To evaluate the performance of traditional cardiovascular (CV) risk factors in identifying a higher than expected coronary atherosclerotic burden.
MethodsWe assessed 2069 patients undergoing coronary CT angiography, with assessment of calcium score (CS), for suspected coronary artery disease. A higher than expected atherosclerotic burden was defined as CS >75th percentile (CS >P75) according to age and gender-adjusted monograms. The ability of traditional CV risk factors to predict a CS >P75 was assessed in a customized logistic regression model (“Clinical Score”) and by the calculation of SCORE (Systemic Coronary Risk Evaluation). The population attributable risk (PAR) of risk factors for CS >P75 was calculated.
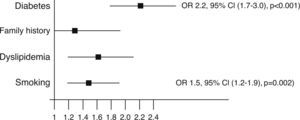
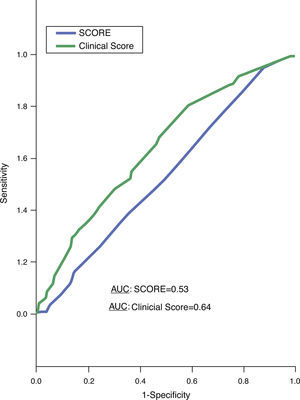
ResultsThe median CS was 3.0 (IQR 0.0–98.0); 362 patients had CS >P75. The median SCORE was 3.0 (IQR 1.0–4.0). With the exception of hypertension, all traditional CV risk factors were independent predictors of CS >P75: diabetes, dyslipidemia, smoking and family history (OR 1.3–2.2, p≤0.026). The areas under the ROC curves for CS >P75 were 0.64 for the Clinical Score (95% CI 0.61–0.67, p<0.001) and 0.53 for SCORE (95% CI 0.50–0.56, p=0.088). About a quarter of patients with CS >P75 were in the two lower quartiles of the Clinical Score. Altogether, the traditional risk factors explain 56% of the prevalence of CS >P75 (adjusted PAR 0.56).
ConclusionDespite the association of CV risk factors with a higher than expected atherosclerotic burden, they appear to explain only half of its prevalence. Even when integrated in scores, the predictive power of these risk factors was modest, exposing the limitations of risk stratification based solely on demographic and clinical risk factors.
O objetivo deste trabalho foi avaliar o desempenho dos fatores de risco cardiovascular (CV) clássicos na identificação de carga aterosclerótica superior ao esperado.
MétodosAvaliámos 2069 doentes (dts) que realizaram AngioTC cardíaca e ScCa para exclusão de doença coronária. Definiu-se carga aterosclerótica superior ao esperado um ScCa acima do percentil 75 (ScCa>p75) de acordo com nomogramas ajustados para o sexo e idade. A capacidade dos fatores de risco clássicos preverem ScCa>p75 avaliou-se num modelo de regressão logística customizado (score clínico) e pelo SCORE. Avaliou-se o Population Attributable Risk (PAR) dos fatores de risco para ScCa>p75.
ResultadosA mediana de ScCa foi 3,0 [IIQ 0,0-98,0]; 362 dts com ScCa>p75. A mediana do HeartScore foi 3,0 [IIQ 1,0-4,0]. Exceto a hipertensão arterial, todos os fatores de risco foram preditores independentes de CaSc>p75: diabetes mellitus, dislipidemia, tabagismo e história familiar (OR 1,3-2,2, p≤0,026). As áreas abaixo da curva ROC para SaCa>p75 foram 0,64 para score clínico (IC95% 0,61-0,67; p<0,001) e 0,53 para SCORE (IC95% 0,50-0,56, p=0,088). Um quarto dos dts com CaSc>p75 encontravam-se nos dois quartis de score clínico mais baixos. No seu conjunto, os fatores de risco clássicos explicam 56% da prevalência de ScCa>p75 (PAR ajustado 0,56).
ConclusãoApesar de os fatores de risco CV se associarem a uma carga aterosclerótica superior ao esperado, justificam pouco mais de metade da sua prevalência. O poder preditor destes fatores de risco é modesto, mesmo integrados em scores, revelando as limitações da estratificação de risco baseada apenas em dados demográficos e fatores de risco clínicos.
Coronary artery disease (CAD) remains the single most frequent cause of premature mortality worldwide, reaching epidemic proportions.1 Primary prevention measures have had a favorable effect on the prognosis of patients with CAD. Estimation of total cardiovascular (CV) risk is a cornerstone of the assessment of patients with suspected CAD, enabling adjustment of the intensity of preventive and therapeutic measures.2 Risk scores that reflect the interaction of multiple CV risk factors are available for this purpose and are frequently used in clinical practice.
