Acute heart failure in patients with severe aortic stenosis and left ventricular systolic dysfunction is well known for its dire prognosis and limited therapeutic options.
The authors describe the case of a man admitted for non-ST-elevation myocardial infarction. Diagnostic exams revealed severe aortic stenosis, with good left ventricular systolic function, and two-vessel coronary artery disease. The development of cardiogenic shock with left ventricular systolic dysfunction on day four led to changes in the therapeutic strategy. Percutaneous aortic balloon valvuloplasty coupled with complete myocardial revascularization was performed with a view to future surgical intervention. After discharge, the patient was readmitted with cardiogenic shock after acute pulmonary edema and cardiopulmonary arrest. Ventilator weaning was not possible due to acute heart failure and so it was decided to administer levosimendan, which resulted in substantial clinical and echocardiographic improvement. The patient subsequently underwent successful aortic valve replacement.
This case highlights the challenge that characterizes the management of patients with concomitant coronary artery disease, left ventricular systolic dysfunction and severe aortic stenosis. Percutaneous aortic balloon valvuloplasty and levosimendan were safe and effective in the treatment of acute heart failure, acting as a bridge to surgery.
A insuficiência cardíaca aguda na estenose aórtica grave com compromisso da função sistólica global tem um prognóstico reservado, com opções terapêuticas limitadas.
Os autores descrevem o caso clínico de um doente admitido por enfarte agudo do miocárdio sem supradesnivelamento de ST, no qual o estudo complementar revelou estenose aórtica grave, com boa função ventricular esquerda, e doença coronária de 2 vasos. O desenvolvimento de choque cardiogénico, com compromisso grave da função sistólica global, ao quarto dia de internamento, alterou a estratégia terapêutica, optando-se por realizar valvuloplastia aórtica com balão e revascularização miocárdica percutânea completa, com vista a posterior referenciação para cirurgia valvular. Após a alta, apresentou novo quadro de choque cardiogénico em contexto de insuficiência cardíaca aguda e paragem cardiorrespiratória. Por dificuldade na extubação, iniciou perfusão de levosimendan, com franca melhoria clínica e ecocardiográfica. Posteriormente, o doente foi submetido com sucesso a implantação de prótese valvular aórtica.
Este caso demonstra o desafio que caracteriza a estabilização e o tratamento destes doentes. A valvuloplastia aórtica com balão e o levosimendan foram eficazes e seguros no tratamento da insuficiência cardíaca aguda e permitiram estabelecer a ponte para a cirurgia.
Degenerative aortic stenosis (AS) is the most prevalent valve disease in developed countries (4.6% in patients aged over 75,1 a figure that is expected to rise with ageing populations). When symptomatic it is associated with high mortality and surgical valve replacement becomes a priority.2 The surgical risk of replacement is generally low and long-term results are excellent, the survival curve being close to that of the general population. However, prognosis is less good in patients with left ventricular (LV) dysfunction, particularly those with acute heart failure (HF). Such patients are usually excluded from clinical trials and clinical evidence in this area is sparse; therapeutic options are accordingly limited.
Percutaneous aortic balloon valvuloplasty (PABV) was first described in 1986 by Cribier et al.3 as an alternative to surgery. Despite initial enthusiasm, medium- and long-term results were disappointing, with high restenosis rates (>70% after the first year) and no beneficial effect on the natural course of the disease.4 It is now used as a palliative measure or as a bridge to more permanent treatment.5
Levosimendan has both positive inotropic and vasodilatory effects without increasing myocardial oxygen consumption.6 Its main active metabolite, OR-1896, prolongs its time of action to 7-9 days.7 Vasodilators have traditionally been considered to be contraindicated in severe AS, but this has recently been challenged.8
The case presented here highlights the therapeutic challenge posed by patients with severe AS and cardiogenic shock. PABV and levosimendan were two therapeutic options that proved safe and effective.
