There are several risk scores for stratification of patients with ST-segment elevation myocardial infarction (STEMI), the most widely used of which are the TIMI and GRACE scores. However, these are complex and require several variables. The aim of this study was to obtain a reduced model with fewer variables and similar predictive and discriminative ability.
MethodsWe studied 607 patients (age 62 years, SD=13; 76% male) who were admitted with STEMI and underwent successful primary angioplasty. Our endpoints were all-cause in-hospital and 30-day mortality. Considering all variables from the TIMI and GRACE risk scores, multivariate logistic regression models were fitted to the data to identify the variables that best predicted death.
ResultsCompared to the TIMI score, the GRACE score had better predictive and discriminative performance for in-hospital mortality, with similar results for 30-day mortality. After data modeling, the variables with highest predictive ability were age, serum creatinine, heart failure and the occurrence of cardiac arrest. The new predictive model was compared with the GRACE risk score, after internal validation using 10-fold cross validation. A similar discriminative performance was obtained and some improvement was achieved in estimates of probabilities of death (increased for patients who died and decreased for those who did not).
ConclusionIt is possible to simplify risk stratification scores for STEMI and primary angioplasty using only four variables (age, serum creatinine, heart failure and cardiac arrest). This simplified model maintained a good predictive and discriminative performance for short-term mortality.
Existem vários scores para estratificação de risco em doentes com enfarte agudo miocárdico com elevação segmento ST (EAMCEST), sendo os mais utilizados o TIMI e o GRACE. Contudo, são complexos e necessitam de várias variáveis para o seu cálculo. Este estudo teve como objetivo encontrar um modelo de predição de risco, com menos variáveis e idêntica capacidade preditiva/discriminativa.
MétodosEstudaram-se 607 doentes (62 anos, SD=13; 76% sexo masculino), admitidos por EAMCEST e submetidos a angioplastia primária com sucesso. Consideraram-se como outcomes, a mortalidade intra-hospitalar e aos 30 dias de seguimento. Para identificar quais das variáveis dos referidos scores se revelaram mais influentes na previsão da mortalidade, foram efetuadas análises de regressão logística.
ResultadosDos dois scores clássicos, o GRACE foi o que apresentou melhor capacidade preditiva/discriminativa para a mortalidade intra-hospitalar, com resultados semelhantes para a mortalidade aos 30 dias. Na construção do modelo reduzido, as variáveis selecionadas foram a idade, a creatinina, a insuficiência cardíaca e a paragem cardíaca. As estimativas das probabilidades de morte intra-hospitalar, obtidas através de validação cruzada, foram comparadas com as do modelo original do score GRACE. As capacidades discriminativas foram idênticas tendo ainda sido obtida alguma melhoria nas estimativas das probabilidades de morte (aumento/diminuição para os doentes que morreram/não morreram).
ConclusõesÉ possível uma simplificação dos scores de estratificação de risco para EAMCEST e angioplastia primária com apenas as variáveis idade, creatinina, insuficiência cardíaca e paragem cardíaca. O modelo simplificado manteve um bom desempenho preditivo/discriminativo para a mortalidade a curto-prazo.
angiotensin-converting enzyme inhibitor
acute coronary syndrome
area under the curve
coronary artery bypass grafting
confidence interval
Global Registry of Acute Coronary Events
Hosmer-Lemeshow
intensive care unit
integrated discrimination improvement
net reclassification improvement
odds ratio
percutaneous coronary intervention
receiver operating characteristic
standard deviation
ST-elevation myocardial infarction
Thrombolysis In Myocardial Infarction
Patients with ST-segment elevation myocardial infarction (STEMI) are at increased risk of cardiovascular events, particularly death, in both short- and long-term follow-up.1,2 In these patients, early risk stratification plays a central role, as the benefits of newer and more aggressive and costly treatment strategies seem to be proportional to the risk of adverse clinical events. Different scores are now available based on initial clinical history, electrocardiogram, and laboratory tests, which enable early risk stratification on admission. The Thrombolysis In Myocardial Infarction (TIMI) score was developed using the database of a large clinical trial (Intravenous nPA for Treatment of Infarcting Myocardium Early II).3 The more recent Global Registry of Acute Coronary Events (GRACE) score was based on the registry of the same name, in a population of patients across the entire spectrum of acute coronary syndromes (ACS).4 Both scores were developed for short-term prognosis.
