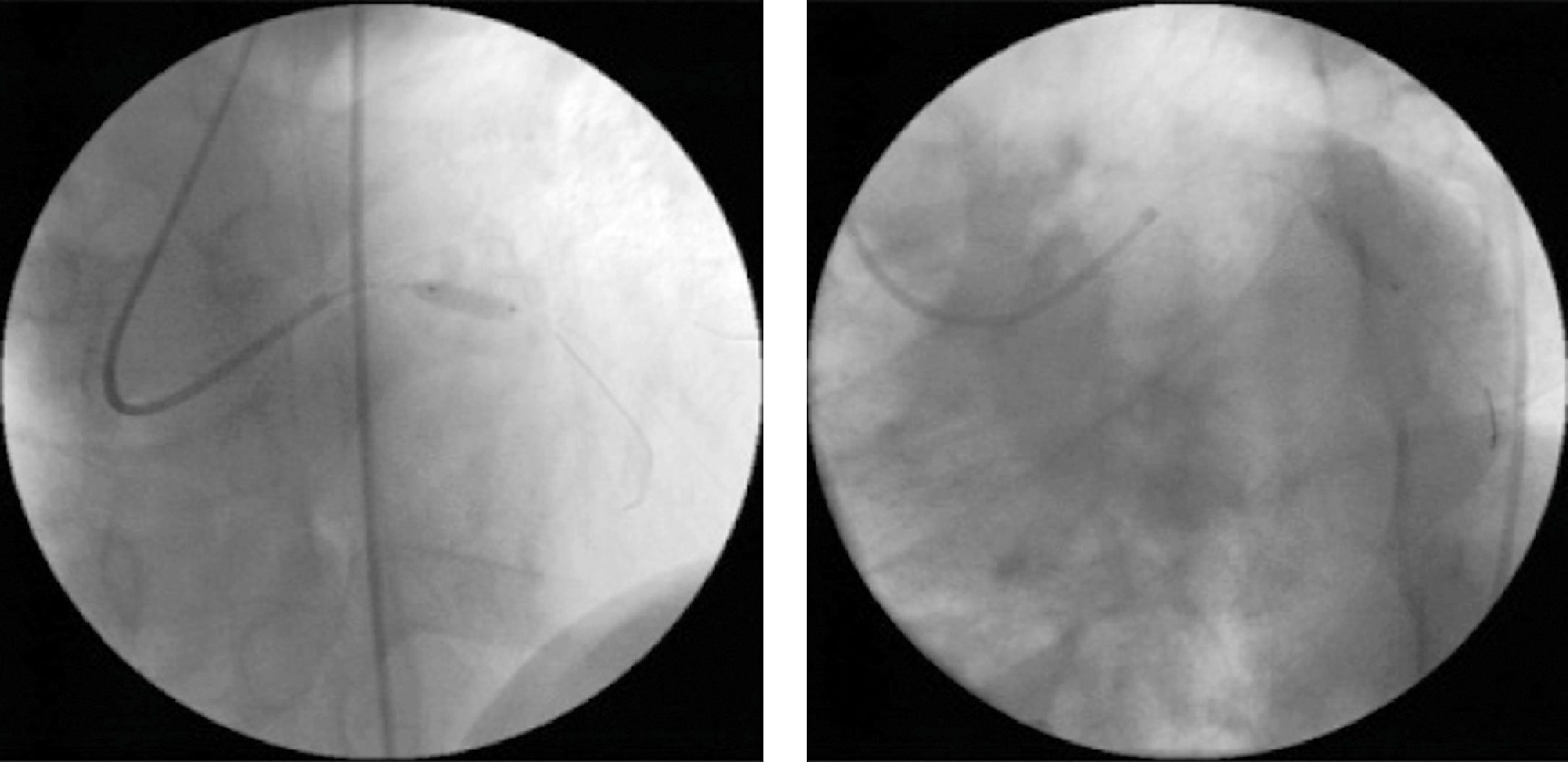
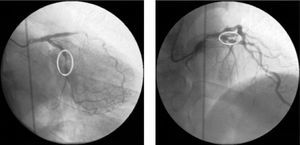
Ad-hoc angioplasty was performed on both vessels with direct stenting (Fig. 2), using standard intracoronary devices (3.0mm×12mm in the proximal LAD and 3.0mm×15mm in the circumflex artery).
