Central blood pressure (CBP) is the pressure exerted by the blood column at any given moment on the aortic and carotid artery walls, which is a close proxy for the blood pressure inside the brain and the heart, and is thus a better marker of cardiovascular morbidity and mortality than peripheral blood pressure (PBP).
ObjectiveTo assess how the augmentation index (AI), peripheral pulse pressure (pPP), central pulse pressure (cPP) and subendocardial viability ratio (SEVR) vary in hypertensive patients according to level of control of CBP and PBP.
MethodsWe performed an observational, cross-sectional study in a convenience sample from a general practice in Central Portugal over a period of four days in May 2010. Measurements were taken after a four-minute resting period. The following values were considered to reflect controlled pressures: PBP <140/90mmHg, CBP <130/80mmHg, pPP <55mmHg and cPP <45mmHg.
ResultsThe sample included 93 patients, 38 male (41.3%), mean age 62.3±11.1 years, with no significant difference in gender distribution. PBP was controlled in 55 (59.8%), and CBP in 53 (57.6%). Both PBP and CBP were controlled in 50 patients (54.3%) and neither was controlled in 34 (37.9%). pPP and cPP were significantly lower in those with controlled PBP (p<0.001) and CBP (p<0.001). AI was non-significantly lower in those with controlled PBP (78±9 vs. 80.7) and those with controlled CBP (78±9 vs.81±7) (p=0.02). SEVR was within the desirable range in 93 patients (92.2%).
ConclusionsIn a convenience sample of 92 patients, PBP and CBP were controlled in 59.8% and 57.6%, respectively. Those with controlled PBP had significantly better peripheral systolic and diastolic blood pressure, CBP, pPP and cPP; the same was true of those with controlled CBP, who also had a significantly better AI.
A pressão arterial central (PAC) é a pressão exercida pela coluna sanguínea, em cada momento, nas artérias aorta e carótidas sendo uma aproximação à pressão arterial no coração e cérebro e assim um marcador mais relacionado com a morbi-mortalidade cardiovascular do que a pressão arterial periférica (PAP).
ObjectivosVerificar, segundo o controlo da PAC e da PAP, como se distribuem os valores de índice de aumento (IA), de pressão de pulso central (PPC), de pressão de pulso periférica (PPP) e razão de viabilidade sub-endocárdica (SEVR), em pacientes com o prévio diagnóstico de hipertensão arterial (HTA).
Material e métodosEstudo observacional transversal em amostra de conveniência no ambiente de Medicina Geral e Familiar (MGF) em quatro dias do mês de maio de 2010. Os pacientes estiveram em repouso durante pelo menos quatro minutos antes do início das duas medições. Definiram-se: controlo de PAP valores inferiores a 140/90mmHg, de PAC valores inferiores a 130/80, de PPP valores inferiores a 55mmHg e de PPC valores inferiores a 45mmHg.
ResultadosAmostra de n=92, sendo 38 homens (41,3%). Idade média de 62,3±11,1 anos, sem diferença por sexos. PAP controlada em n=55 (59,8%) e PAC controlada em n=53 (57,6%). Para n=50 (54,3%) havia simultâneo controlo da PAP e da PAC e para n=34 (37,0%) havia simultâneo não controlo. A PPP e a PPC é significativamente menor nos controlados de PAP (p<0,001) e de PAC (p<0,001) na comparação com os não controlados. O IA é menor sem significado nos controlados da PAP (78±9) que nos não controlados da PAP (80±7) e é também menor nos controlados da PAC (78±9) do que nos não controlados (81±7 (p=0,02). Para n=93 (92,2%) o SEVR tinha um valor desejável. Medicados com medicamentos atuando no sistema renina-angiotensina-aldosterona (SRAA) 78,4% dos estudados.