Although modifiable CV risk factors account for most of the risk of myocardial infarction (MI), risk prediction based on scores including only demographic and clinical characteristics have some limitations.3 The MONICA project4 showed that only part of the variation in the time trends of coronary event rates could be predicted by trends in risk factors. In fact, CV risk can be higher than indicated by the charts in several settings, for example in asymptomatic individuals with preclinical evidence of atherosclerosis, such as the presence of calcified coronary plaques.
The extent of coronary calcification correlates with total coronary plaque burden, and has a high negative predictive value for ruling out the presence of significant coronary stenosis.5,6 Additionally, the calcium score (CS) also has a prognostic impact, as it can show increased risk of MI.7,8 In previous studies, the CS was a predictor for premature CAD independently of traditional clinical CV risk factors, and combining the two appears to change the predicted risk to an extent that may be clinically important, helping to decide how aggressively primary prevention strategies should be implemented.9,10
The aim of the present study was to assess the performance of the traditional CV risk factors, alone or associated in scores, in identifying a higher than expected coronary atherosclerotic burden.
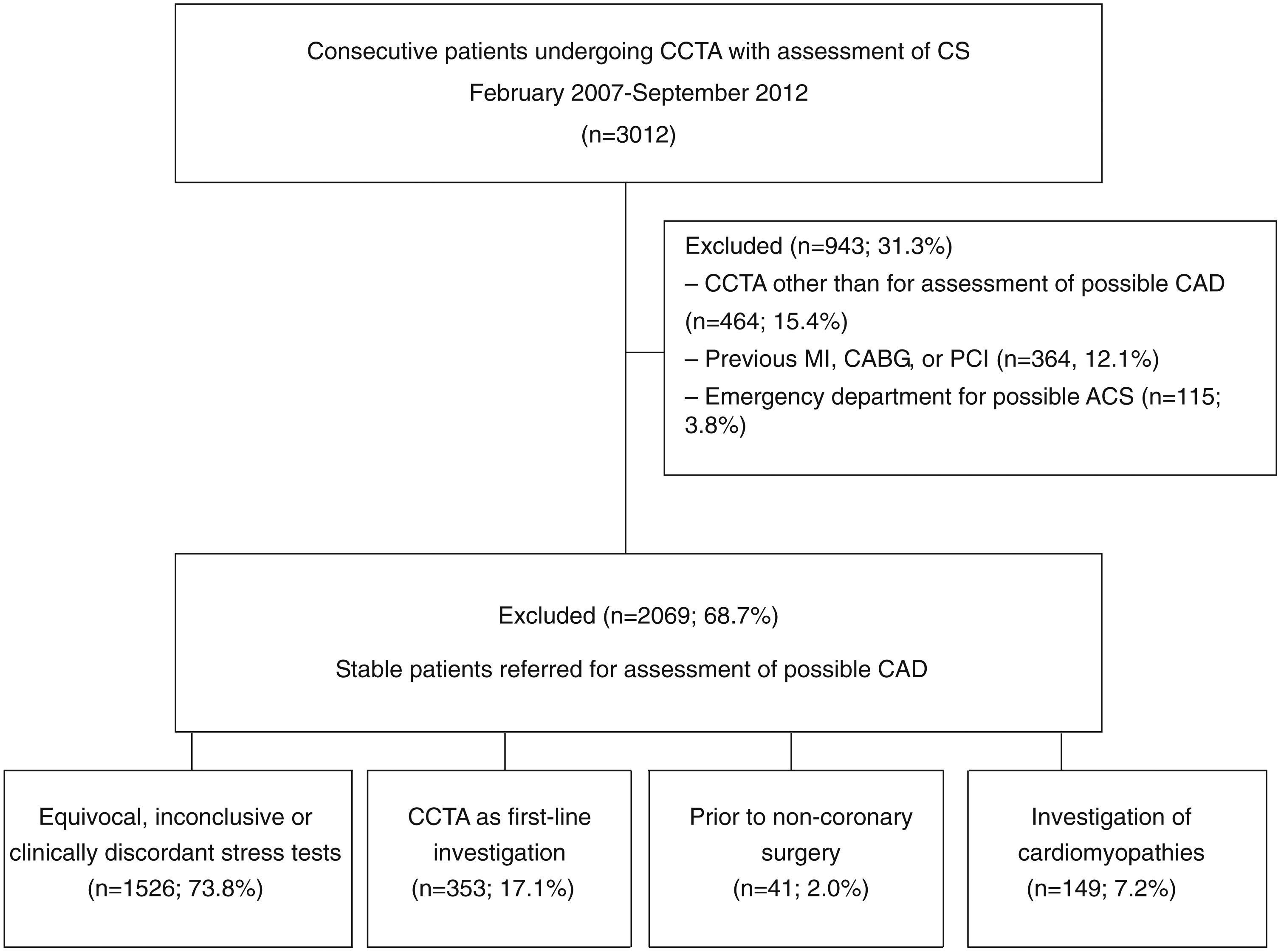
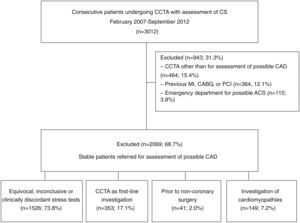
MethodsStudy design and populationBetween February 2007 and September 2012, 3012 consecutive patients undergoing coronary computed tomography angiography (CCTA) for assessment of possible CAD were prospectively enrolled in a single-center registry. Patients referred from the emergency department for possible acute coronary syndrome, those with indications other than assessment for possible CAD, and those without CS assessment were excluded from the present analysis. For the purpose of this study, 2069 patients were included, the majority of them (1526, 73.8%) assessed in the context of previous stress tests that were equivocal, inconclusive or clinically discordant with clinical assessment, while 353 (17.1%) were undergoing first-line investigation of possible CAD. Other exams were performed to investigate possible CAD in patients with cardiomyopathies (149, 7.2%) and for preoperative assessment of CAD prior to non-coronary surgery (41, 2.0%). Patient selection and study design are depicted in Figure 1.