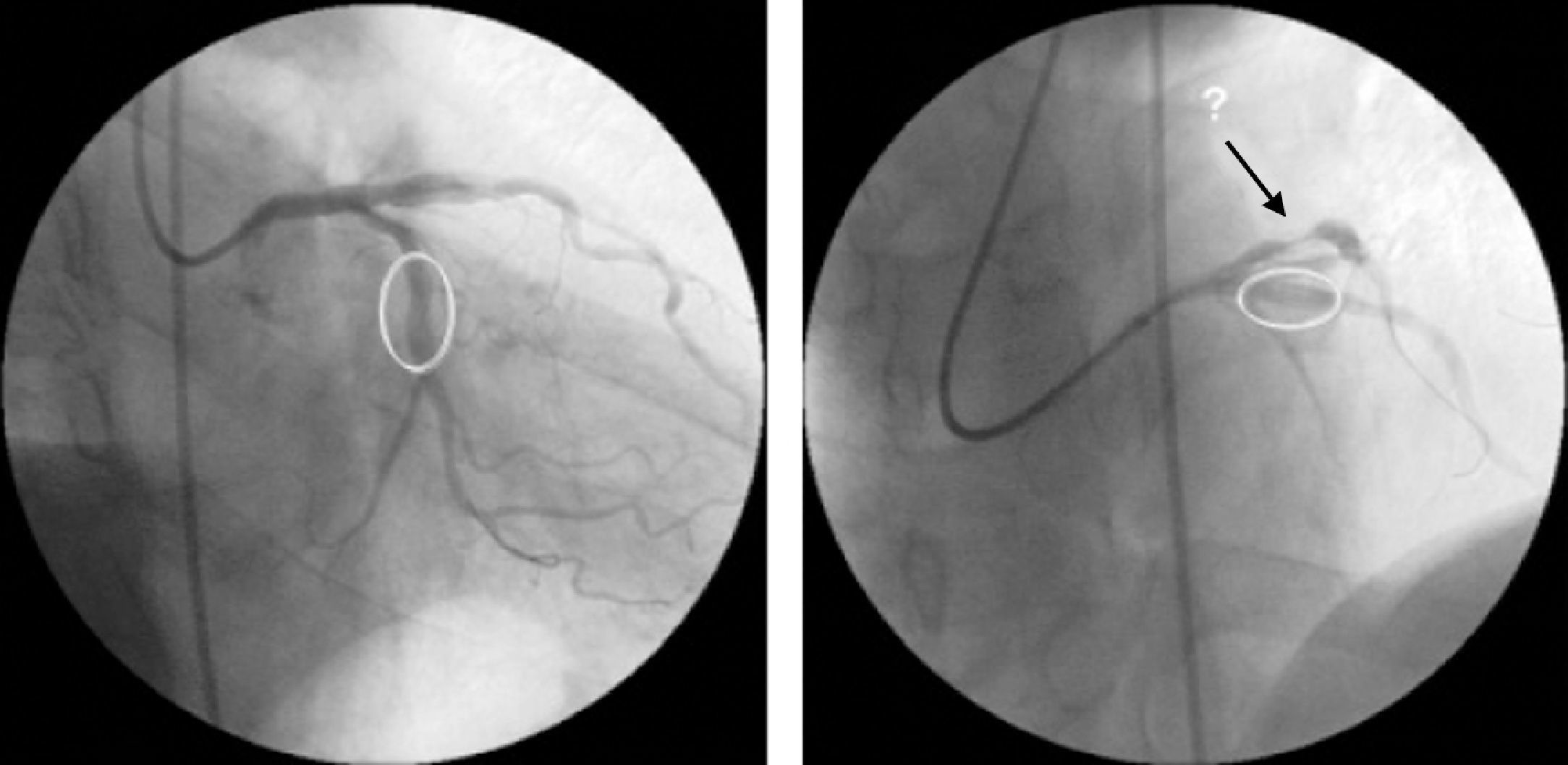
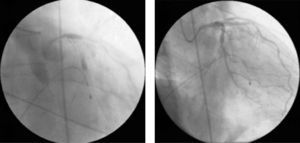
Angiographic control of the last lesion treated (proximal LAD) showed a good angiographic result at the stent implantation site, but a new pre-stent lesion was now visible in the proximal circumflex artery (Fig. 3).
