Cardiac arrest (CA) is a complex event with a dismal survival rate. The aim of this study was to determine whether N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels measured on admission and serial cardiac troponin I determination in patients with in-hospital cardiac arrest (IHCA) are predictive of 30-day mortality.
MethodsOut of 9877 patients hospitalized in the cardiac intensive care unit during the study, we enrolled consecutive patients experiencing cardiac arrest within 12 hours of admission. Baseline characteristics, information about circumstances of CA and cardiopulmonary resuscitation, and initial biochemical parameters were retrospectively collected.
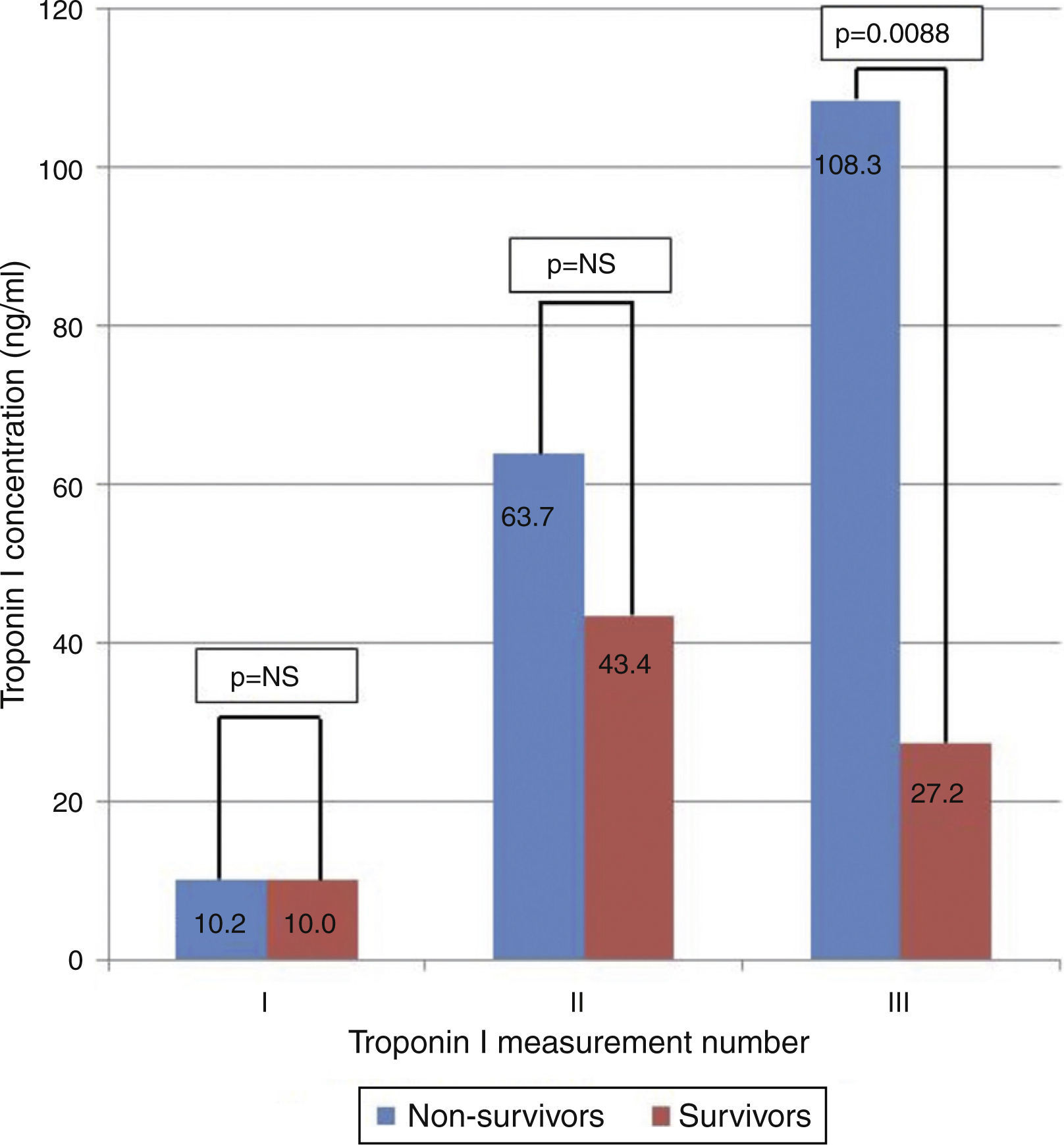
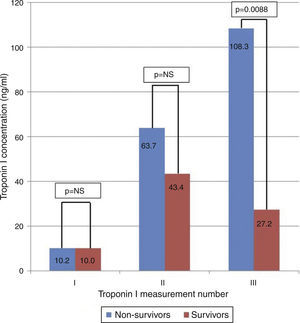
ResultsA total of 106 patients (61 male, age 71.4±12.6 years) were enrolled. Thirty-four (32.1%) had a history of myocardial infarction, and 13 (12.3%) a history of stroke. Total 30-day mortality was 60.4%. Deceased patients were older (73.7±11.9 vs. 67.8±13.0 years; p=0.01) and had lower systolic (89.4±37.0 vs. 115.0±24.0 mmHg; p=0.0001) and diastolic (53.6±24.8 vs. 66.1±15.0 mmHg; p=0.008) blood pressure on admission. Shockable initial rhythm was more often noted in the survivor group (54.8% vs. 28.1%; p=0.01). Deceased patients had higher median NT-proBNP levels (9590.0 [25–75% interquartile range (IQR), 5640.0–26450.0] vs. 3190.0 [25–75% IQR, 973.8–5362.5] pg/ml; p=0.02) on admission. There were no differences in the first two troponin I measurements, but values were higher on the third measurement in non-survivors (98.2 [25–75% IQR, 76.4–175.8] vs. 18.7 [25–75% IQR, 5.2–50.6]; p=0.009).
