Although carotid intima-media thickness (CIMT) is considered a surrogate marker of subclinical atherosclerosis, with known value in risk stratification, its routine use in hypertensive patients is not recommended. The aim of this study was to determine the prevalence of subclinical atherosclerosis through measurement of CIMT and its impact on reclassification of risk in hypertensive patients.
MethodsThis was a cross-sectional study of 94 middle-aged (56.99±11.89 years) hypertensive outpatients without overt cardiovascular disease, 68.1% female. All participants underwent clinical examination, biochemical tests, echocardiogram and measurement of CIMT by high-resolution ultrasound.
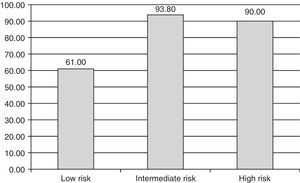
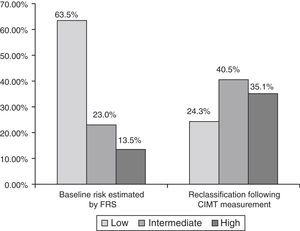
ResultsAlthough the majority of patients were stratified as low (63.5%) or intermediate risk (23%) according to their Framingham score, a high prevalence (75.3%) of increased CIMT was observed in the overall sample, including in the low (61%) and intermediate risk groups (93.8%). CIMT measurement resulted in risk reclassification of 70.31% of the patients, 61% of those at low risk being reclassified as intermediate risk and 93.8% of those at intermediate risk being reclassified as high risk.
ConclusionIn these hypertensive outpatients, predominantly middle-aged and female, CIMT measurement revealed a high prevalence of subclinical atherosclerosis and resulted in risk reclassification in the majority of cases.
Embora a medida da espessura íntimo-medial carotídea (EIMC) seja considerada um marcador direto de aterosclerose subclínica, com importante valor potencial na estratificação de risco cardiovascular, a mesma não tem sido preconizada para uso rotineiro em indivíduos hipertensos. O presente estudo se propôs a investigar a prevalência de aterosclerose subclínica, avaliada pela medida da EIMC, e o impacto desta na estratificação de risco do paciente hipertenso.
MétodosTrata-se de estudo transversal que incluiu 94 hipertensos sem doença aterosclerótica manifesta, com média de idade de 56,99 ± 11,89 anos, sendo 68,1% do sexo feminino, submetidos a exame clínico, dosagens bioquímicas, ecodopplercardiograma e medida da EIMC por ultrassonografia de alta resolução.
ResultadosApesar de a maioria dos indivíduos ter sido estratificada como de risco baixo (63,5%) e intermediário (23%), segundo o escore de Framingham (EF), observou-se expressiva prevalência de espessamento carotídeo na amostra (75,3%), inclusive nos subgrupos de risco baixo (61%) e intermediário (93,8%). A EIMC concorreu para a reclassificação de risco em 70,31% dos pacientes em geral, sendo que 61% dos de risco baixo passaram para o intermediário e 93,8% dos de risco intermediário para o alto.
ConclusãoNestes indivíduos hipertensos ambulatoriais, predominantemente de meia-idade e do sexo feminino, a medida da EIMC demonstrou elevada prevalência de aterosclerose subclínica bem como concorreu para a reclassificação de risco em expressiva proporção dos casos.
Systemic hypertension affects around 50 million individuals in the US and around a billion worldwide.1 Population surveys in Brazil over the last 20 years indicate a mean prevalence of systemic hypertension of around 30%.2,3
Although there is a continuous relationship between blood pressure (BP) and risk for cardiovascular events,4 sustained BP elevation is frequently associated with increased risk due to subclinical cardiovascular disease, including left ventricular hypertrophy, renal glomerular damage and carotid intima-media thickening.5,6 Moreover, it is common for hypertensive individuals to have other cardiovascular risk factors, such as diabetes and hypercholesterolemia. Current Brazilian guidelines accordingly recommend that risk stratification in hypertensives should take account not only of BP levels but also of the coexistence of target-organ damage and other cardiovascular risk factors.2
Ultrasound measurement of carotid intima-media thickness (CIMT) has considerable value for the non-invasive assessment of atherosclerotic disease. Various studies have demonstrated an independent association between CIMT and the incidence of cerebrovascular and coronary artery disease, making CIMT measurement a valuable tool to screen for subclinical atherosclerosis and to stratify cardiovascular risk, potentially adding important information to risk estimates based purely on traditional factors, such as the Framingham risk score (FRS), which is commonly used to determine the 10-year risk of infarction or death due to coronary artery disease in individuals without overt cardiovascular disease.7,8
Although CIMT measurement is recognized as an independent predictor of cardiovascular events, its routine use in hypertensive patients is not recommended in current guidelines, but is reserved for patients who present clinical signs of atherosclerosis or who have been classified as intermediate risk according to their FRS, in whom this score is known to present greater limitations.9,10 Its value in assessing hypertensive individuals considered at low risk according to this score is unknown.