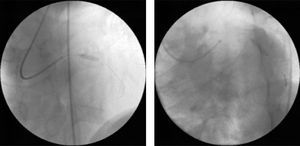
Immediately afterwards there was a drop in arterial blood pressure and the angiogram revealed other new lesions and reduced flow throughout the coronary tree. The patient went into cardiogenic shock and the coronary angiogram showed retention of contrast at various points of the left coronary artery, principally intrastent, and TIMI 0 distal flow (Fig. 4A). Basic and advanced life support maneuvers were begun, a temporary pacing lead was implanted (due to complete atrioventricular block followed by ventricular asystole) and an intra-aortic balloon pump was inserted.
There were various possible causes for this situation including coronary dissection and no-reflow phenomenon, but the most likely in view of the clinical and angiographic context was severe diffuse vasospasm of the coronary tree; intracoronary verapamil was accordingly administered while the patient was still undergoing resuscitation maneuvers and in electromechanical dissociation. This, together with the rest of the pharmacological arsenal and resuscitation efforts, was successful in obtaining TIMI 3 flow (Fig. 4B), sinus rhythm and a rise in blood pressure.
Invasive ventilation and hemodynamic support with intra-aortic balloon pump were required for 48hours, and resulted in progressive improvement and clinical stabilization.
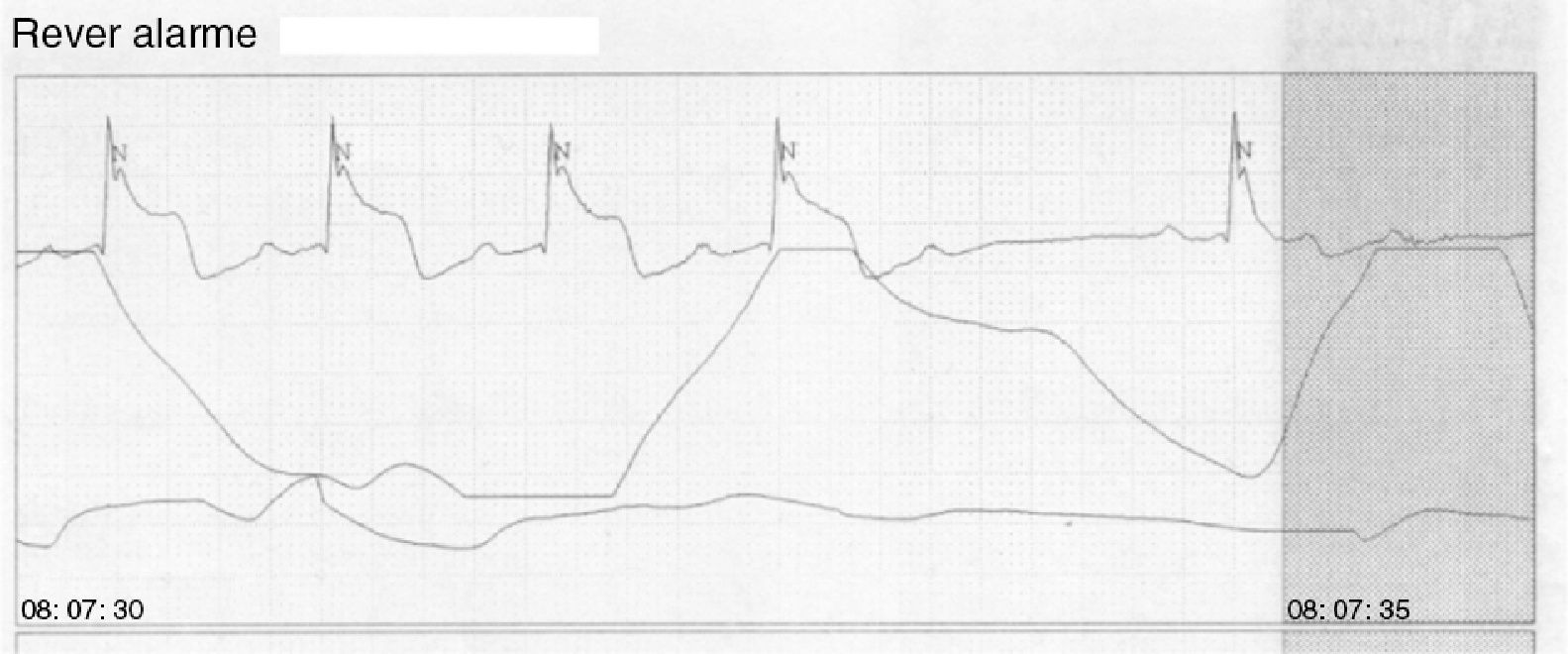
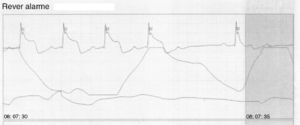
During hospital stay, there were various episodes of angina associated with transient ST-segment elevation on continuous ECG monitoring (Fig. 5), which resolved after administration of coronary vasodilators.