Cardiovascular risk assessmentA detailed medical history, including a CV risk factor questionnaire, was obtained from all patients to assess the presence of: (1) diabetes (defined as fasting plasma glucose ≥7.0 mmol/l or use of oral hypoglycemic agents or insulin); (2) dyslipidemia (defined as total cholesterol ≥5 mmol/l or treatment with lipid-lowering drugs); (3) hypertension (defined as blood pressure ≥140/90 mmHg or the use of antihypertensive medication); (4) family history of premature CAD (defined as the presence of CAD in first-degree relatives younger than 55 [male] or 65 [female] years); and (5) smoking (defined as previous, less than one year, or current smoker).
CV risk was assessed for the overall population using the SCORE (Systemic Coronary Risk Evaluation) system,2 which estimates the 10-year risk of CV death and is determined by the interaction of various clinical risk factors (gender, age, smoking status, blood pressure and total cholesterol). As recommended in the European guidelines on cardiovascular disease prevention2 for stratification of the Portuguese population, we used the chart for low-risk countries. The local ethics committee approved the study and all patients gave their written informed consent.
Scan protocol, image reconstruction and calcium score assessmentScans were performed with a dual-source scanner (SOMATOM Definition®, Siemens Medical Systems, Germany), with the patient in dorsal decubitus and in deep inspiration breath-hold. All patients received sublingual nitroglycerin except when contraindicated, and beta-blockers were administered to lower heart rate when indicated. During the scan acquisition, a bolus of iodinated contrast (Visipaque®, GE Healthcare, USA) was infused at 6 ml/s, followed by a 50-ml saline flush. The contrast dose was calculated according to the following formula: (acquisition time+6 s delay)×flow (6 ml/s). Contrast administration was timed to optimize uniform enhancement of the coronary arteries. Dose reduction strategies – including ECG-gated tube current modulation, reduced tube voltage, and prospective axial triggering – were used whenever feasible. Mean estimated radiation dose was 5.1±3.9 mSv and the contrast dose was 97.0±14.0 ml. Mean heart rate was 67.3±12.7 bpm; 197 (9.5%) patients received beta-blocker therapy before acquisition. Transaxial images were reconstructed with a temporal resolution of 83 ms and slice thickness of 0.75 mm with 0.4 mm increments. Post-processing was carried out using Circulation® software, with multiplanar reconstructions, maximum intensity projection and volume rendering. All scans were analyzed in the same session by both a cardiologist and a radiologist with level III-equivalent experience. The CS was calculated by summing the number of coronary segments with calcium. A higher than expected atherosclerotic burden was defined as a CS above the 75th percentile (CS >P75) according to age- and gender-adjusted monograms.
Statistical analysisContinuous variables with normal distribution were expressed as means and standard deviation (SD) and those with non-normal distribution as medians and interquartile range (IQR). Normality was tested with the Kolmogorov-Smirnov test. Categorical variables were expressed as frequencies and percentages. Statistical comparisons were performed using the chi-square test or Fisher's exact test, as appropriate, for categorical variables and the Mann-Whitney or Kruskal-Wallis tests for continuous variables. The ability of traditional CV risk factors to predict a CS >P75 was assessed in a customized logistic regression model (“Clinical Score”) and by calculating SCORE. Areas under the receiver operating characteristic (ROC) curves of both the Clinical Score and SCORE for prediction of CS >P75 were determined. Additionally, the population attributable risk (PAR) of the various clinical risk factors for a higher than expected atherosclerotic burden was calculated. Two-tailed tests of significance are reported. For all the comparisons, a p value <0.05 was considered statistically significant. When appropriate, 95% confidence intervals (CI) were calculated. The statistical analysis was performed with SPSS version 21.0 (SPSS® Inc., Chicago, IL, USA).