ConclusionsThe survival rate of patients after in-hospital CA is poor. Deceased patients have higher NT-proBNP levels on admission, along with higher troponin I concentrations on the third measurement. Those biomarkers are useful in predicting 30-day mortality in IHCA patients.
A paragem cardíaca (PC) é uma patologia complexa com uma taxa de sobrevivência distal. O objetivo deste estudo foi analisar se a concentração do terminal N do peptídeo natriurético auricular do tipo B (NT-proBNP), medida na admissão, e se a determinação de troponina I cardíaca seriada em doentes com paragem cardíaca intra-hospitalar são fatores preditivos para mortalidade a 30 dias.
MétodosDe 9877 doentes hospitalizados durante o estudo na unidade de cuidados intensivos, inscrevemos doentes consecutivos que passaram por paragem cardíaca nas primeiras 12 horas após o internamento. Foram inicialmente recolhidos características basais, informação sobre as circunstâncias da PC, ressuscitação cardiorrrespiratória e parâmetros bioquímicos iniciais.
ResultadosForam inscritos 106 doentes (61 homens, com 71,4±12,6 anos). Trinta e quatro (32,1%) doentes tinham antecedentes de enfarte do miocárdio e 13 (12,3%) antecedentes de acidente vascular cerebral. A mortalidade total a 30 dias foi de 60,4%. Os doentes falecidos tinham idade superior a (73,7±11,9 versus 67,8±13,0 anos; p=0,01), apresentavam pressão arterial sistólica mais baixa (89,4±37,0 versus 115,0±24,0 mmHg; p=0,0001) e diastólica (53,6±24,8 versus 66,1±15,0 mmHg; p=0,008) na altura do internamento. Um ritmo chocável inicial foi observado mais vezes no grupo dos sobreviventes (54,8% versus 28,1%; p=0,01). Os doentes falecidos apresentaram níveis medianos mais elevados do terminal N do peptídeo natriurético auricular do tipo B (NT-proBNP) [9590,0 (amplitude interquartílica 25–75% (IQR, 5640,0–26450,0) versus 3190,0 (IQR 25–75%, 973,8–5362,5) pg/ml; p=0,02] no internamento. Não se registaram diferenças nas duas primeiras medições de troponina I, com um valor mais elevado na terceira medição nos não sobreviventes [98,2 (IQR 25–75% (76,4–175,8) versus 18,7 (IQR 25–75%, 5,2–50,6); p=0,009].
ConclusõesA taxa de sobrevivência dos doentes após paragem cardíaca intra-hospitalar é fraca. Os doentes que faleceram apresentaram níveis mais elevados de NT-proBNP na admissão, juntamente com concentração mais elevada de troponina I na terceira medição. Aqueles biomarcadores são úteis na previsão da mortalidade a 30 dias nos doentes com paragem cardíaca intra-hospitalar.
confidence interval
cardiopulmonary resuscitation
in-hospital cardiac arrest
interquartile range
N-terminal pro-B-type natriuretic peptide
out-of-hospital cardiac arrest
receiver operating characteristic
standard deviation
Cardiovascular diseases are the leading cause of mortality and morbidity worldwide.1 Unfortunately, in many patients cardiac arrest is the first manifestation of cardiac disease.2 In spite of great improvements in health care, prognosis after cardiac arrest remains dismal and over the past 30 years there have been no dramatic changes in survival rates.3 Several factors have been shown to influence long-term prognosis of cardiac arrest patients: an initial shockable rhythm (ventricular tachycardia or ventricular fibrillation), cardiopulmonary resuscitation (CPR) initiated by bystanders, early defibrillation, and introduction of intensive treatment are associated with more favorable outcome.4,5 It thus seems intuitive that, due to easier and faster access to medical support and treatment, patients who experience in-hospital cardiac arrest (IHCA) will have better prognosis than those with out-of-hospital cardiac arrest (OHCA). Various biomarkers have been extensively studied in order to develop protocols for risk assessment in this group of patients. The aim of this study was to analyze the prognostic implications of N-terminal pro-B-type natriuretic peptide (NT-proBNP) measured on admission and serial cardiac troponin I determination in patients with IHCA.