The aim of the present study was to assess the value of CIMT measurement in a population of hypertensive out-patients, independently of their baseline cardiovascular risk, in determining the prevalence of subclinical atherosclerosis and in risk reclassification.
MethodsThis was a cross-sectional study of hypertensive individuals attending an outpatient clinic linked to a teaching hospital, randomly selected from patient records. Exclusion criteria were mental inability or refusal to participate in the study and a history and/or clinical evidence of atherosclerotic cardiovascular disease.
A full history was taken in all patients, including cardiovascular risk factors, and a physical examination was performed, which included measurement of waist circumference, weight and height. Body mass index was calculated as weight in kg divided by height in m2. Blood pressure was defined as the mean of the last two of three measurements by mercury sphygmomanometer, taken at ≥2-minute intervals after a seated rest period of at least five minutes. Smoking was defined as current consumption of ≥1 cigarette/day. Participants who reported less than 30 minutes of exercise three times a week were considered sedentary.
Venous blood samples were collected after 12 hours fasting and the following biochemical tests were performed: hemogram, blood glucose, uric acid, creatinine, potassium, total cholesterol, HDL-cholesterol, LDL-cholesterol and triglycerides. Glomerular filtration rate was estimated using the Cockcroft-Gault formula, and considered low if <60 ml/min/1.73 m2.
A diagnosis of diabetes was defined as the presence of any of the following criteria: fasting glucose ≥126 mg/dl, current use of glucose-lowering medication or two-hour glucose of ≥200 mg/dl on oral glucose tolerance testing. Patients taking lipid-lowering drugs or who presented abnormal serum lipid values (LDL-cholesterol ≥160 mg/dl, HDL-cholesterol <40 mg/dl for men and <50 mg/dl for women and/or triglycerides ≥150 mg/dl10) were considered dyslipidemic. Metabolic syndrome was defined according to the criteria of the International Diabetes Federation (IDF).11
Absolute 10-year risk of myocardial infarction or death due to coronary artery disease was estimated on the basis of the FRS,10 and was classified as low (<10%), intermediate (10–20%) or high (>20%). Patients with diabetes were automatically considered to be at high risk and were excluded from the analysis of risk based on FRS.10
All patients underwent transthoracic Doppler echocardiography and CIMT measurement by high-resolution ultrasound on a General Electric Vivid 3 scanner.
The echocardiographic exams were performed by a single experienced operator, blinded to the patients’ clinical and laboratory data and risk category. Left ventricular mass index (LVMI) was estimated by the method of Devereux and Reichek and adjusted to body surface area, expressed in g/m2.12 Left ventricular hypertrophy was considered present for LVMI >115 g/m2 in men and >95 g/m2 in women.13
Carotid ultrasound was performed by a single experienced operator, blinded to the patients’ clinical and laboratory data and risk category. After at least a 10-minute resting period in supine position, the patient's neck was slightly hyperextended and bilateral panoramic assessment of the carotid system was performed. CIMT was measured in the distal wall (furthest from the probe) of the common carotid artery, 1 cm proximal to the bifurcation, in accordance with current guidelines. The measurement was taken as the distance between the two lines represented by the lumen-intima and media-adventitia interfaces of the arterial wall.14 Carotid thickening was considered present in cases of CIMT >0.9 mm.2,15
In patients classified as low or intermediate risk according to their FRS, the presence of carotid thickening resulted in reclassification to a higher risk category.10
Qualitative and categorical variables were expressed as percentages and continuous variables as means ± standard deviation. Linear regression analysis was used to assess the correlation between the FRS and CIMT. The data were processed and analyzed using SPSS for Windows, version 16.0, a value of p<0.05 being considered statistically significant.