ConclusõesNuma amostra de n=92 indivíduos, 59,8% tinham PAP controlada e 57,6% tinham a PAC controlada. Há, para a PAP, valores melhores nos controlados e com significado, em Pressão Arterial Sistólica Periférica, Pressão Arterial Diastólica Periférica, Pressão Arterial Central, Pressão de Pulso Periférica e Pressão de Pulso Central. O mesmo se verifica para o Controlo da Pressão Arterial Central com associada diferença significativa para o Índice de Aumento (p=0,02). A percentagem do ciclo cardíaco em diástole, tinha valores desejáveis para 92,2% dos estudados.
Central blood pressure (CBP) is the pressure exerted by the blood column at any given moment in the aorta and carotid arteries, which is a close proxy for the blood pressure inside the brain and the heart. It is now known that CBP has predictive value in cardiovascular disease, independently of peripheral blood pressure (PBP); large-scale studies have shown that CBP is an important therapeutic target in hypertension and a better marker of cardiovascular morbidity and mortality than PBP.1
Hypertensive patients have elevated PBP and pulse pressure (PP), reflecting increased aortic stiffness, and hence increased cardiovascular risk due to the greater mechanical work required for distension,2 particularly in the elderly. It is suggested that drugs that act on the renin–angiotensin–aldosterone system (RAAS) improve central pressure and distensibility.2
As a result of increased life expectancy isolated systolic hypertension is now the most common form of hypertension. It is one of the most frequent diseases confronting general practitioners, and deciding on the appropriate pharmacological therapy can be difficult. The underlying pathophysiology is central arterial stiffness, which leads to progressively increasing PP.
Central systolic pressure is the pressure that the heart has to overcome during ejection, while central diastolic pressure determines coronary perfusion pressure. Equipment that can provide reliable CBP measurements noninvasively is now available,1 based on applanation tonometry, in which information obtained from a probe placed over the radial artery is analyzed and interpreted by software.
The augmentation index (AI) measures the intensity of wave reflections within the vessel and is thus an indicator of arterial stiffness. In the normal arterial tree, the systolic wave is reflected by each bifurcation and returns to the aorta during diastole, boosting coronary perfusion during this phase of the cardiac cycle. In arteries with reduced distensibility, this wave returns prematurely and reaches the aortic root during systole, increasing central systolic pressure and overloading the left ventricle, as well as compromising coronary perfusion.3
The AI can be assessed noninvasively1,3 and is positively associated with cardiovascular risk. High percentages indicate early wave reflection from the periphery due to arterial stiffness and/or increased ventricular ejection time. It is thus a risk marker and should be measured regularly.1,3
Aortic stiffness, as reflected by pulse wave velocity, is an independent predictor of cardiovascular mortality in hypertensive patients; a statistically significant association between mortality and increased pulse wave velocity has been demonstrated.4,5
Central pressure and hemodynamics are known to be independently related to cardiovascular risk, and increased carotid pressure and elevated AI are associated with increased left ventricular mass.1 In addition, CBP is linked to vascular hypertrophy and progression of atherosclerosis.1
Peripheral pulse pressure (pPP), an indirect measure of arterial stiffness, is associated with cardiovascular mortality. However, central pulse pressure (cPP), measured indirectly, is more closely linked to cardiovascular events than pPP.1,5 The CAFE trial6 showed that cPP assessed by applanation tonometry of the radial artery is an independent predictor of cardiovascular events in treated hypertensives. The indicators provided by applanation tonometry are thus of prognostic value as PBP and CBP are surrogate markers for cardiovascular disease.8
The subendocardial viability ratio (SEVR), or Buckberg index, is the ratio between the diastolic and systolic areas in the aortic pressure curve observed by applanation tonometry, and thus reflects the relationship between diastolic and systolic times. The diastolic area is associated with coronary perfusion pressure and time and hence energy supply to the myocardium, while the systolic area is related to cardiac work and hence energy consumption by the myocardium. Thus, a ratio of less than one indicates hypoperfusion, as demonstrated by the CAFE trial.6
The ease and availability of CBP measurement prompted this field study, which set out to assess the level of control of CBP in individuals diagnosed with hypertension, using the SphygmoCor® sphygmomanometer, which is the type most commonly used in clinical studies in which CBP is estimated through analysis of radial or carotid pulse pressures.7
ObjectiveThe aim of the study was to assess how AI, cPP, pPP, and SEVR vary in hypertensive patients according to level of control of CBP and PBP.
