We present the case of a 65-year-old male referred by an oncologist for transthoracic echocardiography because of effort dyspnea. His past medical history was remarkable for chronic obstructive pulmonary disease (COPD) and a gastric adenocarcinoma (pT2N1M0), resected three years previously and treated by adjuvant chemotherapy. Echocardiography revealed preserved biventricular ejection fraction, normal left ventricular diastolic indices, non-significant valvular dysfunction and no signs of pulmonary hypertension. However, a well-delimited 30 mm×23 mm×24 mm right ventricular (RV) ovoid, isoechogenic and homogeneous mass (Figure 1, asterisk) was observed along the basal free wall, in a sub-tricuspid position, well detached from the right coronary artery course (Figure 1, yellow arrow, and Videos 1 and 2).
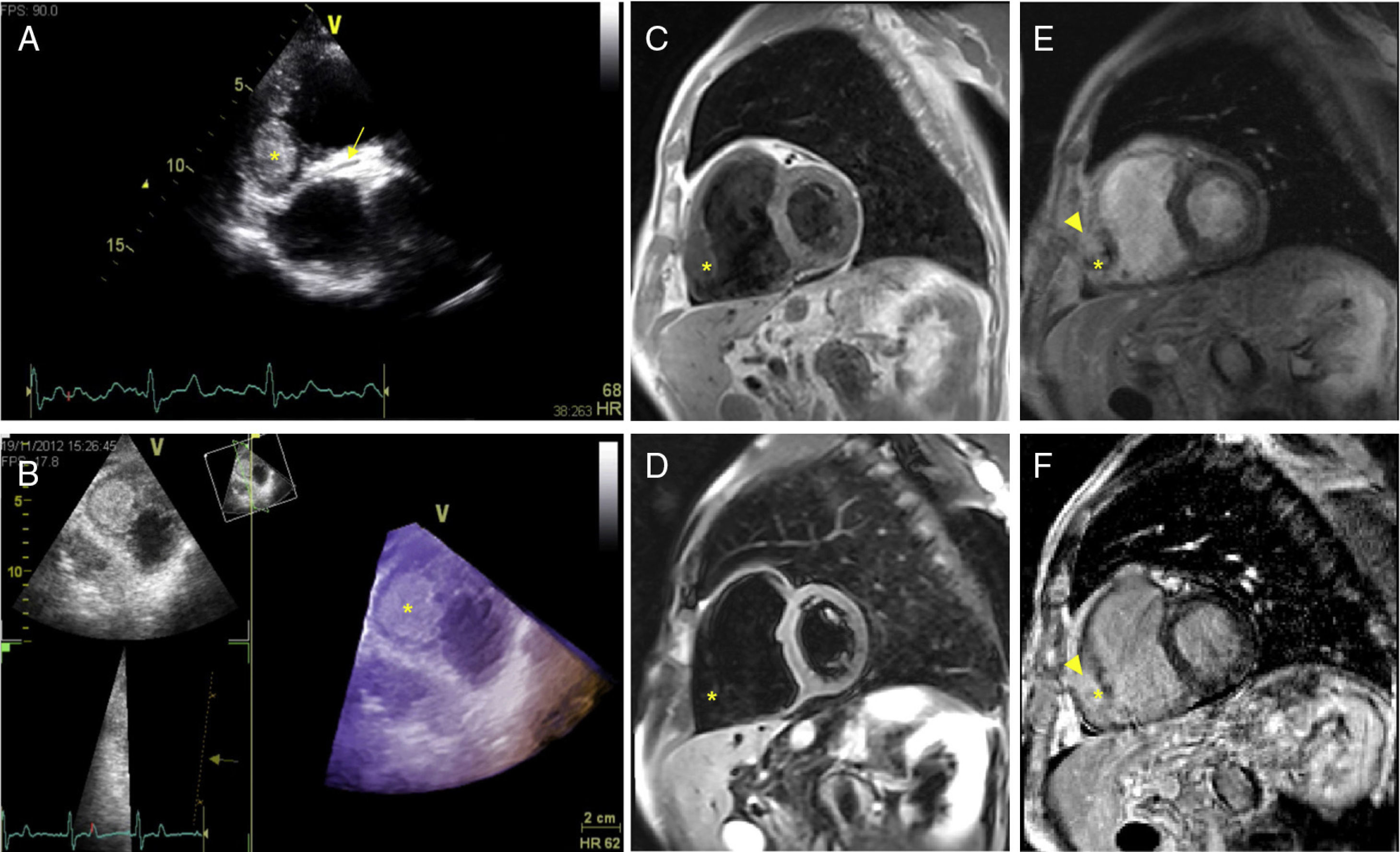
(A) Two-dimensional transthoracic echocardiography, modified short-axis view at the sub-tricuspid level, depicting a well-defined right ventricular mass (*) and part of the right coronary artery course along the atrioventricular groove (arrow); (B) three-dimensional (3D) transthoracic echocardiography, live 3D bird's eye view, modified 4-chamber view, showing a homogeneous and delimited ovoid mass (*) on a sub-tricuspid position; (C and D) mid-ventricular short-axis T1 and fat sat T2-weighted turbo spin-echo sequences, respectively, showing a hypointense homogeneous right ventricular mass (*) with no fat tissue; (E and F) mid-ventricular short-axis T1 post-contrast and phase-sensitive inversion recovery sequences, respectively, illustrating a small hyperintense core (arrowhead) inside the mass (*).
Cardiac magnetic resonance (CMR) allowed detailed tissue characterization. The mass was homogeneous and hypointense in both T1- (Figure 1C) and T2-weighted (Figure 1D) sequences, without fat tissue (Video 3). There was no detectable perfusion (Video 4) but a small core sign (Figure 1, arrowhead) was present on both T1 post-contrast (Figure 1E) and delayed enhancement (Figure 1F) acquisitions. No other abnormalities were noted, including pericardial or pleural effusions. In view of these findings, a benign cardiac mass was assumed. Repeated cardiac CMR at six and 12 months revealed similar findings.
Notwithstanding the previous clinical history, the CMR study excluded malignant primary or secondary etiologies for this mass, even suggesting an alternative process. During investigation, the patient confirmed the occurrence of a severe blunt chest trauma in a traffic accident 20 years before. Indeed, the non-specific tissue data were in accordance with an organized hematoma of the RV free wall. In this specific case, symptoms were attributed to COPD progression, as assessed by pulmonary function tests.
We found this case notable for the importance of CMR in the cardio-oncology setting. This tool provided biventricular functional assessment and excluded cardiac tumoral involvement, allowing confident risk stratification and conservative management. Furthermore, it led additional clinical investigation towards a definitive diagnosis of a very rarely reported cardiac condition.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Steady-state free precession cine cardiac magnetic resonance sequences, modified long-axis 4-chamber and short-axis views, showing an apparently encapsulated mass along the right ventricular (RV) trabeculae. This mass is slightly hypointense compared with the ventricular cavity, and shows a synchronous movement with the RV free wall.