Although percutaneous coronary intervention (PCI) has significantly improved the outcome of patients with STEMI compared to fibrinolytic treatment, high-risk patients still have considerable mortality and morbidity and implementation of new treatment modalities is highly desirable.1,5,6 There is no agreement on how to define high-risk patients with STEMI; different studies used different clinical definitions and scores and there is no unanimity on which definition or score should be used to identify a patient's risk category.1,7–10
The aim of this study was to compare the performance of the TIMI and GRACE scores for risk stratification of STEMI patients, and to assess the feasibility of developing a simpler model with similar predictive performance.
MethodsThis is a retrospective study of consecutive patients admitted to our intensive care unit (ICU) with a diagnosis of STEMI between January 2005 and December 2009. Although this was a retrospective study, data were collected prospectively and recorded in a computer database of ACS patients admitted to our institution's ICU (single-center ACS registry). The inclusion criteria were a history of chest pain at rest or other symptoms suggestive of an ACS, with the most recent episode occurring within 12 hours of admission, associated with at least 1-mm ST-segment elevation in two or more contiguous leads or at least 2-mm elevation in leads V1-V4 or new or presumably new left bundle branch block on the electrocardiogram and serial increases in serum biochemical markers of cardiac necrosis. The registry enrolled patients treated with rescue and primary PCI, but for the purpose of this study we included only patients who underwent successful primary angioplasty (post-procedural TIMI grade >2 flow and <10% diameter stenosis in the infarct-related artery) (98% of all STEMI patients included in our registry). The biomarker used was cardiac troponin I, with a threshold for positivity of 0.06 ng/ml. We evaluated patients’ demographic characteristics, risk factors for coronary artery disease, previous cardiac history, laboratory data, vital signs on admission and in-hospital treatment. Hypertension, diabetes and hyperlipidemia were defined as either previously known or under specific therapy. For each patient, a numerical classification according to the TIMI and GRACE risk scores was calculated from the initial clinical history, electrocardiogram and laboratory values collected on admission.3,4
The study endpoint was all-cause mortality in-hospital and at 30 days. Follow-up was obtained in all patients who survived to discharge by telephone contact 30 days after admission by a dedicated follow-up team. Vital status was available for 99.6% of patients.
The study complies with the ethical guidelines of the Declaration of Helsinki and written informed consent was obtained from all subjects.
Statistical analysisAn exploratory analysis was carried out for all variables. Categorical variables were presented as percentages and continuous variables as mean and standard deviation (SD).
All variables used in the TIMI and GRACE risk scores were considered in multivariate analysis and a new reduced model was obtained with the variables that attained p<0.05 in a backward stepwise logistic regression analysis. In order to compare the classical GRACE risk score with the reduced model, GRACE score estimates of probabilities of death were calculated using Granger's model for in-hospital mortality4 and a 10-fold cross validation was used to estimate the probabilities of death by the reduced model.
Predictive and discriminative abilities were assessed by the Hosmer-Lemeshow (HL) test and by the area under the receiver operating characteristic curve (AUC), respectively. The method described by DeLong et al. was used to compare AUCs from each of these models.11
Continuous net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were also calculated. The net proportion of patients with events, with higher probabilities of death (NRIevents) and of patients without events, with lower probabilities of death (NRInonevents), were calculated using both models. The NRI is the sum of NRIevents and NRInonevents and quantifies the correctness of upward and downward reclassification of predicted probabilities.12 The IDI is a measure of improvement in prediction and may be viewed as the difference between improvement in average sensitivity and in average 1-specificity.12 To complement this comparative study, predictiveness curves were also calculated.13 The interpretation of this curve is straightforward: a marker (or a model) that is useless assigns equal risk to all individuals, and hence, the corresponding predictiveness curve is a horizontal line at the prevalence of the disease; on the other hand, a marker (or a model) that is highly informative about risk yields a predictive curve that is close to a step function.
Two-tailed tests of significance are reported. For all comparisons, a p value of <0.05 was considered statistically significant. When appropriate, confidence intervals (CI) were calculated, with a 95% confidence level.
The statistical analysis was carried out using IBM SPSS Statistics, version 19.0 (IBM Corp., North Castle, New York, USA) and R software.14
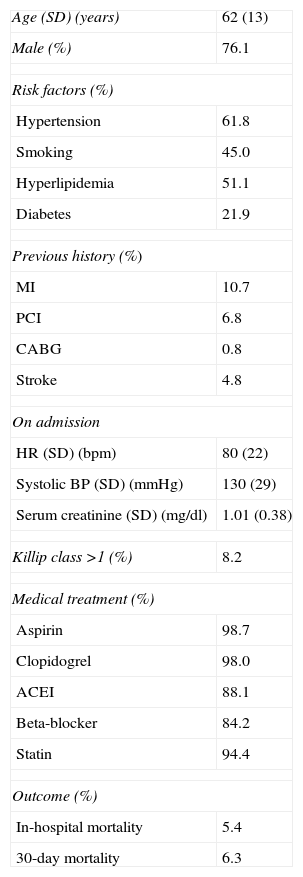
ResultsA total of 607 consecutive patients were included in this study, mainly male (76%), with a mean age of 62 (SD=13) years. The baseline characteristics and hospital management are presented in Table 1. During hospital stay, 33 patients died (5.4%). At 30-day follow-up, there were 38 deaths (6.3%).