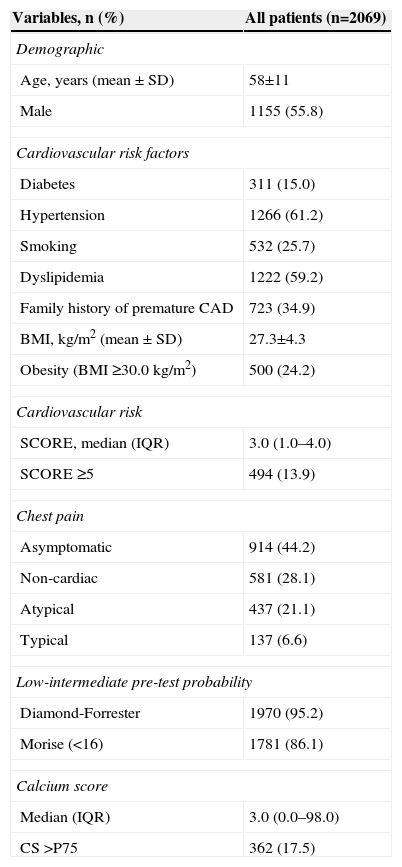
ResultsBaseline population characteristicsDemographic and clinical characteristics are depicted in Table 1. Briefly, the mean age of the 2069 patients studied was 58±11 years and 55.8% were male. Almost two-thirds (65.9%) of the patients had more than one CV risk factor, the most prevalent being hypertension (61.2%), followed by dyslipidemia (59.2%), family history of premature CAD (34.9%), smoking (25.7%) and diabetes (15.0%). Mean body mass index (BMI) was 27.3±4.3 kg/m2; 24.2% patients were obese (BMI ≥30.0 kg/m2). The median SCORE was 3.0 (IQR 1.0–4.0); 13.9% patients had high/very high CV risk (SCORE ≥5). Regarding clinical presentation, 44.2% patients were asymptomatic, only 6.6% reporting typical chest pain. The majority of the population had a low-intermediate pre-test probability of CAD as assessed by the Diamond-Forrester and Morise scores (95.2% and 86.1%, respectively). The median CS was 3.0 (IQR 0.0–98.0), with 362 patients (17.5%) having CS >P75.
Demographic and clinical characteristics of the study population.
| Variables, n (%) | All patients (n=2069) |
|---|---|
| Demographic | |
| Age, years (mean ± SD) | 58±11 |
| Male | 1155 (55.8) |
| Cardiovascular risk factors | |
| Diabetes | 311 (15.0) |
| Hypertension | 1266 (61.2) |
| Smoking | 532 (25.7) |
| Dyslipidemia | 1222 (59.2) |
| Family history of premature CAD | 723 (34.9) |
| BMI, kg/m2 (mean ± SD) | 27.3±4.3 |
| Obesity (BMI ≥30.0 kg/m2) | 500 (24.2) |
| Cardiovascular risk | |
| SCORE, median (IQR) | 3.0 (1.0–4.0) |
| SCORE ≥5 | 494 (13.9) |
| Chest pain | |
| Asymptomatic | 914 (44.2) |
| Non-cardiac | 581 (28.1) |
| Atypical | 437 (21.1) |
| Typical | 137 (6.6) |
| Low-intermediate pre-test probability | |
| Diamond-Forrester | 1970 (95.2) |
| Morise (<16) | 1781 (86.1) |
| Calcium score | |
| Median (IQR) | 3.0 (0.0–98.0) |
| CS >P75 | 362 (17.5) |
BMI: body mass index; CAD: coronary artery disease; CS: calcium score; CV: cardiovascular; IQR: interquartile range; P75: 75th percentile; SD: standard deviation.