Case reportA 67-year-old man with a history of hypertension, insulin-treated type 2 diabetes, hypertriglyceridemia, obesity and obstructive sleep apnea syndrome, and suspected poor compliance with medication, was admitted to the emergency department with anginal chest pain of around six months’ duration, worsening in the previous two weeks (CCS class II-III). Physical examination him to be hemodynamically stable (blood pressure 107/43 mmHg, heart rate 60 bpm); cardiac auscultation revealed a grade III/VI crescendo-decrescendo systolic murmur over the aorta radiating to the carotid arteries but no signs of HF. The ECG showed sinus rhythm with voltage criteria for LV hypertrophy, repolarization abnormalities of the lateral wall suggestive of overload and/or myocardial ischemia, and poor R-wave progression in V1-V4. There was a slight isolated rise in troponin I (0.071-0.102 ng/ml) on laboratory testing.
The patient was admitted to the cardiac intensive care unit with a diagnosis of non-ST-elevation myocardial infarction, in Killip class I.
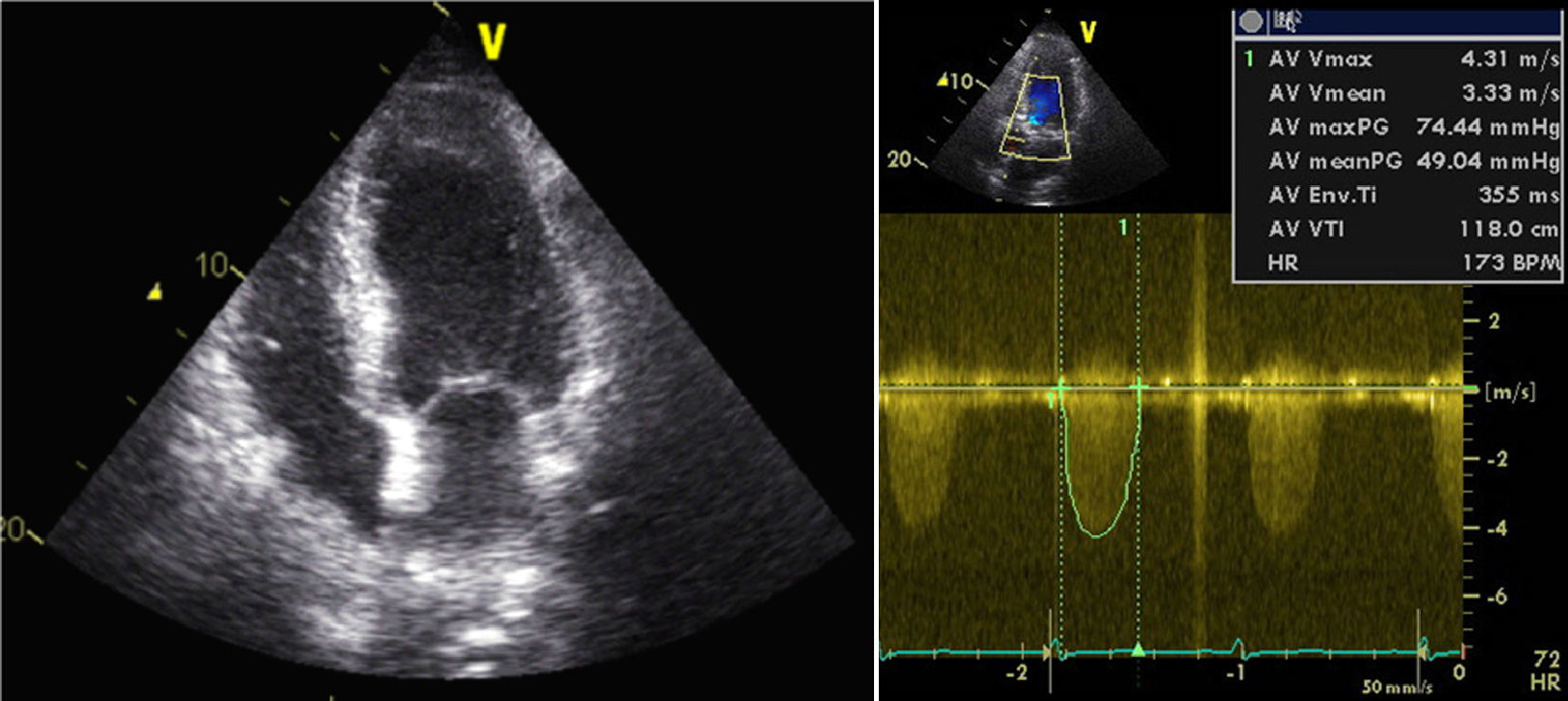
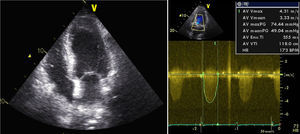
The transthoracic echocardiogram (Figure 1) revealed a non-dilated left ventricle with mild hypertrophy of the ventricular septum and good global and segmental systolic function, a calcific aortic valve with a peak transvalvular gradient of 74 mmHg and mean gradient of 49 mmHg, and valve area of 0.77 cm2 calculated by the continuity equation.
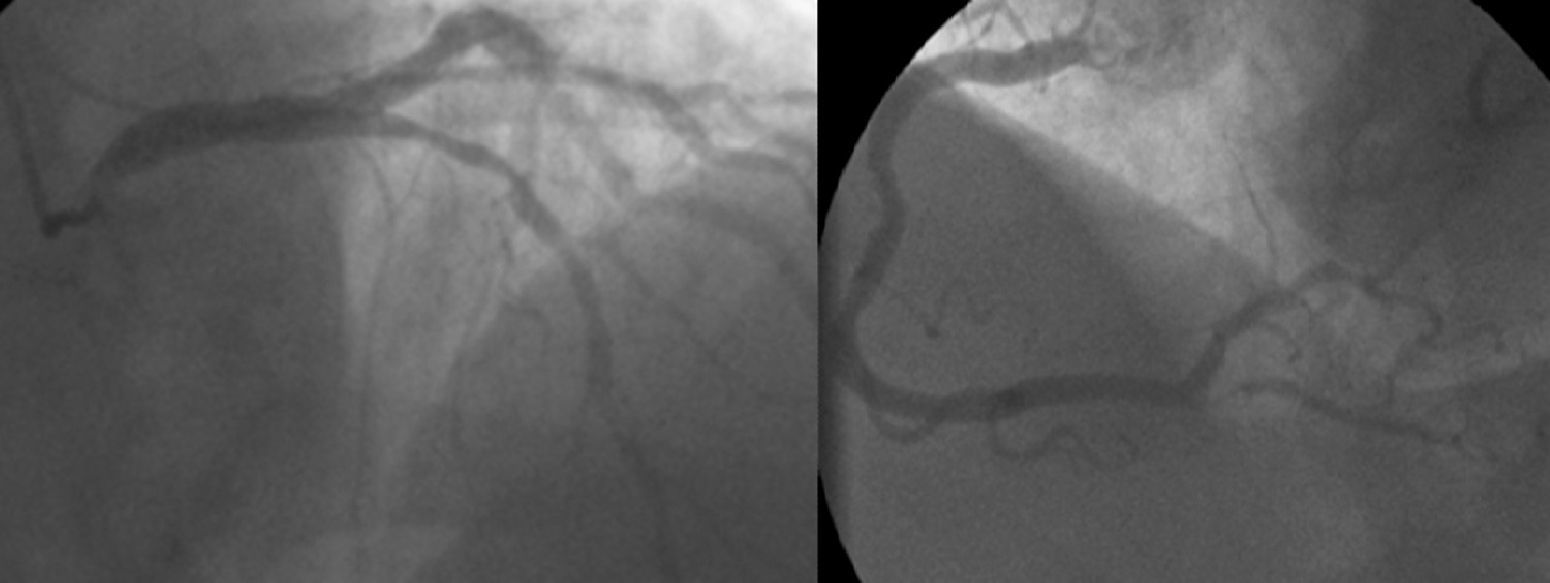
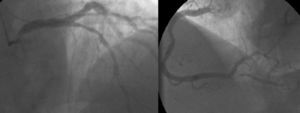
Coronary angiography (Figure 2) showed two-vessel coronary artery disease (75% lesion in the mid left anterior descending artery and 90% lesion at the origin of the posterior descending artery). Hemodynamic study revealed an aortic valve gradient of 97 mmHg.