Baseline characteristics and hospital management.
| Age (SD) (years) | 62 (13) |
| Male (%) | 76.1 |
| Risk factors (%) | |
| Hypertension | 61.8 |
| Smoking | 45.0 |
| Hyperlipidemia | 51.1 |
| Diabetes | 21.9 |
| Previous history (%) | |
| MI | 10.7 |
| PCI | 6.8 |
| CABG | 0.8 |
| Stroke | 4.8 |
| On admission | |
| HR (SD) (bpm) | 80 (22) |
| Systolic BP (SD) (mmHg) | 130 (29) |
| Serum creatinine (SD) (mg/dl) | 1.01 (0.38) |
| Killip class >1 (%) | 8.2 |
| Medical treatment (%) | |
| Aspirin | 98.7 |
| Clopidogrel | 98.0 |
| ACEI | 88.1 |
| Beta-blocker | 84.2 |
| Statin | 94.4 |
| Outcome (%) | |
| In-hospital mortality | 5.4 |
| 30-day mortality | 6.3 |
ACEI: angiotensin-converting enzyme inhibitor; BP: blood pressure; CABG: coronary artery bypass grafting; HR: heart rate; MI: myocardial infarction; PCI: percutaneous coronary intervention.
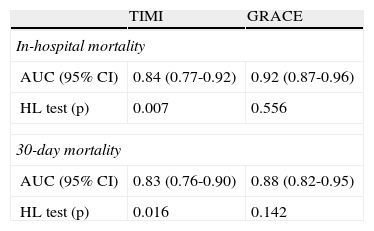
Both TIMI and GRACE scores showed good discriminatory ability regarding mortality in short-term follow-up. However, the performance of the TIMI score was not as good as the GRACE score: its goodness of fit (predictive ability) was inferior, as demonstrated by the p values of the HL test (Table 2). Concerning 30-day follow-up, the two scores were very similar in their predictive performance, but again the GRACE score was better at predicting mortality.
Discriminative ability and goodness of fit of the TIMI and GRACE risk scores.
| TIMI | GRACE | |
| In-hospital mortality | ||
| AUC (95% CI) | 0.84 (0.77-0.92) | 0.92 (0.87-0.96) |
| HL test (p) | 0.007 | 0.556 |
| 30-day mortality | ||
| AUC (95% CI) | 0.83 (0.76-0.90) | 0.88 (0.82-0.95) |
| HL test (p) | 0.016 | 0.142 |
AUC: area under the receiver operating characteristic curve; CI: confidence interval; HL: Hosmer-Lemeshow.
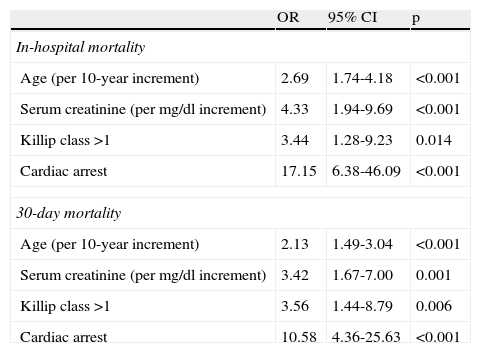
In a stepwise multivariate logistic regression analysis, the most important independent predictors of mortality were age, Killip class on admission, renal function and the occurrence of cardiac arrest. The selected variables were then used to built a new predictive model for both in-hospital and 30-day mortality (Table 3).
Multivariate logistic regression analysis.
| OR | 95% CI | p | |
| In-hospital mortality | |||
| Age (per 10-year increment) | 2.69 | 1.74-4.18 | <0.001 |
| Serum creatinine (per mg/dl increment) | 4.33 | 1.94-9.69 | <0.001 |
| Killip class >1 | 3.44 | 1.28-9.23 | 0.014 |
| Cardiac arrest | 17.15 | 6.38-46.09 | <0.001 |
| 30-day mortality | |||
| Age (per 10-year increment) | 2.13 | 1.49-3.04 | <0.001 |
| Serum creatinine (per mg/dl increment) | 3.42 | 1.67-7.00 | 0.001 |
| Killip class >1 | 3.56 | 1.44-8.79 | 0.006 |
| Cardiac arrest | 10.58 | 4.36-25.63 | <0.001 |
CI: confidence interval; OR: odds ratio.