MethodsWe performed an observational, cross-sectional study in a convenience sample of individuals diagnosed with hypertension who attended consultations in a health center on the outskirts of Coimbra on May 19, 20, 27 and 28, 2010, and who agreed to CBP assessment.
A SphygmoCor® sphygmomanometer (AtCor Medical) was used to measure CBP and Dinamap (Omron 705IT) to measure PBP, by technicians experienced in their use. SphygmoCor Cardiovascular Management Suite software was used to analyze the results.
Measurements were taken following at least a four-minute resting period. PBP was assessed by the Dinamap device and CBP curves by the SphygmoCor®, and the results were recorded for each individual in the form of figures and tables. Measurements were made with the left arm bare and comfortably supported on a padded surface. PBP was taken as the mean of two readings with the equipment positioned out of the patient's sight; CBP was measured after calibration and visualization of the best window for each individual, in accordance with the software for wave interpretation, and with the probe positioned over the radial artery.
Gender and age were recorded, and two age-groups were analyzed: under 65 and over 64 years.
Controlled PBP was defined as <140/90mmHg, CBP as <130/80mmHg, pPP as <55mmHg, cPP as <45mmHg, and SEVR as >1.
A descriptive statistical analysis was performed using the Student's t test for unpaired variables; normal distribution of the data was confirmed using the Kolmogorov–Smirnov test. The chi-square test and Pearson's correlation test were used for nominal variables.
ResultsThe study population included 92 individuals, of whom 38 (41.3%) were men. Mean age was 62.3±11.1 years (64.6±11.5 for men and 60.9±10.7 for women [p=NS]), minimum 36 and maximum 82 years.
The sample had normal distribution for age, systolic PBP, diastolic PBP and CBP, with values of 0.062, 1.163, 0.678 and 0.814, respectively.
Based on the reference values of 140mmHg for systolic PBP and 90mmHg for diastolic PBP, 55 hypertensives (59.8%) were controlled. Only five (5.4%) of the 92 individuals studied presented both systolic and diastolic hypertension, the remainder having isolated systolic hypertension. Fifty-three (57.6%) had CBP values within the desired range; 82 (90.1%) were taking medication. Table 1 summarizes the mean values of the parameters assessed.
Mean values of the parameters assessed.
| Systolic PBP (mmHg) | 138.1±20.1 |
| Diastolic PBP (mmHg) | 75.6±9.5 |
| Systolic CBP (mmHg) | 127.1±18.4 |
| pPP (mmHg) | 62.6±18.15 |
| cPP (mmHg) | 50.4±16 |
| AI (%) | 79±8 |
| Mean heart rate (bpm) | 69.7±11.7 |
| Increase in CBP (mmHg) | 17.6±8.9 |
AI: augmentation index; CBP: central blood pressure; cPP: central pulse pressure; PBP: peripheral blood pressure; pPP: peripheral pulse pressure.
Table 2 presents mean values in those with controlled and uncontrolled PBP and CBP, which shows significant differences for all parameters except AI.