Given the diagnosis of severe AS and two-vessel coronary artery disease, surgery was scheduled for implantation of an aortic valve prosthesis and myocardial revascularization. However, on day four the patient developed angina at rest, with dyspnea and agitation, associated with hemodynamic instability (blood pressure 80/60 mmHg, sinus tachycardia and signs of poor peripheral perfusion). Following the diagnosis of cardiogenic shock, optimized medical therapy, mechanical ventilation and high-dose vasopressor and inotropic support (noradrenaline 20 μg/min and dobutamine 15 μg/kg/min) were begun.
The ECG showed sinus tachycardia with more marked ST depression (2 mm) in the lateral wall. Echocardiography revealed apical akinesia with moderate to severe global systolic dysfunction and a mean aortic gradient of 44 mmHg; laboratory tests showed elevation of troponin I to 12 ng/ml and worsening renal function.
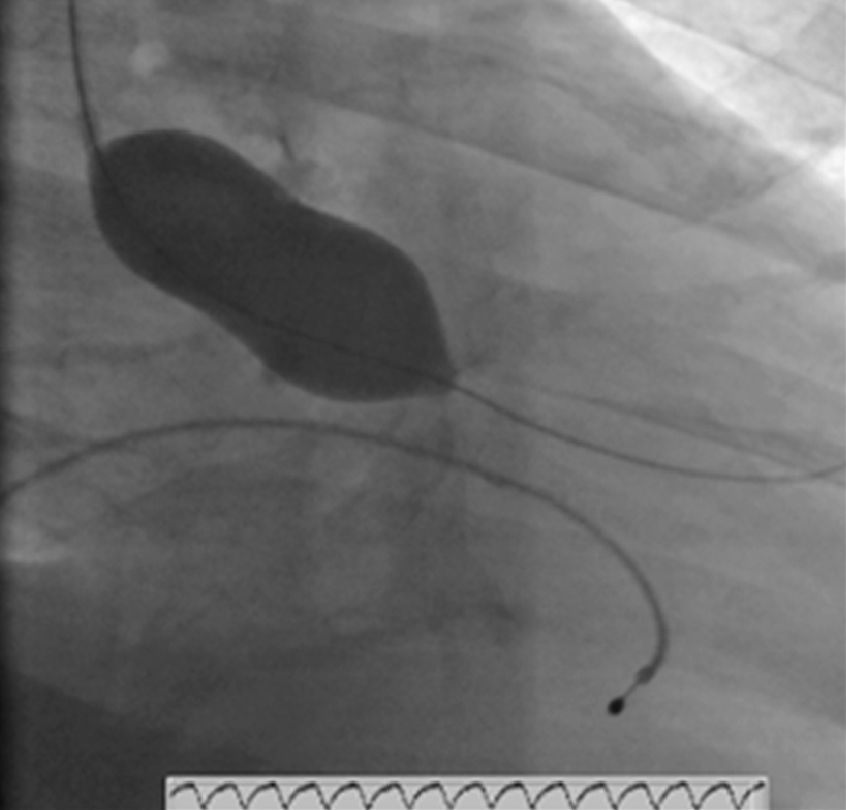
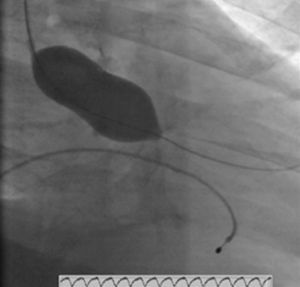
In view of the patient's hemodynamic instability with cardiogenic shock, aortic valvuloplasty was performed (Figure 3) with a 20-mm NuCLEUS balloon under pacing rhythm at 220 bpm, resulting in a reduction in aortic valve gradient from 97 mmHg to 46 mmHg. Complete myocardial revascularization was performed at the same time with two bare-metal stents. Aortography revealed moderate aortic regurgitation and so it was decided not to insert an intra-aortic balloon pump.