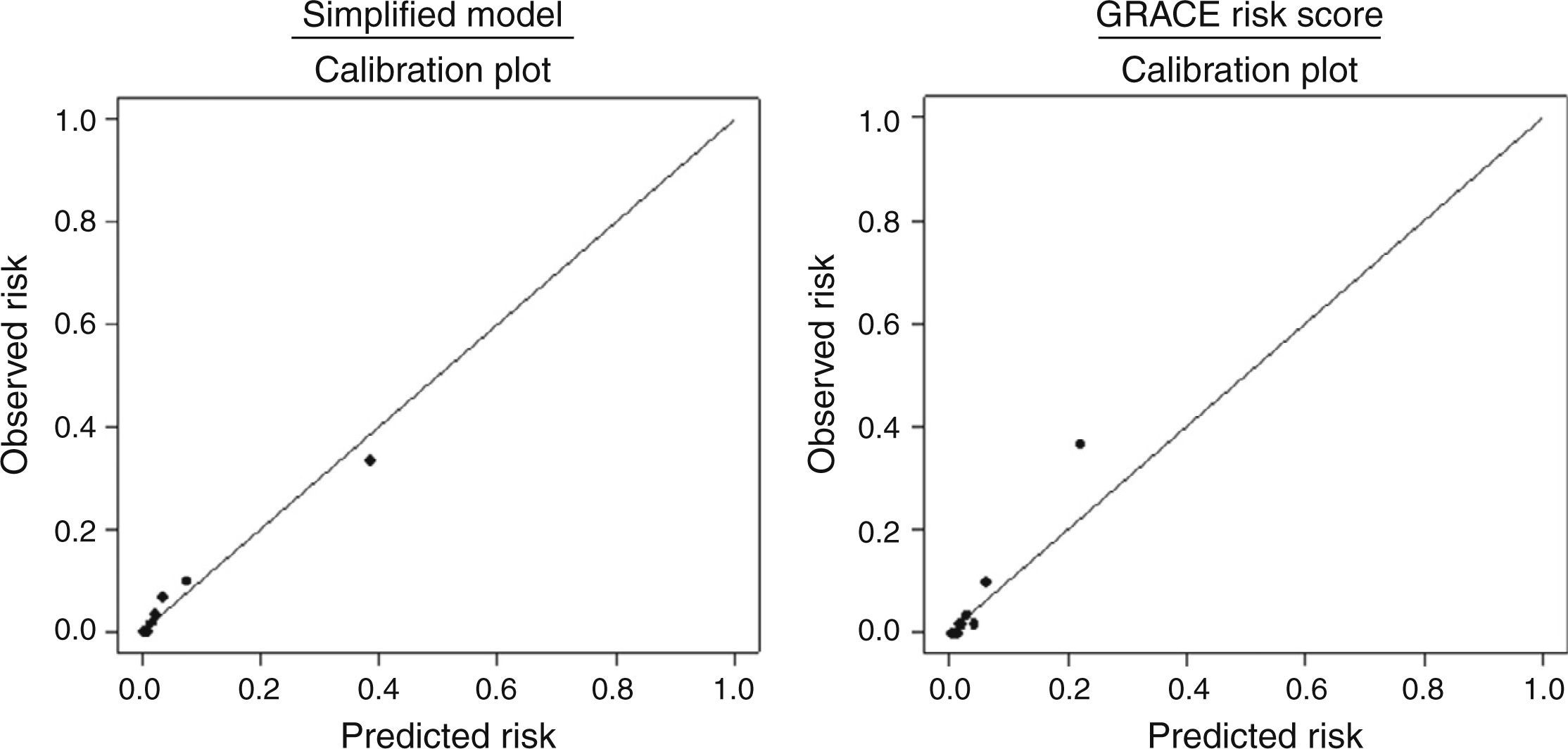
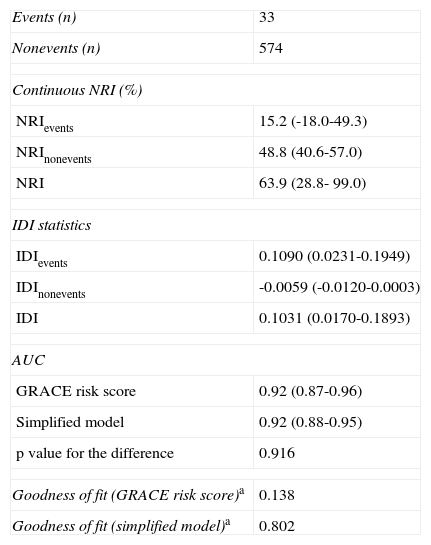
Compared to the GRACE risk score, after 10-fold cross validation, the reduced model showed the same discriminatory ability (AUC=0.92 for both, p=0.916) (Figure 1) and better predictive ability evaluated by goodness of fit (p=0.138 and p=0.802, respectively) and by calibration plots (Figure 2).
