We report the case of a 31-year-old man, a smoker, previously hospitalized in a medical ward with non-lithiasic necrohemorrhagic pancreatitis. A month after discharge he was readmitted due to fatigue on minimal exertion, exertional dyspnea, orthopnea, asthenia, night sweats and weight loss of 6kg in one month (10 % of body weight). He was transferred to our department with a diagnosis of pericardial effusion with cardiac tamponade and non-lithiasic necrohemorrhagic pancreatitis.
On arrival in the emergency department he was tachypneic (respiratory rate 22 cycles/min), with blood pressure of 96/60mmHg, heart rate of 120bpm, jugular venous distension at 30° and hepatosplenomegaly.
Cardiac auscultation revealed S1 and S2 of reduced intensity; on pulmonary auscultation breath sounds were audible on both sides but diminished in the right base. The ECG showed sinus rhythm with heart rate of 125bpm and poor R-wave progression in the precordial leads.
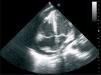
Transthoracic echocardiography performed at the first hospital showed a large pericardial effusion, a 12 × 16mm mass adhering to the roof of the right atrium (RA), and diastolic collapse of the right ventricle, but preserved biventricular function (Figure 1).
Thoracic-abdominal computed tomography (CT) revealed a hypodense area, with a maximum diameter of about 3cm, suggestive of pancreatitis with a necrotic component involving the tail of the pancreas, as well as bilateral pericardial and pleural effusion, moderate on the right.
Pericardiocentesis was performed, and 3100cc of serous fluid was drained. On the second day the pericardial drain ceased to function despite persistence of a large pericardial effusion and signs of tamponade, and so the patient was transferred to our unit.
On arrival transesophageal echocardiography was performed, which showed significant thickening of the atrial septum (13-15mm) and of the roof and free wall of the RA, and a rounded immobile mass adhering to the RA roof (13 × 12mm), not causing obstruction. A moderate pericardial effusion was observed, with slight diastolic collapse of the right ventricle; there were no other relevant alterations on echocardiographic study. Given the setting of necrohemorrhagic pancreatitis, the images of the RA and atrial septum were interpreted as resulting from infiltration or hemorrhage, i.e. intramural hematoma (Figures 2-4).
Laboratory tests on admission showed hemoglobin 11.1g/l, leukocytes 6.51 × 109/l with 74.9 % neutrophils and 13.2 % lymphocytes, CRP 15.47mg/dl, creatinine 1.0mg/dl, total bilirubin 0.8mg/dl, direct bilirubin 0.2mg/dl, triglycerides 230mg/dl, LDH cholesterol 4954 U/l, pancreatic amylase 34 U/l, NT-proBNP 3794.0pg/ml and calcium 7.6mg/dl. Viral markers were positive for type 1 HIV, of which the patient had been unaware.
Pericardiocentesis was repeated and 400cc of yellowish fluid was drained. Biochemical study showed characteristics of exudate; the bacteriological exam was negative, while cytological study revealed some mesothelial cells and multiple large atypical cells with irregular nuclei, prominent nucleoli and evidence of mitosis, that tested positive for LCA and negative for CK7 and calretinin, suggestive of lymphoma.
During his short stay in the ICU the patient was asymptomatic, reporting only slight abdominal pain on palpation of the epigastric and left hypochondriac regions. After stabilization he was transferred to a general ICU in our hospital, where he underwent a minilaparotomy to insert a pancreatic drain, inframesocolic peritoneal drainage, feeding jejunostomy and bilateral pleural drainage.
Cytological study of the pleural fluid revealed Burkitt's lymphoma with a high proliferative index, but there was no evidence of neoplastic cells in the pleural biopsy.
Bone biopsy showed normocellular bone marrow (50 %) with trilineage hematopoiesis and slight alterations in topography and maturation. Minimal focal infiltration of CD20-positive blasts was observed, compatible with infiltration by high-degree B-cell lymphoma. The histopathological diagnosis was:
- 1
– Minimal infiltration of high-degree B-cell lymphoma compatible with Burkitt's lymphoma associated with HIV infection.
- 2
– Dyshematopoiesis associated with HIV infection.
The thoracic, abdominal and pelvic CT exams performed during the patient's stay in the general ICU showed no images suggestive of metastasization.
After 19 days, during which he was hemodynamically stable without requiring inotropic or ventilatory support, the patient was transferred to his local hospital, where he suffered sudden death in the ICU.
DiscussionCardiac involvement as the first manifestation of non-Hodgkin lymphoma is extremely rare, accounting for 1 % of primary cardiac tumors 1. However, its frequency has increased in the last 10 years, mainly in immunocompromised patients with AIDS 2 and transplant patients under long-term immunosuppressive therapy.
The prognosis of primary cardiac lymphoma is generally poor, since by the time it is diagnosed there is usually extensive local infiltration.
The tumor is presumed to originate in perivascular lymphatic tissue. In over 90 % of cases there is pericardial involvement and disseminated disease at initial presentation.
There is no established treatment for cardiac lymphoma and a wide range of therapies have been used; surgery does not improve prognosis 3. Since such tumors are usually high-degree histologically, survival of these patients could probably be improved by early diagnosis and chemotherapy with anthracycline.