Progressive clinical improvement was seen, inotropic support being withdrawn after 48 hours and the patient being extubated after 72 hours. Peak troponin I was 144 ng/ml and progressively decreased; renal function gradually improved, with no significant fall in hemoglobin. Hospital stay was prolonged by nosocomial pneumonia caused by an unknown agent.
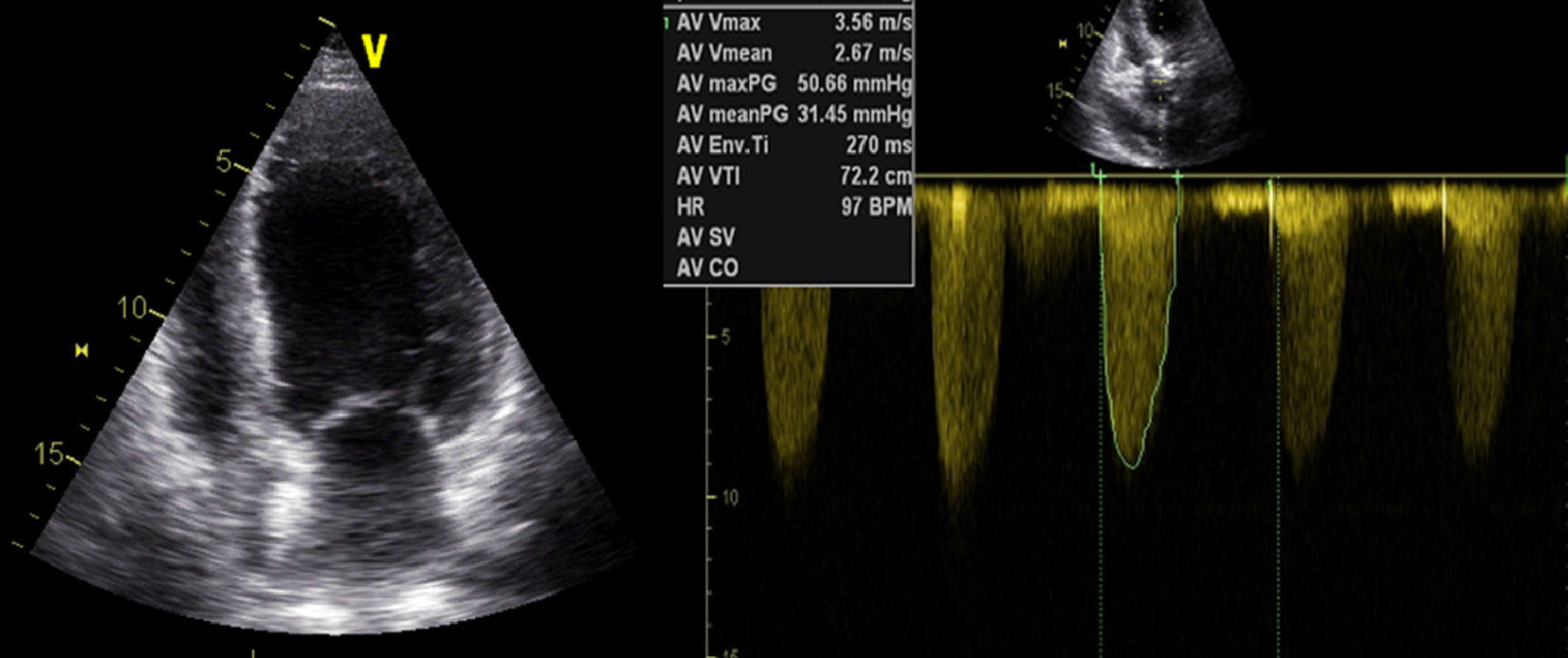
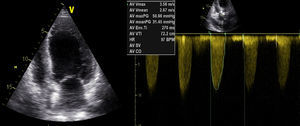
The patient was discharged on day 24 in NYHA class II. The discharge transthoracic echocardiogram showed moderate to severe global systolic dysfunction, mean aortic gradient of 31 mmHg and valve area of 1.06 cm2 (Figure 4). Cardiac surgery was scheduled following one month of dual antiplatelet therapy.