The study was approved by the institution's ethics committee. Written informed consent was obtained from all patients.
ResultsOf the 101 patients initially recruited seven were excluded due to a history and/or clinical evidence of atherosclerotic cardiovascular disease; thus 94 patients, predominantly female, were included, with a mean age of 56.99±11.89 years.
There was a high prevalence of dyslipidemia, metabolic syndrome and left ventricular hypertrophy in the study population. Mean glomerular filtration rate was within the normal range and mean systolic BP was slightly higher than normal limits despite use of antihypertensive agents.
The majority of patients (almost 90%) were classified as at low or intermediate cardiovascular risk according to the FRS, contrasting with the high prevalence of increased CIMT. These and other characteristics of the study population are shown in Table 1.
Characteristics of the study population (n=94).
| Age, years (mean ± SD) | 56.99±11.89 |
| Female, n (%) | 64 (68.1%) |
| Non-white, n (%) | 61 (64.9%) |
| Smoking, n (%) | 9 (9.7%) |
| Sedentarism, n (%) | 39 (41.5%) |
| Diabetes, n (%) | 12 (12.7%) |
| Family history of premature coronary disease, n (%) | 46 (48.9%) |
| Body mass index, kg/m2(mean ± SD) | 28.27±5.04 |
| Waist circumference, cm (mean ± SD) | |
| Men | 93.29±9.18 |
| Women | 92.85±9.68 |
| Fasting blood glucose, mg/dl (mean ± SD) | 102.78±22.83 |
| Total cholesterol, mg/dl (mean ± SD) | 205.26±40.42 |
| HDL-cholesterol, mg/dl (mean ± SD) | |
| Men | 42.52±9.35 |
| Women | 49.43±12.24 |
| LDL-cholesterol, mg/dl (mean ± SD) | 132.03±34.32 |
| Triglycerides, mg/dl (mean ± SD) | 148.59±81.38 |
| Dyslipidemia, n (%) | 65 (72.2%) |
| Metabolic syndrome, n (%) | 50 (58.8%) |
| Creatinine, mg/dl (mean ± SD) | 0.83±0.2 |
| Glomerular filtration rate, ml/min (mean ± SD) | 90.32±30.61 |
| Systolic blood pressure, mmHg (mean ± SD) | 145.63±18.85 |
| Diastolic blood pressure, mmHg (mean ± SD) | 86.95±11.83 |
| Framingham risk score (mean ± SD) | 8.74±8.38 |
| Low risk, n (%) | 52 (63.5%) |
| Intermediate risk, n (%) | 19 (23%) |
| High risk, n (%) | 11 (13.5%) |
| Left ventricular mass index, g/m2(mean ± SD) | |
| Men | 121.04±26.77 |
| Women | 97.2±22.54 |
| Left ventricular hypertrophy, n (%) | 45 (52.9%) |
| CIMT, mm (mean ± SD) | 1.07±0.22 |
| Increased CIMT, n (%) | 61 (75.3%) |
CIMT: carotid intima-media thickness.
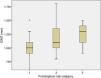
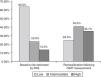
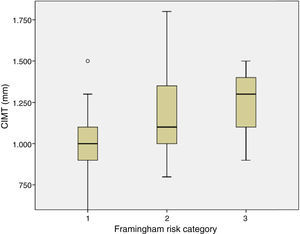
On analysis of the sample by Framingham risk categories, a high prevalence of increased CIMT was found in all groups, even in those classified as low risk (Figure 1). In addition, mean CIMT increased in parallel with risk category (Figure 2).
Simple linear regression analysis showed a significant correlation between CIMT and FRS (r=0.485, p<0.001), which persisted even after adjustment for the different variables that make up the score: age (r=0.335, p=0.002), systolic BP (r=0.450, p<0.001), total cholesterol (r=0.484, p<0.001), HDL-cholesterol (r=0.457, p<0.001) and smoking (r=0.475, p<0.001).
Considering increased CIMT as an aggravating risk factor resulted in 70.31% of the total population being reclassified, 61% of low-risk patients being reclassified as intermediate risk and 93.8% of intermediate-risk patients being reclassified as high risk, changing the profile of the study population to one of predominantly intermediate or high risk (Figure 3).