MethodsStudy design, settings and selection of subjectsWe retrospectively analyzed data on consecutive patients admitted between January 2007 and July 2012 to the intensive cardiac care unit of a high-volume, tertiary university hospital who suffered cardiac arrest within 12 hours of admission to the hospital. Exclusion criteria were age <18 years, first cardiac arrest prior to or >12 hours after admission, and trauma-related cardiac arrest. Patients’ clinical data were collected by investigators via analysis of medical records. Following cardiac arrest all patients were managed in accordance with the applicable European Resuscitation Council guidelines.6,7 The collected data covered circumstances of cardiac arrest, patients’ baseline clinical characteristics (including comorbidities and cardiovascular risk factors), vital status on admission (including Glasgow Coma Scale score and laboratory tests results), treatment administered, and functional status on discharge. Biochemical parameters were assessed in blood samples taken on admission for initial troponin I and NT-proBNP levels and at the prespecified time intervals for serial troponin I measurement (the second 6–9 hours after admission, and the third 12–24 hours after admission). Troponin I was measured using an immunoassay (Abbott Laboratories, Illinois, USA), and NT-proBNP using quantitative assay (electrochemiluminescence; Roche Diagnostics GmbH, Mannheim, Germany). Patients were divided into two groups according to 30-day mortality. The follow-up on 30-day mortality was conducted using in-hospital records and data from the PESEL Polish population database. The study protocol was approved by the regional ethics committee.
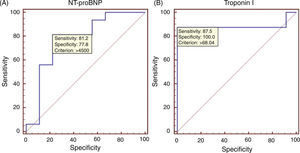
Statistical analysisContinuous data were tested for normal distribution using the Kolmogorov-Smirnov test. Variables displaying normal distribution were presented as mean ± standard deviation (SD) and compared using the Student's t test. Variables without normal distribution were presented as median and 25–75% interquartile range (IQR) and compared using the Mann-Whitney test. Categorical variables were compared using either the chi-square test or Fisher's exact test. A p value of less than 0.05 was considered statistically significant, with 95% confidence intervals (CI). Receiver operating characteristics (ROC) curves were constructed for the relation of troponin I and NT-proBNP with 30-day mortality. The area under the curve (AUC), or C-statistic, was used as a measure of the predictive accuracy of cardiac biomarkers. All analyses were performed using SAS statistical software, version 8.02 (SAS Institute Inc, Cary, NC, USA).
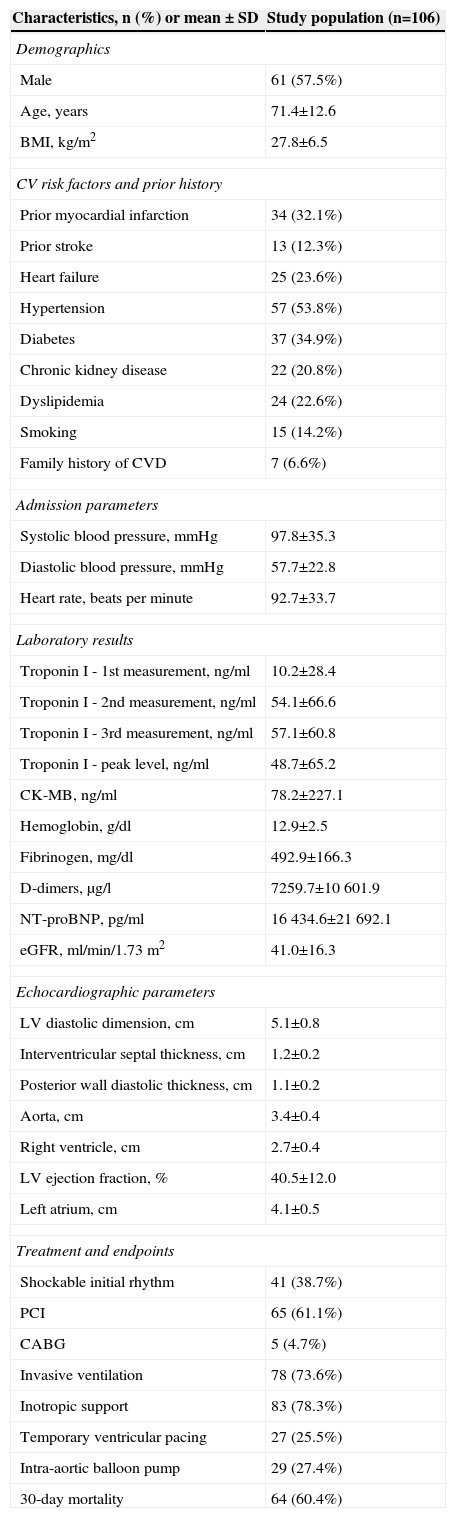
ResultsOut of 9877 patients hospitalized during the study enrollment period in the intensive cardiac care unit, 106 were included in the study (61 male, age 71.4±12.6 years) in accordance with the inclusion and exclusion criteria. Many patients had a history of major adverse cardiac events: 34 (32.1%) had a history of myocardial infarction and 13 (12.3%) of stroke (Table 1). In the majority of cases (87.7%) the primary diagnosis on admission was acute coronary syndrome; other primary diagnoses included cardiac arrhythmias (5.7%) and exacerbation of heart failure (6.6%). Mean systolic and diastolic blood pressure on admission were 97.8±35.3 and 57.7±22.8 mmHg, respectively. Median serum troponin I concentration on admission was 0.5 ng/ml (25–75% IQR, 0.1–5.3), the second measurement (6–9 hours after admission) was 24.0 ng/ml (25–75% IQR, 3.5–80.4), and the third (12–24 hours after admission) was 49.8 ng/ml (25–75% IQR, 8.3–80.0). Total all-cause 30-day mortality was 60.4%.