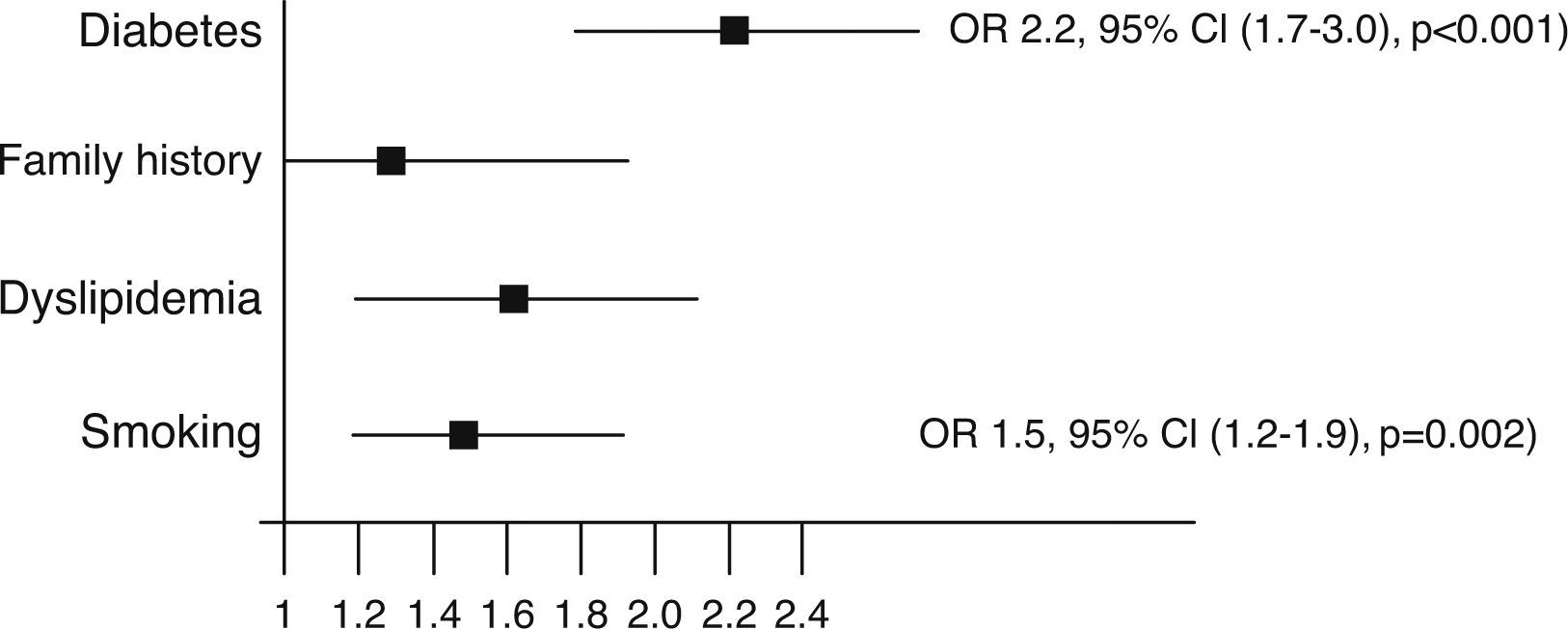
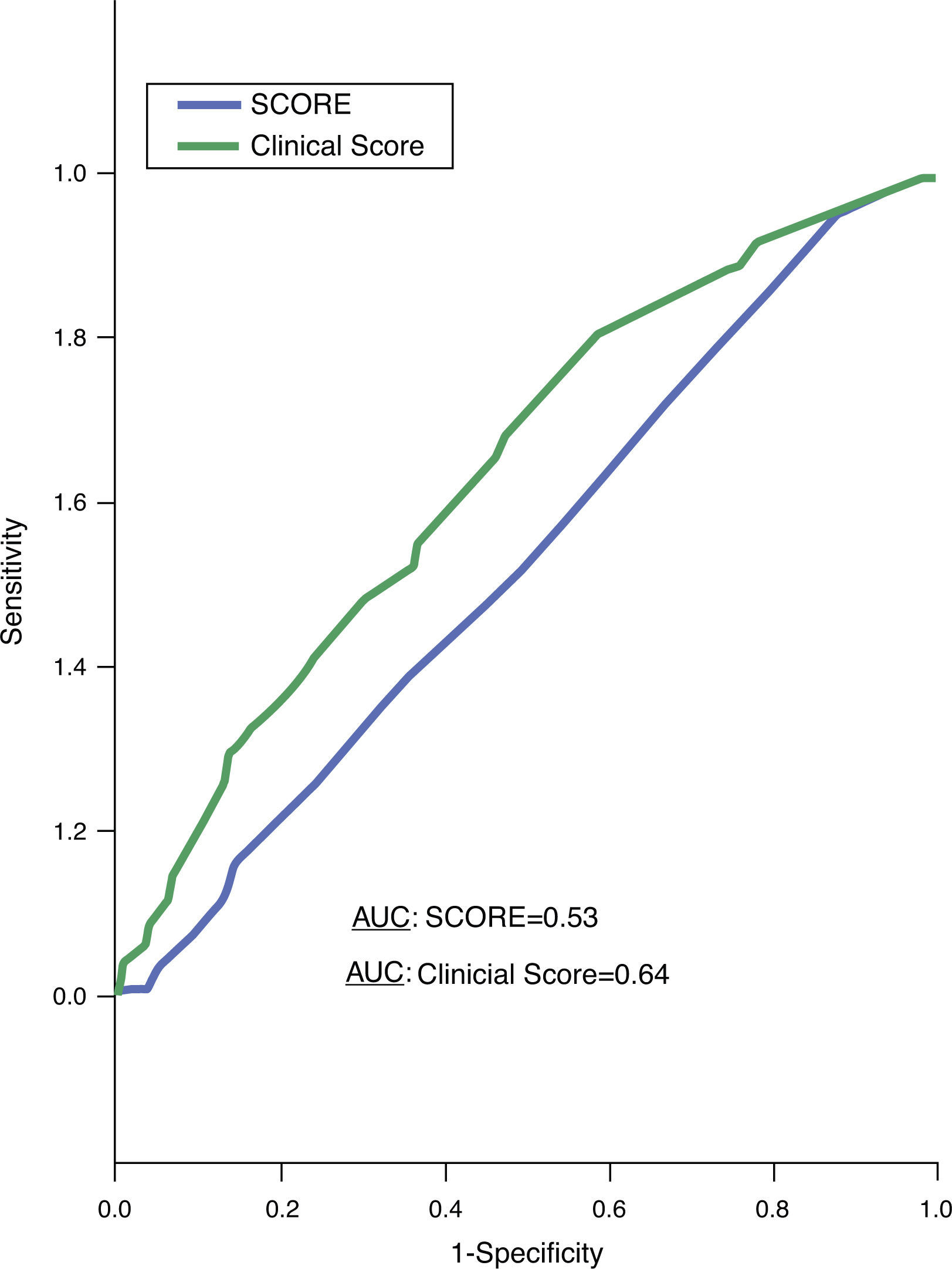
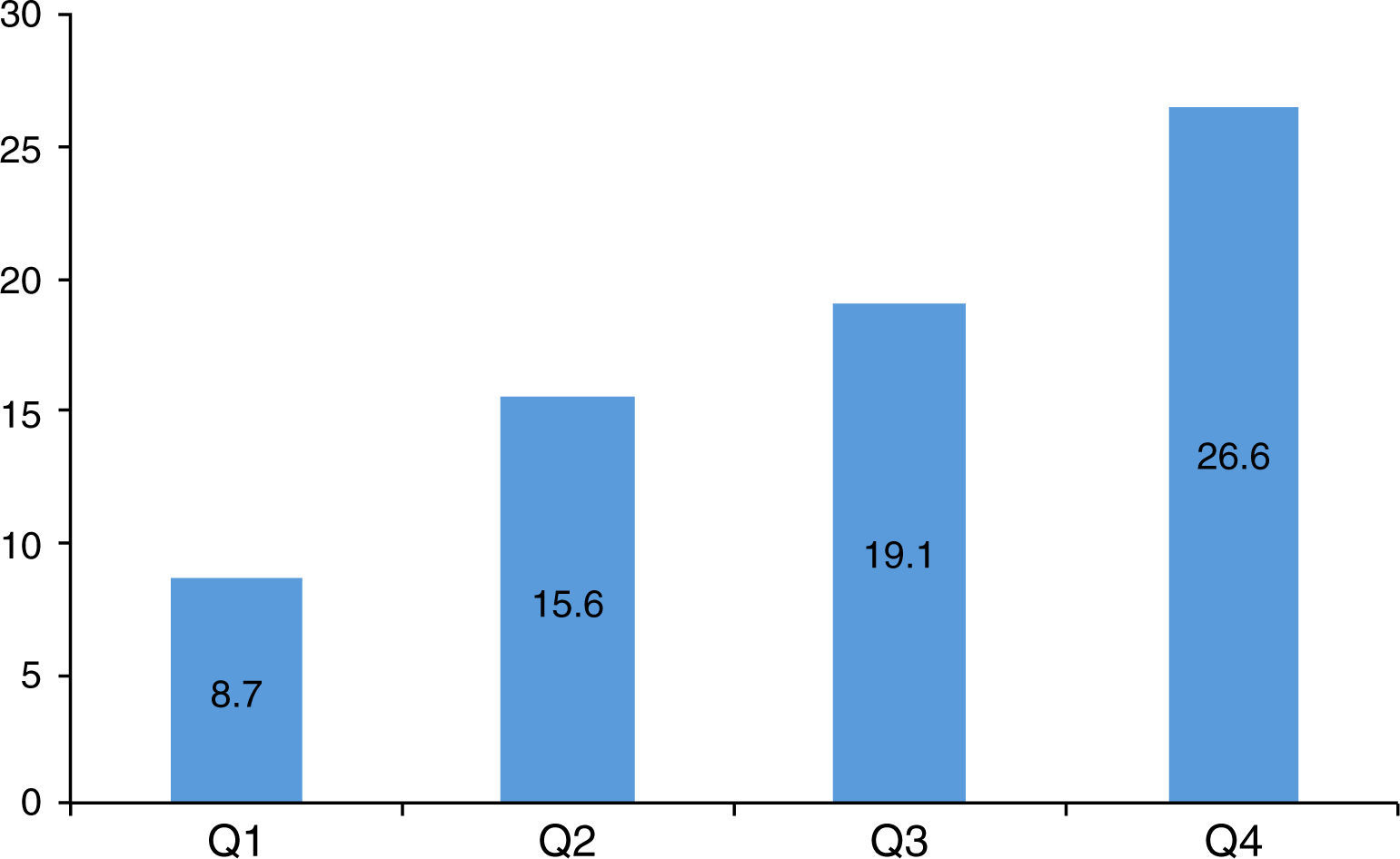
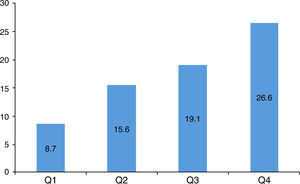
With the exception of hypertension, all the traditional CV risk factors – diabetes, dyslipidemia, smoking and family history of CAD – were independent predictors of CS >P75, all odds ratio (OR) 1.3–2.2, p≤0.026 (Figure 2). The predictive power of both Clinical Score and SCORE for the presence of CS >P75, as assessed by ROC curves, was low (Figure 3): area under the curve (AUC) 0.64 for the Clinical Score (95% CI 0.61–0.67, p<0.001) and 0.53 for SCORE (95% CI 0.50–0.56, p=0.088). Analyzing the population by quartile of the Clinical Score, a quarter of patients with CS >P75 (24.3%) were in the two lower quartiles (Figure 4). Altogether, the traditional CV risk factors analyzed (hypertension, dyslipidemia, smoking, diabetes and family history of premature CAD, and obesity) explain only 56% of the prevalence of CS >P75 (adjusted PAR 0.56).
The present study shows that despite the association between traditional CV risk factors and a higher than expected atherosclerotic burden, as defined by a CS above the 75th percentile according to age and gender-adjusted monograms, these risk factors appear to explain only 56% of its prevalence. Even when integrated in scores, the predictive power of these traditional CV risk factors was relatively modest, exposing the limitations of risk stratification based solely on demographic and clinical risk factors.