The patient was discharged home, asymptomatic, medicated with calcium channel blockers and nitrates. He has since been readmitted twice for unstable angina, with a similar clinical setting to the first admission. In both cases, the patient had completely or partially discontinued the recommended therapy.
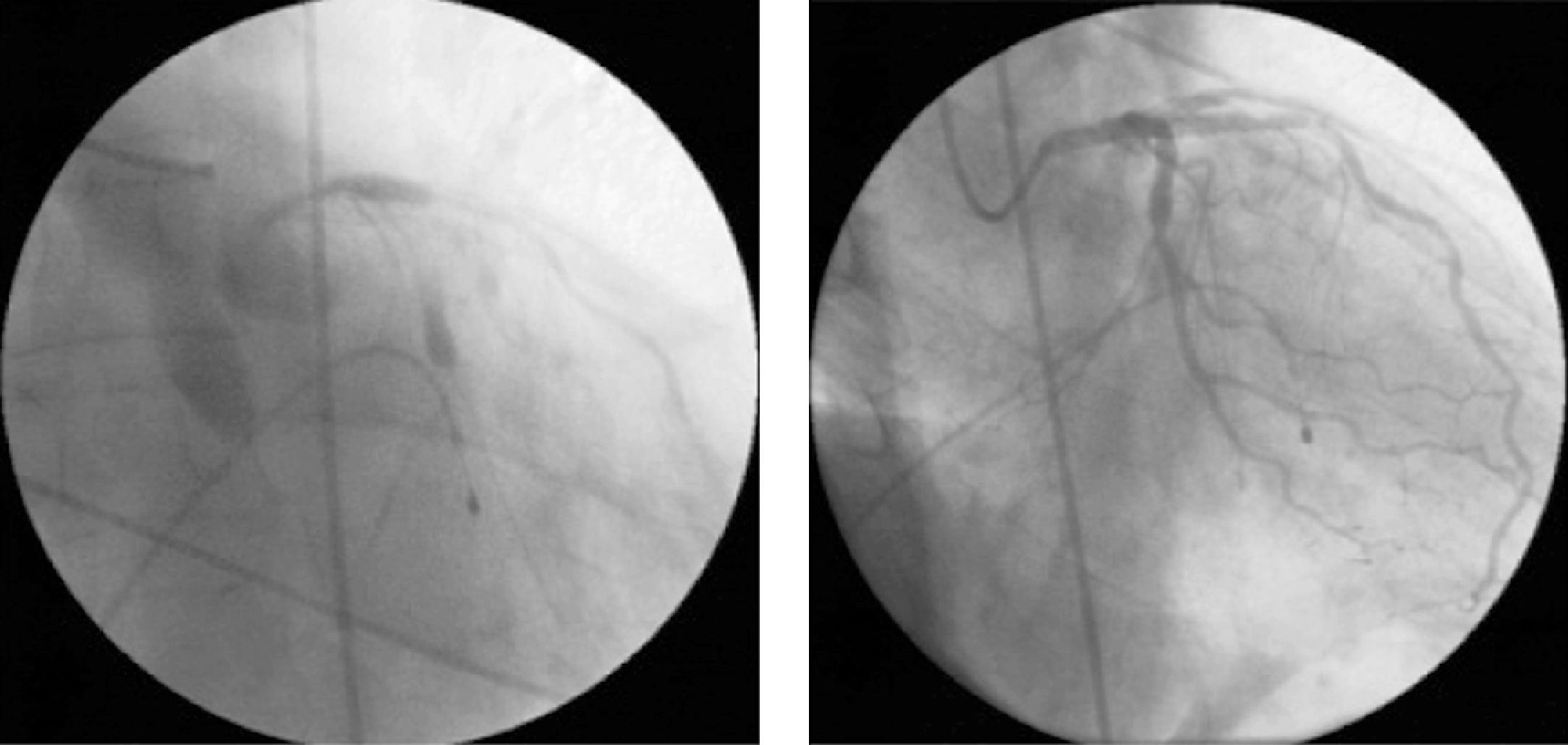
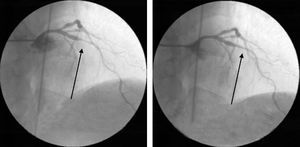
During the latest hospitalization, invasive coronary angiography was repeated, which once again revealed coronary findings that could easily have been interpreted as new lesions, but these resolved after aggressive treatment with intracoronary nitrates (Fig. 6).