Baseline characteristics of the study group.
| Characteristics, n (%) or mean ± SD | Study population (n=106) |
|---|---|
| Demographics | |
| Male | 61 (57.5%) |
| Age, years | 71.4±12.6 |
| BMI, kg/m2 | 27.8±6.5 |
| CV risk factors and prior history | |
| Prior myocardial infarction | 34 (32.1%) |
| Prior stroke | 13 (12.3%) |
| Heart failure | 25 (23.6%) |
| Hypertension | 57 (53.8%) |
| Diabetes | 37 (34.9%) |
| Chronic kidney disease | 22 (20.8%) |
| Dyslipidemia | 24 (22.6%) |
| Smoking | 15 (14.2%) |
| Family history of CVD | 7 (6.6%) |
| Admission parameters | |
| Systolic blood pressure, mmHg | 97.8±35.3 |
| Diastolic blood pressure, mmHg | 57.7±22.8 |
| Heart rate, beats per minute | 92.7±33.7 |
| Laboratory results | |
| Troponin I - 1st measurement, ng/ml | 10.2±28.4 |
| Troponin I - 2nd measurement, ng/ml | 54.1±66.6 |
| Troponin I - 3rd measurement, ng/ml | 57.1±60.8 |
| Troponin I - peak level, ng/ml | 48.7±65.2 |
| CK-MB, ng/ml | 78.2±227.1 |
| Hemoglobin, g/dl | 12.9±2.5 |
| Fibrinogen, mg/dl | 492.9±166.3 |
| D-dimers, μg/l | 7259.7±10601.9 |
| NT-proBNP, pg/ml | 16434.6±21692.1 |
| eGFR, ml/min/1.73 m2 | 41.0±16.3 |
| Echocardiographic parameters | |
| LV diastolic dimension, cm | 5.1±0.8 |
| Interventricular septal thickness, cm | 1.2±0.2 |
| Posterior wall diastolic thickness, cm | 1.1±0.2 |
| Aorta, cm | 3.4±0.4 |
| Right ventricle, cm | 2.7±0.4 |
| LV ejection fraction, % | 40.5±12.0 |
| Left atrium, cm | 4.1±0.5 |
| Treatment and endpoints | |
| Shockable initial rhythm | 41 (38.7%) |
| PCI | 65 (61.1%) |
| CABG | 5 (4.7%) |
| Invasive ventilation | 78 (73.6%) |
| Inotropic support | 83 (78.3%) |
| Temporary ventricular pacing | 27 (25.5%) |
| Intra-aortic balloon pump | 29 (27.4%) |
| 30-day mortality | 64 (60.4%) |
BMI: body mass index; CABG: coronary artery bypass grafting; CK-MB: creatine kinase MB mass; CV: cardiovascular; CVD: cardiovascular disease; eGFR: estimated glomerular filtration rate; LV: left ventricular; NT-proBNP: N-terminal pro B-type natriuretic peptide; PCI: percutaneous coronary intervention.