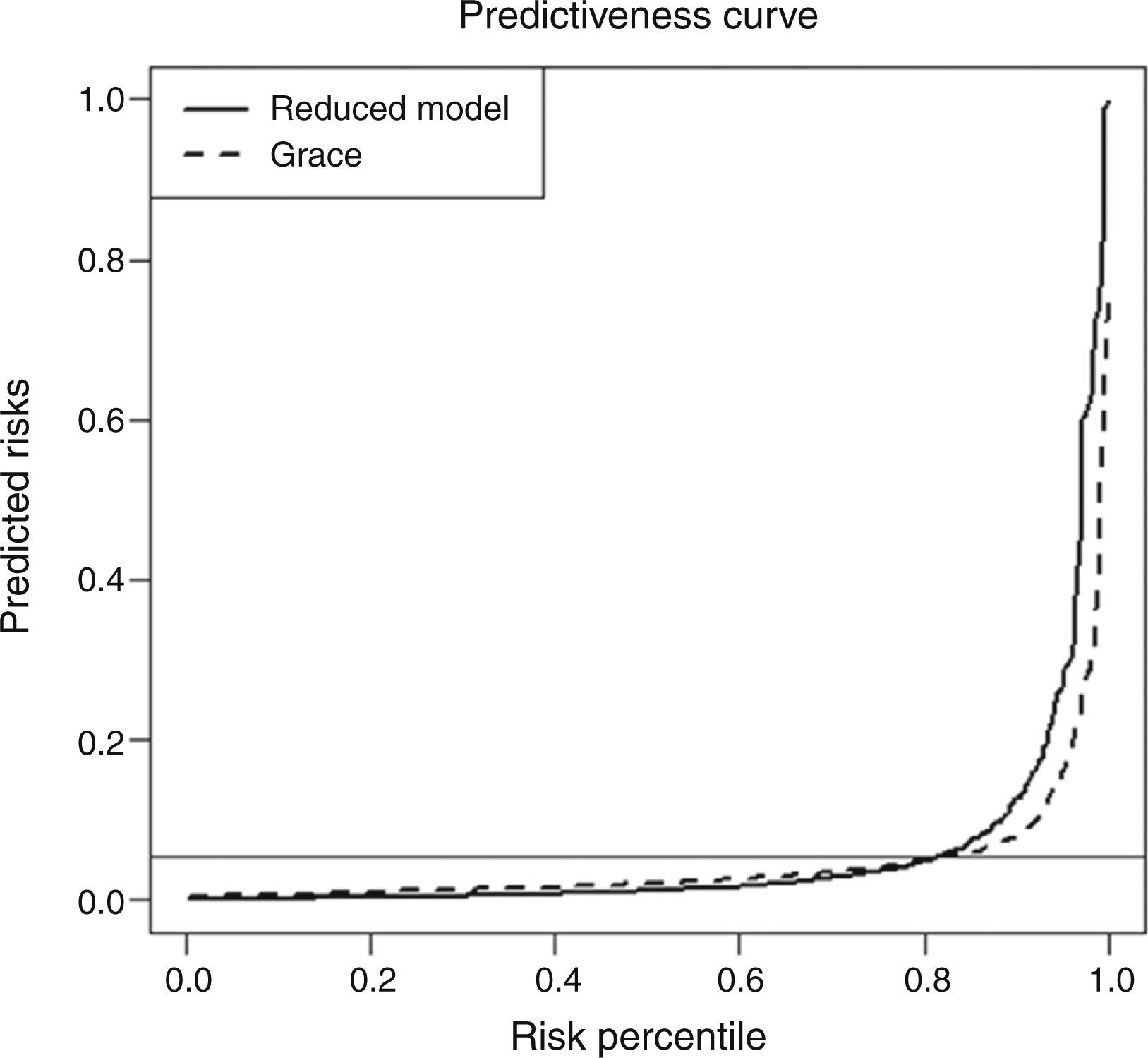
Regarding the other metrics that were used to study model improvement (continuous NRI and IDI), reducing the number of variables used to calculate the GRACE risk score increased the predicted risk of death in 15% of patients who died and reduced the predicted risk of death in 49% of those who did not. This reclassification resulted in an overall continuous NRI of 64%. However, the size of the changes was only significant for those with events (IDI=0.11), with a moderate overall IDI of 0.103. These results are detailed in Table 4 and show a slightly better performance for the reduced model. The comparative study ended with the construction of a predictiveness plot. Analysis of the two curves revealed that the reduced model has a better performance, as seen in Figure 3: the reduced model assigns lower risk to patients with lower risk percentiles (although very slightly) and higher risk to patients with higher risk percentiles (in this case more markedly).