DiscussionPatients with variant angina present typical chest pain at rest associated with transient ST-segment elevation, mainly at night or in the early morning.6
Diagnostic coronary angiography, with administration of intracoronary nitrates and if necessary injection of contrast for non-selective catheterization, excludes the possibility of coronary vasospasm as opposed to obstructive atherosclerotic disease in most cases.7
Not all the typical clinical and imaging features of vasospastic coronary artery disease were present in our patient at admission. While he had experienced several anginal episodes at rest, almost all had occurred during evening dialysis sessions, and there was no evidence of significant ischemia on myocardial perfusion scintigraphy performed in the month prior to the first hospital admission. These findings could be taken as supporting the hypothesis of vasospastic angina. However, on initial assessment following admission with the patient still presenting residual angina, serial electrocardiograms did not show significant ST-T changes and initial administration of nitrates during diagnostic coronary angiography did not alter the angiographic appearance of the lesions observed. The latter two findings contributed to the operators’ decision to proceed to coronary angioplasty, in the belief that it was a case of fixed coronary obstruction.
Although coronary vasospasm tends to resolve spontaneously, prolonged episodes can lead to myocardial infarction, arrhythmias and sudden cardiac death. In the case presented, coronary intervention played a major role in exacerbating coronary spasm, resulting in cardiogenic shock,8 and death was only prevented by rapid diagnosis and appropriate treatment.
The administration of intracoronary verapamil was providential, since although it is contraindicated in cardiogenic shock with electromechanical dissociation, it was key to resolving this patient's severe vasospasm and thus to his survival.
As also seen in our patient, vasospasm can recur in different locations to the treated segment, and even in multiple vessels.9
Coronary revascularization (whether percutaneous or surgical) is not indicated in cases of isolated coronary spasm without fixed coronary stenosis.2 Our patient's coronary anatomy was reassessed during subsequent admissions, with due caution in the light of what had occurred during the first hospitalization, and with generous doses of intracoronary nitrates in order to establish a differential diagnosis between isolated vasospasm (which was in fact confirmed) and obstructive atherosclerotic disease.
Although not used in this case, intravascular ultrasound or optical coherence tomography can be valuable in characterizing arterial wall atherosclerosis, and thus provide important additional information on the therapeutic approach to adopt.
Cardiac rhythm disturbances are common during vasospastic crises, notably atrioventricular block and severe ventricular arrhythmias.
In most cases of variant angina, appropriate treatment with vasodilators prevents new episodes of vasospasm. Cardioverter-defibrillator implantation should be considered in refractory vasospastic angina complicated by syncope and/or severe ventricular arrhythmias.10
The prognosis of variant angina is good if it is associated with normal coronary arteries and responds well to treatment with calcium channel blockers or nitrates. The incidence of myocardial infarction, malignant arrhythmias and sudden death is low in these patients.5
Persistence of symptoms is normally associated with active smoking11 or suboptimal doses of anti-anginal drugs, which was once again seen in our case.
ConclusionsCoronary vasospasm is not a benign entity and can have a fatal outcome. It is therefore imperative to obtain effective coronary vasodilation, for which verapamil may be a good choice, even in the worst hemodynamic scenarios.
Administration of potent coronary vasodilators (intracoronary nitrates or verapamil) should be borne in mind for accurate assessment of the severity of angiographic lesions before proceeding to percutaneous intervention.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Guardado, J; Grave vasoespasmo coronário. Rev Port Pneumol. 2012. http://dx.doi.org/10.1016/j.repc.2012.06.002.