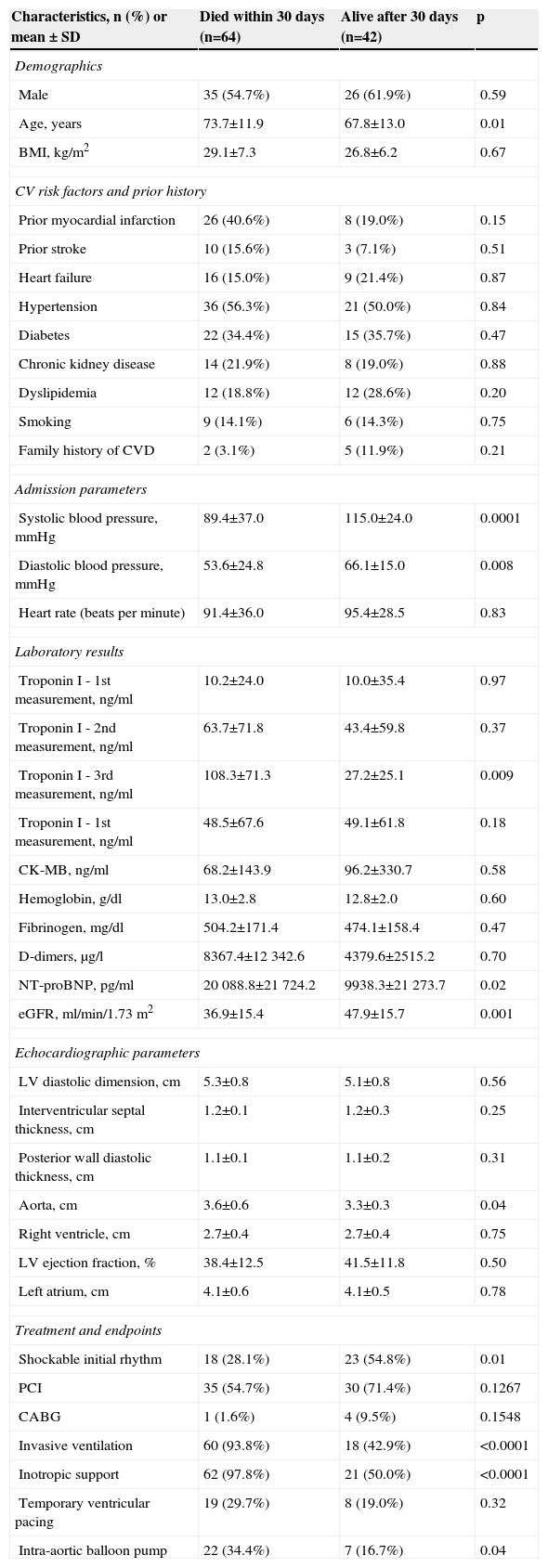
After dividing patients into survivors and non-survivors of the first 30-day period, we saw differences in baseline characteristics, clinical profile and outcome. There were 64 patients in the non-survivor group (60.4%) and 42 (39.6%) in the survivor group. Deceased patients were older (73.7±11.9 vs. 67.8±13.0 years; p=0.01) than survivors. They also had lower systolic (89.4±37.0 vs. 115.0±24.0 mmHg; p=0.0001) and diastolic (53.6±24.8 vs. 66.1±15.0 mmHg; p=0.008) blood pressure on admission. There were no differences between the groups concerning gender, body mass index, or history of hypertension, diabetes, myocardial infarction, or prior cardiac arrest (p>0.05). Concerning circumstances of cardiac arrest and applied treatment, significant differences were noted only in the prevalence of shockable initial rhythm (ventricular fibrillation/ventricular tachycardia), which was present less often in the deceased than in survivors (28.1% vs. 54.8%; p=0.01) (Table 2). The most common cause of cardiac arrest in this group was myocardial infarction (87 patients, 82.1%). Cardiac arrest was caused by heart failure in five patients (4.7%), electrolyte abnormalities in seven (6.6%), pulmonary embolism in two (1.9%), renal failure in two (1.9%), respiratory failure in two (1.9%), and aortic dissection in one (0.9%).
Comparison of the survivor and non-survivor groups.