Mean values of the parameters assessed in those with controlled and uncontrolled PBP and CBP.
| Blood pressure | Parameter | Controlled | Uncontrolled | p |
| Peripheral | Systolic PBP (mmHg) | 125.5±12.6 | 156.8±13.4 | <0.001 |
| Diastolic PBP (mmHg) | 72.8±8.5 | 79.7±9.4 | <0.001 | |
| CBP (mmHg) | 115.9±12.0 | 143.7±13.0 | <0.001 | |
| pPP (mmHg) | 52.7±10.5 | 77.4±17.1 | <0.001 | |
| cPP (mmHg) | 42.0±9.3 | 63.1±15.6 | <0.001 | |
| AI (%) | 78±9 | 80±7 | NS | |
| Central | Systolic PBP (mmHg) | 125.7±13.6 | 154.9±14.4 | <0.001 |
| Diastolic PBP (mmHg) | 71.9±8.1 | 80.6±9.0 | <0.001 | |
| Systolic CBP (mmHg) | 114.9±11.4 | 143.6±12.2 | <0.001 | |
| pPP (mmHg) | 53.8±12.2 | 74.6±18.2 | <0.001 | |
| cPP (mmHg) | 41.9±9.4 | 62.1±15.8 | <0.001 | |
| AI (%) | 78±9 | 81±7 | 0.02 | |
AI: augmentation index; CBP: central blood pressure; cPP: central pulse pressure; PBP: peripheral blood pressure; pPP: peripheral pulse pressure.
With regard to therapy, 78.4% of the study population were taking drugs that act on the RAAS, but no significant difference was found between those taking and those not taking such drugs in AI (0.80±0.08 vs. 0.79±0.08, p=NS) or in control of PBP, CBP, pPP, cPP or SEVR (Table 3).
Control of peripheral blood pressure, central blood pressure, peripheral pulse pressure, central pulse pressure and subendocardial viability ratio according to prescription of renin–angiotensin–aldosterone system inhibitors.
| Controlled | RAAS | Yes*, n (%) | No*, n (%) |
| Peripheral blood pressure | Yes | 40 (58.0) | 11 (58.9) |
| No | 29 (42.0) | 8 (42.1) | |
| Central blood pressure | Yes | 39 (56.5) | 11 (57.9) |
| No | 30 (43.5) | 8 (42.1) | |
| Peripheral pulse pressure | Yes | 24 (34.8) | 8 (42.1) |
| No | 45 (65.2) | 11 (57.9) | |
| Central pulse pressure | Yes | 35 (50.7) | 11 (57.9) |
| No | 34 (49.3) | 8 (42.1) | |
| Subendocardial viability ratio | Yes | 61 (89.7) | 18 (100) |
| No | 7 (10.3) | 0 (0.0) |
RAAS: taking renin–angiotensin–aldosterone system inhibitors.
Table 4 shows cross-referencing of data for control of PBP and CBP, from which it can be seen that 50 individuals (54.3%) had both controlled, while 34 (37.0%) had neither controlled.
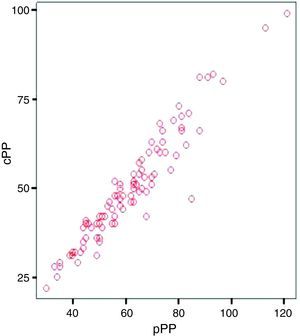
Figure 1 shows that the pPP and cPP curves are similar, with two-tailed Pearson's correlation p=0.01 and r=0.957.
With regard to SEVR, a measure of the percentage of the cardiac cycle in diastole, 83 individuals (92.2% of the total) had a value within the normal range. SEVR was controlled in 94.4% of men and 90.7% of women; those with uncontrolled SEVR were older (mean age 72.1±8.0 vs. 60.9±8.0, p=0.008).
Table 5 shows control of SEVR according to age-group, with a lower proportion of older individuals presenting normal SEVR, although without statistical significance.
As shown in Table 6, only one individual (1.8%) with controlled PBP did not have normal SEVR, as opposed to 17.1% of those with uncontrolled PBP, a significant difference (p=0.01 with Yates correction).
Table 7 shows that 7.5% of those with controlled CBP had uncontrolled SEVR, as opposed to 8.1% of those with uncontrolled CBP.
DiscussionStudies such as the present one face the inevitable problem that in general practice, health centers do not routinely have access to the equipment employed.