The association of traditional risk factors in scores has emerged as a central step in the stratification of CV risk and subsequent implementation of preventive actions. Several risk assessment algorithms, such as those derived from the Framingham Heart Study in the USA or from the Prospective Cardiovascular Münster (PROCAM) study in Germany, and SCORE, are available for estimating multifactorial absolute risk in clinical practice. In the European guidelines on cardiovascular disease prevention,2 determination of SCORE is recommended in asymptomatic adults without evidence of CV disease, since risk stratification is an important measure, even in asymptomatic individuals. Sudden cardiac death or acute MI can be the first manifestation of coronary atherosclerosis, highlighting the importance of prevention. However, the identification of asymptomatic individuals with higher risk for CV events remains challenging.
Although several studies and registries, such as the landmark INTERHEART study,3 show that traditional CV risk factors account for most of the risk of MI, risk prediction based only on demographic and clinical factors appears to have limitations. In a population of more than 120000 patients enrolled in 14 international randomized clinical trials of coronary heart disease and presenting with acute coronary syndrome or undergoing percutaneous coronary intervention, Khot et al.11 showed that 58% had none or one of the CV risk factors diabetes, dyslipidemia, smoking and hypertension. Additionally, another analysis by Akosah et al.12 in a population of young adults with first acute MI showed that only 25% met criteria to qualify for pharmacotherapy. Even in the presence of established clinical CV risk factors, a significant number of coronary events are unpredictable.