| Characteristics, n (%) or mean ± SD | Died within 30 days (n=64) | Alive after 30 days (n=42) | p |
|---|---|---|---|
| Demographics | |||
| Male | 35 (54.7%) | 26 (61.9%) | 0.59 |
| Age, years | 73.7±11.9 | 67.8±13.0 | 0.01 |
| BMI, kg/m2 | 29.1±7.3 | 26.8±6.2 | 0.67 |
| CV risk factors and prior history | |||
| Prior myocardial infarction | 26 (40.6%) | 8 (19.0%) | 0.15 |
| Prior stroke | 10 (15.6%) | 3 (7.1%) | 0.51 |
| Heart failure | 16 (15.0%) | 9 (21.4%) | 0.87 |
| Hypertension | 36 (56.3%) | 21 (50.0%) | 0.84 |
| Diabetes | 22 (34.4%) | 15 (35.7%) | 0.47 |
| Chronic kidney disease | 14 (21.9%) | 8 (19.0%) | 0.88 |
| Dyslipidemia | 12 (18.8%) | 12 (28.6%) | 0.20 |
| Smoking | 9 (14.1%) | 6 (14.3%) | 0.75 |
| Family history of CVD | 2 (3.1%) | 5 (11.9%) | 0.21 |
| Admission parameters | |||
| Systolic blood pressure, mmHg | 89.4±37.0 | 115.0±24.0 | 0.0001 |
| Diastolic blood pressure, mmHg | 53.6±24.8 | 66.1±15.0 | 0.008 |
| Heart rate (beats per minute) | 91.4±36.0 | 95.4±28.5 | 0.83 |
| Laboratory results | |||
| Troponin I - 1st measurement, ng/ml | 10.2±24.0 | 10.0±35.4 | 0.97 |
| Troponin I - 2nd measurement, ng/ml | 63.7±71.8 | 43.4±59.8 | 0.37 |
| Troponin I - 3rd measurement, ng/ml | 108.3±71.3 | 27.2±25.1 | 0.009 |
| Troponin I - 1st measurement, ng/ml | 48.5±67.6 | 49.1±61.8 | 0.18 |
| CK-MB, ng/ml | 68.2±143.9 | 96.2±330.7 | 0.58 |
| Hemoglobin, g/dl | 13.0±2.8 | 12.8±2.0 | 0.60 |
| Fibrinogen, mg/dl | 504.2±171.4 | 474.1±158.4 | 0.47 |
| D-dimers, μg/l | 8367.4±12342.6 | 4379.6±2515.2 | 0.70 |
| NT-proBNP, pg/ml | 20 088.8±21724.2 | 9938.3±21273.7 | 0.02 |
| eGFR, ml/min/1.73 m2 | 36.9±15.4 | 47.9±15.7 | 0.001 |
| Echocardiographic parameters | |||
| LV diastolic dimension, cm | 5.3±0.8 | 5.1±0.8 | 0.56 |
| Interventricular septal thickness, cm | 1.2±0.1 | 1.2±0.3 | 0.25 |
| Posterior wall diastolic thickness, cm | 1.1±0.1 | 1.1±0.2 | 0.31 |
| Aorta, cm | 3.6±0.6 | 3.3±0.3 | 0.04 |
| Right ventricle, cm | 2.7±0.4 | 2.7±0.4 | 0.75 |
| LV ejection fraction, % | 38.4±12.5 | 41.5±11.8 | 0.50 |
| Left atrium, cm | 4.1±0.6 | 4.1±0.5 | 0.78 |
| Treatment and endpoints | |||
| Shockable initial rhythm | 18 (28.1%) | 23 (54.8%) | 0.01 |
| PCI | 35 (54.7%) | 30 (71.4%) | 0.1267 |
| CABG | 1 (1.6%) | 4 (9.5%) | 0.1548 |
| Invasive ventilation | 60 (93.8%) | 18 (42.9%) | <0.0001 |
| Inotropic support | 62 (97.8%) | 21 (50.0%) | <0.0001 |
| Temporary ventricular pacing | 19 (29.7%) | 8 (19.0%) | 0.32 |
| Intra-aortic balloon pump | 22 (34.4%) | 7 (16.7%) | 0.04 |
BMI: body mass index; CABG: coronary artery bypass grafting; CK-MB: creatine kinase MB mass; CV: cardiovascular; CVD: cardiovascular disease; eGFR: estimated glomerular filtration rate; LV: left ventricular; NT-proBNP: N-terminal pro B-type natriuretic peptide; PCI: percutaneous coronary intervention.