Statistics for model improvement (for hospital mortality) with the simplified model after 10-fold cross validation vs. the GRACE risk score.
| Events (n) | 33 |
| Nonevents (n) | 574 |
| Continuous NRI (%) | |
| NRIevents | 15.2 (-18.0-49.3) |
| NRInonevents | 48.8 (40.6-57.0) |
| NRI | 63.9 (28.8- 99.0) |
| IDI statistics | |
| IDIevents | 0.1090 (0.0231-0.1949) |
| IDInonevents | -0.0059 (-0.0120-0.0003) |
| IDI | 0.1031 (0.0170-0.1893) |
| AUC | |
| GRACE risk score | 0.92 (0.87-0.96) |
| Simplified model | 0.92 (0.88-0.95) |
| p value for the difference | 0.916 |
| Goodness of fit (GRACE risk score)a | 0.138 |
| Goodness of fit (simplified model)a | 0.802 |
95% confidence intervals are shown in brackets. a Hosmer-Lemeshow goodness of fit test (p value). AUC: area under the receiver operating characteristic curve; IDI: integrated discrimination improvement; NRI: net reclassification improvement.
Predictiveness curves comparing the GRACE risk score and the reduced prediction model. The reduced model correctly assigns lower risk to patients with lower risk percentiles and higher risk to patients with higher risk percentiles. The horizontal line represents the prevalence of in-hospital death (5.4%).
Effective risk stratification is essential in the management of patients with ACS. Even in patients with STEMI, for whom initial therapeutic options are well-defined, patient risk characteristics have an impact on early therapeutic decision-making, enabling informed decisions regarding additional therapeutic interventions. After reperfusion treatment it is important to identify patients at high risk of further events, and hopefully to intervene in order to prevent those events. Careful attention to pivotal factors that increase the risk of early mortality might illuminate the role of second-tier interventions or adjunctive pharmacotherapy that would further lower the fatality rate of acute MI. In addition, risk stratification may offer the opportunity to select low-risk patients for a less aggressive strategy as well as for early hospital discharge. Tools that enhance the clinician's ability to rapidly and accurately assess risk are thus of substantial interest.
The wide heterogeneity among clinical scores in the assessment of patients’ risk may be relevant to the design of clinical trials targeting high-risk patients. Regarding existing scores, it has been shown that only a few variables are needed to stratify patients with respect to 30-day mortality. However, most scores still include more than five variables, some with further complexity.
The ideal score should have a good balance between complexity and utility. To be useful in clinical practice, a risk stratification tool should be simple and easily applied at the bedside and should make use of clinical data that are routinely available at hospital presentation and offer independent prognostic information. The complexity of a score is essentially determined by factors related to data collection, rather than the methodology involved in the calculation. In this regard, the GRACE risk score has advantages, as all its variables are objective data. However, when more variables are required, this adds complexity to the score.
This single-center study, based on a consecutive STEMI cohort, confirmed that the GRACE risk score is in some respects superior to the TIMI score in the estimation of short-term prognosis. This may be explained by changes in the treatment of STEMI patients over time. Modest increases in the use of aspirin, clopidogrel, glycoprotein IIb/IIIa inhibitors and low molecular weight heparin (instead of unfractionated heparin) have been seen in recent years, particularly in STEMI patients, likely in part accounted for by an increase in the use of primary PCI instead of fibrinolysis as reperfusion therapy.15 There has also been a downward trend in the frequency of bleeding16: although the frequency of major bleeding would be expected to have increased over time as a result of more potent combinations of antithrombotic therapies and greater use of cardiac catheterization and PCI, the opposite is found. This may be due to changes in contemporary clinical practice, and may have implications for mortality. Nevertheless, when major bleeding occurs, it is associated with a greater risk of death. The TIMI score for STEMI was developed for risk stratification in the era of thrombolytic reperfusion therapy3 and not in the context of contemporary treatment, in which PCI (mechanical reperfusion) is the mainstay of treatment and new antithrombotic agents are available. This may be why the TIMI score showed lower predictive accuracy.