DiscussionThis study assessed hypertensive patients without overt cardiovascular disease, predominantly middle-aged and classified as low or intermediate risk by the FRS. This patient profile is commonly encountered in clinical practice, but questions remain in terms of risk stratification in these patients.
The prevalence of subclinical atherosclerosis was high in the overall sample, as shown by the finding of increased CIMT in around 75%, and it was relatively high even among those classified as low or intermediate risk by the FRS. The characteristics of the study population, including a high prevalence of uncontrolled BP, dyslipidemia and metabolic syndrome, may explain this finding, which appears to conflict with the low mean FRS observed. Some authors suggest that uncontrolled hypertension is the major determinant of carotid atherosclerosis.16
The clinical importance of increased CIMT led to over half of the low-risk group and almost all the intermediate-risk group being reclassified, which resulted in a significant change in the risk profile of the study population compared to the FRS classification. This finding is important since routine ultrasound study of the carotid arteries in not recommended for hypertensive patients in current Brazilian guidelines, but is only indicated in hypertensives with clinical evidence of atherosclerosis2 or as an alternative method of screening for aggravating risk factors in individuals classified as intermediate risk by the FRS, thus excluding those classified as low risk.10 According to the guidelines, most of the individuals in our sample would therefore not have undergone carotid ultrasound; their risk would have been underestimated and they would have been excluded from stricter therapeutic goals for lipid and BP control.17
The cut-off used in the present study for increased CIMT was the one recommended in the Sixth Brazilian Guidelines on Hypertension,2 but there is some variation in the literature, some studies suggesting slightly higher (>1 mm) and some slightly lower (≥0.8 mm) values.14,15 However, it was not the purpose of this study to screen for carotid atherosclerotic plaques. Despite the lack of consistency in the literature, other studies have also reported significant rates of risk reclassification when carotid ultrasound is systematically performed; one example is an Italian multicenter study involving around 1700 patients, in which the use of carotid ultrasound to measure CIMT and screen for atherosclerotic plaques resulted in the reclassification of around half of those initially considered to be at low or intermediate risk.18
Another important finding of our study was the significant correlation between the FRS and CIMT, which persisted even after adjustment for the variables that make up the score, corroborating the results of the large observational PARC-AALA study involving over 2600 individuals from 21 countries in Asia, Africa, the Middle East and Latin America.19 This highlights the value of the FRS in the general population, particularly in view of its ease of application on a large scale. However, the score may not be sufficient on its own in certain specific populations. It has been found to be less accurate in younger individuals and in women,10 and the present study clearly showed that it significantly underestimated the risk profile of our population of predominantly middle-aged hypertensives, not only of those classified as intermediate risk but also those considered low risk. As mentioned above, this is probably explained by the characteristics of the study population, which undoubtedly contributed to the high prevalence of increased CIMT in the overall sample, including individuals classified as low risk. While reinforcing the importance of the FRS by demonstrating its correlation with CIMT, our findings also point to the need for its applicability to be tested in different patient populations.
Thus, while a significant correlation between the FRS and CIMT was observed, the high prevalence of increased CIMT in the overall sample suggests application of the score in isolation is less useful for risk stratification in these patients and that simple, non-invasive ultrasound measurement of CIMT, a surrogate marker of atherosclerosis, should be used more widely in assessment of hypertensive outpatients.
Finally, it should be noted that the present study was limited by its cross-sectional design and by the fact that it analyzed a specific patient population, and thus its results cannot be extrapolated to the general population. Furthermore, since CIMT measurement is an operator-dependent exam and assessments were performed by a single operator, analysis of intra- and inter-observer agreement was not possible. It should also be borne in mind that no screening for atheromatous plaques was performed, although its incremental prognostic value has been clearly demonstrated.19
ConclusionSystematic assessment by carotid ultrasound in this study of hypertensive patients showed a high prevalence of increased CIMT irrespective of their baseline risk category, resulting in a high rate of reclassification, even among those classified as low risk by the FRS.
Please cite this article as: Das Chagas Monteiro Júnior F, Pereira da Cunha Júnior C, Muniz Ferreira PA, et al. Prevalência de aterosclerose subclínica e reclassificação de risco cardiovascular pela medida da espessura íntimo-medial carotídea em pacientes hipertensos ambulatoriais. Rev Port Cardiol. 2013;32:975–980.