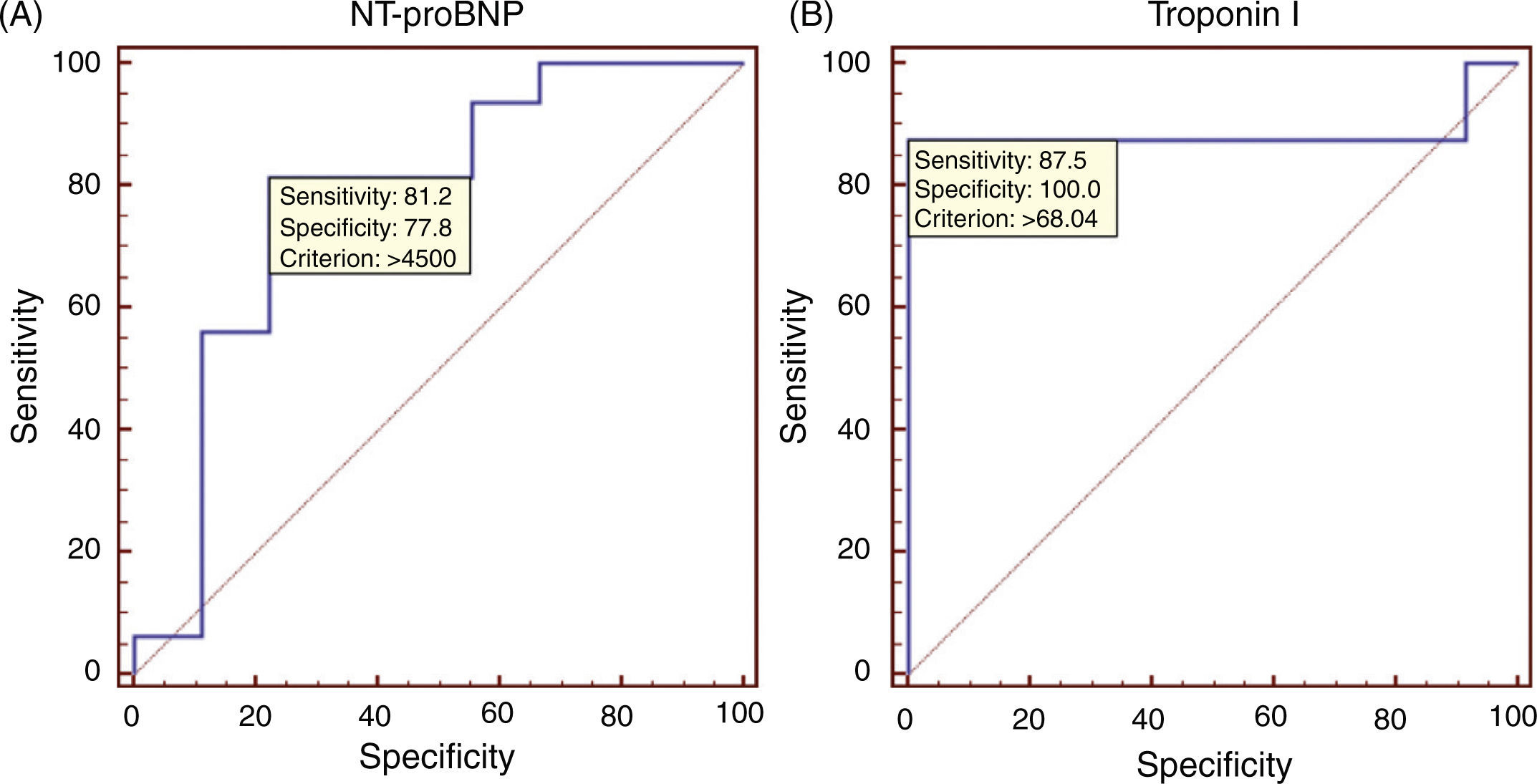
In admission laboratory results the median serum NT-proBNP level was higher (9590.0 [25–75% IQR, 5640.0–26450.0] vs. 3190.0 [25–75% IQR, 973.8–5362.5] pg/ml; p=0.02) and median estimated glomerular filtration rate (eGFR) was lower (36.0 [25–75% IQR, 25.0–49.5] vs. 55.5 [25–75% IQR, 41.5–60.0] ml/min/1.73 m2; p=0.001) in deceased patients compared to survivors. There were no statistical differences between the groups in the first two measurements of troponin I concentration (median 0.6 vs. 0.5 ng/ml; p=0.97, and 37.1 vs. 17.5 ng/ml; p=0.37, respectively). However, the third measurement showed an almost four-fold higher mean troponin I concentration in the deceased than the survivor group (98.2 [25–75% IQR, 76.4–175.8] vs. 18.7 [25–75% IQR, 5.2–50.6]; p=0.009) (Figure 1). The area under the ROC curve to predict 30-day mortality was 0.778 (95% CI, 0.57–0.92) for NT-proBNP concentration, and 0.885 (95% CI, 0.66–0.98) for the third troponin I measurement. The ROC curves for NT-proBNP and the third troponin I measurement are depicted in Figures 2A and 2B, respectively. Comparison of the two ROC curves showed no statistical difference (p>0.05).
Of the 30-day survivors, three additional patients died during prolonged hospitalization, and 39 (36.8%) were discharged alive. Mean hospital stay was 31.1±37.7 days.
DiscussionThe management of patients after cardiac arrest is still challenging in spite of constant advances in medicine. The majority of cardiac arrests are associated with conditions involving the heart muscle itself. Coronary artery abnormalities, myocarditis, and hypertrophic cardiomyopathy account for about 63% of cases of cardiac arrest.8 But not all cardiac arrests are actually of cardiac origin. It has been shown that in IHCA patients the immediate cause was cardiac in 39% of cases.9 Non-cardiac origins of cardiac arrest include hemorrhage, intracranial processes, lung disease, malignancy, intoxication, trauma, and suffocation. In this group survival to discharge is even lower than in patients with cardiac etiology.10 Whether the cause is cardiac or non-cardiac, what is important is the reversibility of the process. There is also little known about the long-term outcomes of survivors. There are some data on in-hospital and short-term mortality, but hardly any studies go beyond a one-year period.11 We present data from almost five years of observation of patients in a cardiac intensive care unit, so this trend is not surprising. However, this trend is constant even if data are collected from all emergency department patients.