A month after discharge, the patient was readmitted to the emergency department with acute pulmonary edema, probably due to non-compliance with therapy. In the emergency room he suffered cardiopulmonary arrest with ventricular fibrillation but was resuscitated after 30 minutes of advanced life support. Cardiogenic shock was diagnosed and mechanical ventilation and vasopressor support with noradrenaline were begun. The ECG and echocardiogram were similar to those at discharge and peak troponin I was 10.4 ng/ml.
Noradrenaline was discontinued after less than 24 hours, but the patient's acute HF persisted, and various attempts at extubation were unsuccessful. On day 8 it was decided to administer levosimendan (maintenance dose of 0.1 μg/kg/min, without a loading dose). There were no complications and substantial clinical improvement was seen, the patient being extubated 24 hours later. Echocardiography showed improved LV function (ejection fraction 40%) and a mean aortic valve gradient of 47 mmHg.
Following clinical and hemodynamic stabilization, the patient was transferred to the cardiothoracic surgery department where he underwent aortic valve replacement with a Carpentier-Edwards biological prosthesis. The echocardiogram performed in the cardiothoracic surgery department revealed moderate global systolic dysfunction.
Three months after surgery, the patient was in NYHA class II with no anginal symptoms.
DiscussionAcute HF in the context of severe AS and severe global systolic dysfunction has a dire prognosis with limited therapeutic options and clinical evidence is sparse.
The case presented is noteworthy for the use of aortic balloon valvuloplasty and levosimendan.
PABV was developed in the 1980s as an alternative to surgical valve replacement.3 Despite initial enthusiasm, with increased valve area, reduced aortic valve gradient and improved LV function,9 long-term results were disappointing and many institutions abandoned the technique4 due to the significant complication rate (3% mortality and 25% hemodynamic or arrhythmic complications).9
The advent of percutaneous aortic valve implantation revived the role of PABV; there were also improvements in the balloons employed, which required smaller introducers and thus reduced vascular complications,10 and in the use of rapid ventricular pacing (180-220 bpm) with a temporary pacing electrode. Witzke et al.11 assessed the safety and efficacy of rapid ventricular pacing and showed that it enabled more precise and stable balloon placement, although at the cost of a smaller increase in valve area.
PABV is thus now used as a bridge to more permanent treatment (surgical or percutaneous valve replacement) or as a palliative measure in patients at high surgical risk or without access to or indication for percutaneous replacement.5
Hemodynamic instability is another indication for PABV, though with a low level of recommendation (class IIb) and evidence (C),2 and should only be considered as a last resort, due to its significant morbidity and mortality.5
In one of the largest series on PABV in patients with cardiogenic shock, by Moreno et al.5 (21 patients), in-hospital mortality was 43% (n=9): two during the procedure, two due to refractory HF and five due to comorbidities.
Buchwald et al.12 analyzed 14 patients treated by PABV for severe AS complicated by cardiogenic shock. In-hospital mortality was high (71%; n=10), but in multivariate analysis, only a delay of more than 48 hours between onset of shock and PABV was associated with a fatal outcome. All patients treated within 24 hours were alive at one-year follow-up, whether or not they had undergone surgical valve replacement.