The limitations of risk scores based on clinical characteristics highlights the potential utility of direct imaging modalities, such as CCTA, for accurate identification of the presence and extent of coronary atherosclerosis. In this context, CS has emerged as a feasible and easy method for assessment of the presence of CAD. A high CS is indicative of advanced atherosclerotic lesions as identified by histological criteria as fibroatheroma14; although it cannot localize lesions that are stenotic or at risk of rupture, it may be able to determine the total coronary atherosclerotic disease burden, and is linearly correlated with the occurrence of hard clinical events.15,16 Although the absolute prevalence of severely stenotic plaques may be higher than that of mildly stenotic plaques, there are more plaques with mild than with severe stenosis. Data from the PROSPECT study17 show that in patients presenting with acute coronary syndrome and undergoing percutaneous coronary intervention, major adverse CV events during follow-up were equally attributable to recurrence at the site of culprit lesions and to nonculprit, frequently angiographically mild, lesions. The CONFIRM registry18 showed that both obstructive and nonobstructive plaques are associated with higher mortality, with risk profiles differing for age and gender, and the absence of CAD is associated with a favorable prognosis. An interesting finding was that more than two-thirds of patients did not have obstructive disease, and when compared in survival analysis, the prognosis of patients with nonobstructive stenosis was closer to that of those with significant single-vessel disease than that of those with no coronary plaques. In this context, even with low values, determination of CS may help in deciding how aggressive primary prevention strategies should be.