The fact that SphygmoCor® and Dinamap equipment, together with experienced operators, were to be provided for a limited period of time raised the question of the method to be used in selecting the study population. We opted for hypertensive patients attending a health center on a particular sequence of days, in order to avoid logistical difficulties in attendance of participants following randomization.
The main source of bias in the study is that patients were attending consultations with their own physicians and only those who consented to participate in the study were assessed, and therefore the study population constituted a convenience sample. A further limitation concerns the definitions used for control of PBP, CBP, pPP and cPP, as well as the choice of the Dinamap and SphygmoCor measuring equipment.
The sample size was sufficiently large to ensure the quality of the results given the methodology used and the study's objective. Not all hypertensive patients follow advice to have their blood pressure measured regularly, but the study population had a similar age and gender distribution to that in the health center's reports on the distribution of the hypertensive population.
The equipment used has been validated,4 which ensures the quality of the measurements.
The results show that there were significant differences in the parameters studied according to whether CBP and PBP were controlled, with the exception of AI in the case of CBP. This highlights the importance of making greater efforts with uncontrolled patients, in terms of encouraging them to comply with therapy, notwithstanding the many factors influencing this question and of ensuring that the therapy is appropriate.2,3
It is particularly interesting that AI was closer to unity in uncontrolled hypertensives and that SEVR was worse in those with controlled CBP, implying that therapy could be improved. In patients with controlled PBP, only one (1.8%) did not have normal SEVR, while the frequency in those with uncontrolled PBP was 17.1%; and 7.5% of those with controlled CBP had uncontrolled SEVR, as opposed to 8.1% in those with uncontrolled CBP.
What the study did show was a high prevalence of controlled PBP in the sample compared to that reported in other studies,8 similar to other studies in Portugal,10,11 demonstrating that CBP measurement can help greatly in improving therapy.
Another interesting finding was that not all individuals with controlled PBP also had controlled CBP, a situation found in 9.1% of the sample. Since CBP is more strongly associated with cardiovascular morbidity and mortality, this means that following the assessment these individuals would need different care, including changes in the therapeutic regime, or even in the time of day at which medications are taken, in order to obtain health gains.3,9 Similarly, 5.6% of the sample had controlled CBP but uncontrolled PBP.
Mean AI differed between individuals with controlled or uncontrolled PBP and CBP, although only significantly in the case of CBP; the lack of a statistically significant difference in those with controlled or uncontrolled PBP may be due to the sample size.
The finding that pPP and cPP curves were similar is a good indicator of the quality of these patients’ standard of care, although the fact that they were assessed during consultations for hypertension may have biased the results.
The fact that SEVR was controlled in most patients is important, since this means that cardiac damage is to some extent being delayed. The elderly had worse control of SEVR, which is a concern and should prompt re-examination of the pharmacological regime in these individuals.
Use of drugs that act on the RAAS did not result in any significant differences in the parameters studied, unlike other studies on smaller samples.2
Periodic assessment of CBP would thus appear to have a role in monitoring hypertensive patients as it gives additional information on the effects of therapy, even though some indicators such as SEVR and AI lacked discriminatory power in our study.
ConclusionsIn a convenience sample of 92 hypertensive patients, PBP and CBP were controlled in 59.8% and 57.6%, respectively; 54.3% had both parameters controlled, while 37.0% had neither controlled; 9.1% had controlled PBP and uncontrolled CBP, and 8.1% had uncontrolled PBP and controlled CBP.
The percentage of the cardiac cycle in diastole (SEVR) was within the normal range in 92.2% of the sample.
The particular pharmacological regime did not appear to affect the parameters assessed.
Further studies are required using this methodology in an outpatient environment in order to draw firmer conclusions, particularly with regard to the value of periodic assessment of SEVR.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Santiago LM, et al. Pressão arterial periférica por Dinamap e pressão arterial central por tonometria planar de absorção no ambulatório de Medicina Geral e Familiar. Rev Port Cardiol. 2013. http://dx.doi.org/10.1016/j.repc.2013.03.001