In the case presented, the fact that the patient underwent PABV within 24 hours, resulting in a final valve area of around 1 cm2, may have contributed to the favorable outcome.
There are some reports in the literature suggesting that combined PABV and coronary angioplasty in patients who refuse surgery or are at high surgical risk may be safe and effective. McKay et al.13 described nine patients with single-vessel coronary disease and severe AS who underwent this combined procedure; seven of the nine showed clinical improvement at six months.
Patients with acute HF secondary to severe AS and LV dysfunction represent a challenge due to the need both to treat HF and to maintain perioperative stability. If not treated surgically, these patients’ prognosis is dismal, but intervention is associated with high morbidity and mortality.14
The case presented also raises the question of the ideal timing for valve replacement surgery after PABV in a patient with LV dysfunction. The standard approach is to proceed as soon as possible after the patient is clinically stable, but in this case (cardiogenic shock complicated by nosocomial pneumonia and moderate global systolic dysfunction), the decision was taken to postpone surgery for four weeks in light of the increased bleeding risk resulting from dual antiplatelet therapy.
Levosimendan is a calcium sensitizer that has both positive inotropic and vasodilatory effects without increasing myocardial oxygen consumption.6 Its beneficial effects in acute HF with global systolic dysfunction are well documented,15 but patients with severe AS are excluded from trials, since vasodilators are traditionally contraindicated in severe AS due to fears of hypotension. However, this idea has recently been challenged by studies showing that sodium nitroprusside is both safe and beneficial in patients with acute HF and severe AS with global systolic dysfunction8; this may be explained by its reduction of afterload, to which the left ventricle is particularly sensitive.
The little clinical evidence that exists on the use of levosimendan in this population16 consistently indicates that it is safe and effective, leading to clinical improvement, and that it is beneficial in high-risk patients preoperatively and postoperatively, improving global systolic function through recruitment of hibernating myocardium and thus promoting recovery.
The supposed benefit of levosimendan in patients with severe AS and global systolic dysfunction may be explained by its reduction of preload and afterload, together with improved coronary flow and cardiac function.15,17 In the presence of systolic dysfunction, the left ventricle is particularly sensitive to increased afterload, and so reduced peripheral vascular resistance may increase cardiac output without significantly lowering blood pressure.
Some studies have hypothesized, based on levosimendan's mechanism of action, that the drug could be used to assess contractile reserve in these patients, with a lower risk of myocardial ischemia than dobutamine.15
There is a similar lack of evidence concerning the use of levosimendan in the extubation of ventilator-dependent patients with LV dysfunction.18,19
Sterba et al.18 assessed 12 ventilator-dependent patients with global systolic dysfunction treated with 24-hour levosimendan perfusion; LV function and respiratory failure improved and seven of the 12 patients were then successfully extubated.
In a study of the hemodynamic effects of levosimendan and dobutamine in 10 ventilator-dependent patients with chronic obstructive pulmonary disease and increased ventricular filling pressures, Ouanes-Besbes et al.19 found that both drugs, but particularly levosimendan, reduced pulmonary capillary wedge pressure.
In the case presented, levosimendan was administered after several unsuccessful attempts at extubation in a patient with refractory HF. Its positive inotropic and vasodilatory effects may have contributed to successful extubation and improved global systolic function. No complications occurred during administration of the drug, including hypotension or complex ventricular arrhythmias.
ConclusionsThis case highlights the therapeutic challenge posed by patients with severe AS and coronary artery disease, particularly when accompanied by LV dysfunction. Percutaneous aortic balloon valvuloplasty and levosimendan were safe and effective as a bridge to surgery, the definitive treatment for such patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Caetano F, Almeida I, Seca L, et al. Estenose aórtica grave e choque cardiogénico: um desafio terapêutico. Rev Port Cardiol. 2013;32:701–706