The relationship between CS and traditional CV risk factors, with CS increasing the prognostic value of traditional clinical predictors, has been addressed in several studies. The St. Francis Heart Study,19 a prospective population-based study including 4613 asymptomatic individuals aged between 50 and 70 and followed for 4.3 years, showed that CS predicted CAD events independently of traditional risk factors and C-reactive protein, was superior to the Framingham score in the prediction of events, and enhanced stratification of those falling into the Framingham categories of low, intermediate, and high risk. Data from a large registry15 of 25253 asymptomatic patients followed for 6.8 years revealed that CS provides independent and incremental information in addition to traditional risk factors. In the Rotterdam calcification study,7 the upper percentile range of CS reflected a 12-fold increased risk of MI, also independently of traditional risk factors, even in elderly people. In the 1330 participants with intermediate risk (assessed by the Framingham score) included in the MESA study,13 during a median follow-up of 7.6 years, CS, ankle-brachial index, high sensitivity C-reactive protein and family history of CAD were independently associated with incident coronary heart disease. Further analysis of this study showed that the addition of CS to the Framingham risk score plus race caused the highest increase in the AUC and provided superior discrimination and risk reclassification compared with other risk markers. Therefore, CS constitutes a feasible non-invasive tool that may lead to CV risk reclassification of a significant number of individuals, with a number needed to scan for risk reclassification of patients with intermediate risk estimated at 4–6.20,21
The discrepancy between clinical data and documented CS was also evident in our study, with the distribution of advanced coronary atherosclerosis showing almost a quarter of patients in the two lower quartiles of the Clinical Score. Indeed, these patients with a known higher than expected coronary atherosclerotic burden could not be identified without determination of the CS.
Although the diagnostic sensitivity of the CS in detecting obstructive CAD is high, the frequency of false negatives (significant CAD in the absence of CS) is not well established. The CONFIRM registry18 showed nonobstructive CAD in 13% and obstructive CAD in 3.5% of the 10037 symptomatic patients without known CAD who had CS of zero. In a previously analysis performed in our center20 of 864 patients with zero CS, 12.4% had coronary plaques on contrast CT (1.6% obstructive). The independent predictors of CAD were age >55 years, hypertension and dyslipidemia, and in the presence of these three variables the probability of having coronary plaques was 21%. However, it is important to emphasize the low rate of clinical events in this population without evidence of CS.15
Another important point concerning the CS is the possible effect of CS assessment on reduction of CV risk. This issue was analyzed in the EISNER study,22 in which asymptomatic patients were randomized to CS scan versus no scan with comparison of the changes in CV risk at four years of follow-up. The group of patients scanned showed a net favorable improvement in risk, including a considerable reduction in mean systolic blood pressure and low-density lipoprotein cholesterol, and reduced waist circumference (WC) for those with increased WC at baseline.
Although the results of the present study and previous published data demonstrate the incremental value of the CS over traditional clinical CV risk factors, the accuracy and cost-effectiveness of this more expensive imaging test in large populations has yet to be determined. Nonetheless, the inclusion of objective tools for identification of subclinical CAD in CV risk stratification schemes seems logical and necessary. This will allow identification of patients with higher risk for fatal CV events, which unfortunately are sometimes the first event. As Eugene Braunwald wrote, “treating such events is analogous to locking the barn door after the horse has been stolen.”23
This study has some limitations: it was a single-center study with a medium-sized cohort; the study population had predominantly low-intermediate cardiovascular risk; the risk factors of dyslipidemia and hypertension were included in the analysis as categorical variables, which could have led to underestimation of their predictive power; and follow-up data to assess the prognostic impact of the studied characteristics on clinical outcomes were lacking.
In conclusion, despite the statistical association of CV risk factors with a higher than expected atherosclerotic burden, in the population studied they appear to explain only half of its prevalence. Even when integrated in scores, the predictive power of these risk factors is relatively modest, exposing the limitations of risk stratification based solely on demographic and clinical risk factors. This study provides additional support for the use of CS as a tool for refining CV risk prediction.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.