Regardless of the cause, mortality rates and neurological prognosis remain poor.12 Development of optimal strategies for management of cardiac arrest patients is both important and extremely difficult, due to a variety of factors. During cardiac arrest saving human life is the priority, pushing scientific research into the background; large prospective studies to validate different CPR strategies are almost impossible to carry out due to ethical and other considerations.13 Furthermore, studies aiming to describe appropriate behavior models are required, but are rare.14
Applying even strictly specified CPR and other management techniques depends on initial diagnosis and appropriately categorizing the patient's status. As mentioned above, time is crucial at every step of the process, from initial diagnosis to administration of treatment, which is especially important in emergency departments.4,5 There is still a lack of simple, proven tools, scales or biomarkers which can predict short- and/or long-term survival and neurological outcome of cardiac arrest patients.15 It is still necessary to depend on clinical examination along with experience to decide on appropriate treatment. In this situation it is helpful to realize that cardiac arrest patients are a heterogeneous group whose initial characteristics influence outcome. Various biomarkers have been studied in the settings of cardiac arrest, but as the causes of cardiac arrest, primary myocardial infarction, may differ between patients, the same goes for the biomarker utility.16,17
In our study we examined only patients with cardiac arrest within 12 hours of admission. This specific criterion was applied to rule out patients with exacerbation of chronic critical disease, and to include the clinical characteristics of patients most often encountered in an emergency department. There were no significant differences in the baseline characteristics of the two groups, except for older age in the deceased group. Laboratory results showed that eGFR was significantly lower in deceased patients, which shows that they had worse renal function. Renal disease is known to increase the risk of cardiovascular disease; for example chronic kidney disease is now considered a coronary heart disease risk equivalent, placing patients at high risk for coronary events. Cardiac arrest risk is higher with every level of kidney disease, which is estimated to be a cause of about 60% of cardiovascular deaths.18
Another important clinical finding in our study were higher NT-proBNP levels in deceased patients. Baseline NT-proBNP concentration was previously shown to be predictive of sudden cardiac death in the general population.19 Another factor that our study showed to be predictive of outcome was troponin I level on the third measurement. Many patients have elevated troponin concentrations after cardiac arrest irrespective of its etiology.20 Nevertheless, elevated troponin concentration is predictive of myocardial damage, size of coronary artery thrombus, and death, as well as other acute conditions in this group of patients.21,22 In our study first measurements of troponin I concentration were similar in non-survivors and survivors. Then, in survivors there was a slight elevation in the second measurement, and a slow decrease in the third. However in non-survivors there was a constant rise through the second and third measurements (Figure 1), which may show that myocardial damage expanded rather than decreased.
Some studies show that prognosis in patients with IHCA is worse than in those experiencing OHCA. It has been shown that in-hospital presentation of life-threatening ventricular arrhythmias is associated with worse prognosis than out-of-hospital.22 The authors concluded that this may be due to greater burdens of concomitant disease in the in-hospital group. These findings may also apply to our study, but other possible explanations may include greater disease severity causing cardiac arrest. We may suspect that the overall clinical state of IHCA patients is generally worse than in OHCA. First of all, their cardiac arrest took place when they were already admitted and were thus under medical supervision and receiving pharmacological and other treatment. Although all the IHCA took place in the presence of medical personnel, and in the majority there was no delay in administering CPR, it was still associated with poor prognosis in our study, as in others.23,24 A shockable initial rhythm, defined as ventricular fibrillation or ventricular tachycardia as the first cardiac arrest rhythm, is associated with better outcome. As may be predicted, a shockable initial rhythm was more often present in survivors than the deceased group. There were differences in management concerning the use of an intra-aortic balloon pump (IABP), which was more often applied in IHCA patients. The small number of participants in our study does not provide sufficient data to draw conclusions about the efficacy of IABP treatment. Nevertheless its efficacy in improving survival in, for example, cardiogenic shock has recently been questioned.25 In our study different rates of IABP use are rather a reflection of the worse clinical status of IHCA patients.
The present study has certain limitations. Firstly, the patients enrolled were hospitalized only in the intensive care unit of a cardiology department, and so the results presented may not be applicable to the whole population of IHCA patients. Secondly, for more accurate results the study population should have been larger. We are also unable to provide an explanation why NT-proBNP and troponin I levels were elevated in the study patients. It is probably due to many reasons, including CPR and in many cases acute coronary syndrome. The relationship of troponin levels and echocardiographic findings in the present study also cannot be objectively analyzed, because many patients had a previous history of myocardial infarction or coronary artery disease, therefore without previous medical records we are unable to confirm whether impaired contractility or reduced ejection fraction were related to the current hospitalization.
ConclusionsPatients with in-hospital cardiac arrest have poor short-term prognosis; the short-term survival rate of patients after IHCA within 12 hours of hospitalization is 39.6%. Deceased patients have higher NT-proBNP levels on admission, along with higher troponin I concentrations on the third measurement. The above-mentioned biomarkers are useful in predicting 30-day mortality in IHCA patients, and may be valuable in planning treatment strategies in this group of patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.