On the other hand, although the GRACE database is more recent, only 74.2% of its STEMI patients presenting to the hospital within 12 hours of symptom onset received reperfusion therapy and, of these, only 30.2% underwent primary PCI.15 A third of patients who appeared to be otherwise eligible received no reperfusion therapy and only a third received such therapy within the guideline-recommended targets of 30 and 90 minutes for thrombolysis and primary PCI, respectively.15 The GRACE registry also showed that patients admitted to a hospital with catheterization facilities were more likely to undergo intervention, which may explain the higher risk of death within six months of discharge observed in these patients; this may be partly due to the bias of referral of patients in worse clinical condition to tertiary centers, but also to hazards related to the intervention.15,17
The relative performance of the different risk scores can also be explained by their composition. The TIMI risk score includes age as a categorical variable, unlike the GRACE score. This approach may miss the continuous prognostic value observed over the entire spectrum of age. The TIMI risk score also does not take into account renal function, which is one of the most important predictors of outcome.
In our population, multivariate logistic regression analysis identified age, as a continuous variable, heart failure on admission and baseline serum creatinine as the most significant predictors of prognosis, together with cardiac arrest. Serum creatinine has only more recently been identified as a powerful risk variable, as it was not generally included in ACS databases before 2000.18
After an internal 10-fold cross validation, it was shown that it is possible to obtain a simplified reduced prediction model with only four variables that maintains the same discriminative ability and with a slightly better predictive performance.
In the present study, other traditional risk markers were not significant predictors of outcome. This may be related to the more aggressive invasive management adopted in these high-risk patients, since all patients underwent successful primary angioplasty in the first 12 hours of STEMI. By contrast, studies that demonstrated the prognostic value of other variables such as cardiac biomarkers used peak instead of baseline levels as analyzed in our study.
We chose to study this specific patient population because of the considerable heterogeneity found in ACS populations, which differ in type of medical treatment, use of PCI or fibrinolysis, and mortality. These differences make it difficult to determine the applicability of risk scores to these differing populations. STEMI patients are a high-risk cohort of ACS patients, with the highest mortality. We analyzed patients undergoing successful primary PCI to obtain a more homogeneous population, since other patients have different baseline characteristics and different treatment management and a worse prognosis. For this reason, our study evaluated only primary PCI patients, reflecting the contemporary treatment of STEMI in a more homogeneous population. In these patients, risk stratification is more important, particularly in the selection of new therapies to improve their prognosis, which is ominous, with in-hospital mortality of >5%.15
LimitationsThis is a relatively small sample, and the fact that it is a single-center study may limit our conclusions. Moreover, the results only apply to STEMI patients undergoing successful primary PCI.
Because the GRACE risk score was developed for prediction of hospital mortality, no further comparisons were made regarding 30-day mortality.
It is also important to determine whether the validity of this new model seen for short-term follow-up is maintained in medium-term follow-up (one year).
ConclusionsOf the classical scores available for risk stratification after STEMI and in the contemporary era of treatment, the GRACE risk score has the highest predictive accuracy. It is, however, possible to simplify current scores after STEMI and primary angioplasty with only four variables (age, serum creatinine on admission, heart failure on admission and the occurrence of cardiac arrest). This simplified model maintained good predictive ability for short-term mortality compared to more complex risk scores. Due to our relatively small sample, it was not possible to construct a new score based on the proposed simplified model. However, this study supports the possibility that such a simplified score could be constructed if a much larger sample (such as from a large registry) were used.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestsThe authors have no conflicts of interest to declare.


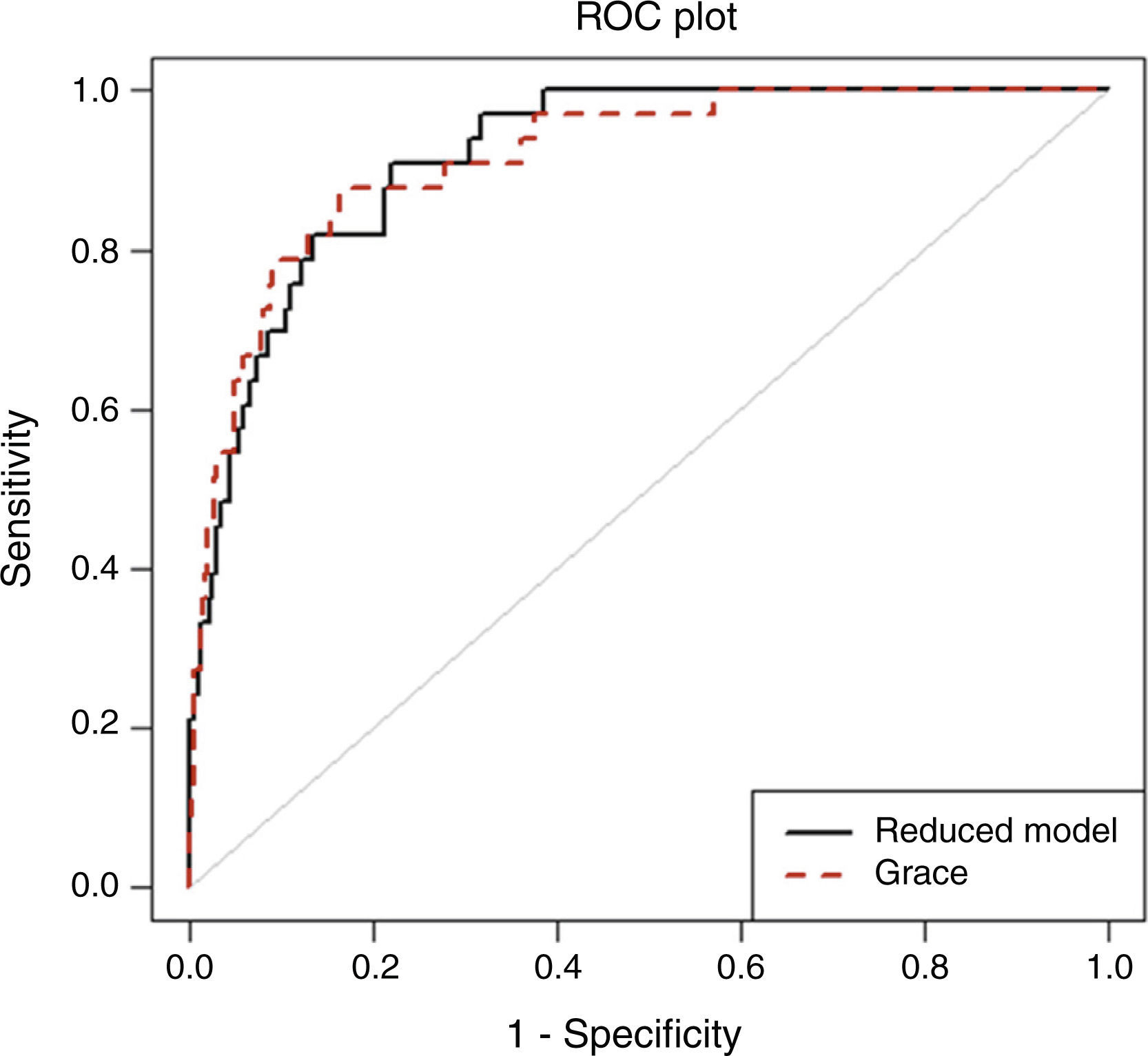
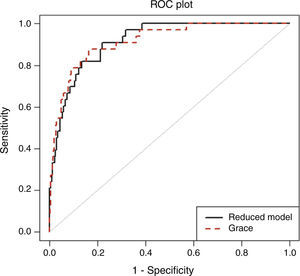 GRACE risk score and the simplified prediction model (p=0.916).' title='Receiver operating characteristic curve analysis comparing the
GRACE risk score and the simplified prediction model (p=0.916).' title='Receiver operating characteristic curve analysis comparing the 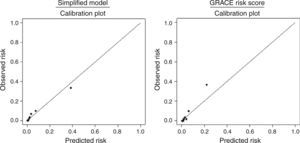 GRACE risk score. The diagonal line indicates perfect calibration (predicted probabilities of death equal estimated probabilities of death).' title='Calibration plots for the simplified model and the
GRACE risk score. The diagonal line indicates perfect calibration (predicted probabilities of death equal estimated probabilities of death).' title='Calibration plots for the simplified model and the 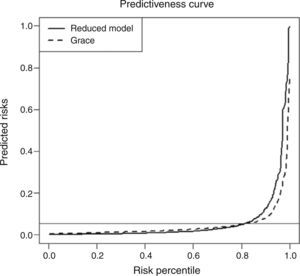 GRACE risk score and the reduced prediction model. The reduced model correctly assigns lower risk to patients with lower risk percentiles and higher risk to patients with higher risk percentiles. The horizontal line represents the prevalence of in-hospital death (5.4%).' title='Predictiveness curves comparing the
GRACE risk score and the reduced prediction model. The reduced model correctly assigns lower risk to patients with lower risk percentiles and higher risk to patients with higher risk percentiles. The horizontal line represents the prevalence of in-hospital death (5.4%).' title='Predictiveness curves comparing the 

