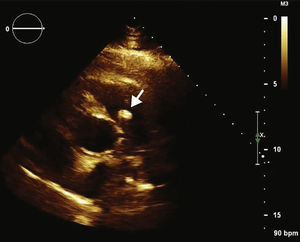
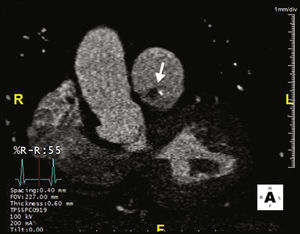
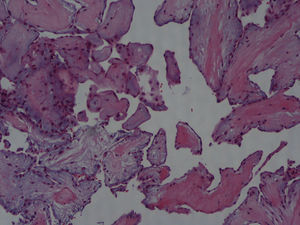
A 42‐year‐old man with a history of hypertension, type 2 diabetes mellitus and obesity was referred to our center due to the incidental finding of a mass adjacent to the pulmonary valve on a routine transthoracic echocardiogram (Figure 1). He was asymptomatic and physical examination and laboratory values were unremarkable. The transesophageal echocardiogram (Figure 2) revealed a pedunculated, highly mobile hyperechogenic mass, measuring 8 mm × 7 mm, attached to the right pulmonary valve leaflet. The pulmonary valve was functionally normal, with no observed pulmonary regurgitation or stenosis, and no masses were visualized on any other valves or heart chambers. Computed tomography angiography excluded significant coronary stenosis and confirmed the presence of a mass at the level of the pulmonary valve (Figure 3). We concluded that it most likely represented a papillary fibroelastoma. Surgical excision of the mass was decided upon due to its mobility and location, resulting in high risk for embolization. It was successfully resected, with preservation of the valve apparatus. Histopathological examination confirmed the diagnosis of papillary fibroelastoma (Figure 4).
Papillary fibroelastomas are rare benign tumors of the endocardium that account for around 7% of all heart tumors. They are located mainly on the left heart valves. Occurrence of these tumors on the pulmonary valve has rarely been reported. Although benign, papillary fibroelastomas can cause turbulent flow, thrombus, embolic events and death. Given these potential complications, surgical resection is recommended in the majority of patients.
1Ethical disclosures1.1Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
1.2Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
1.3Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
2Conflicts of interestThe authors have no conflicts of interest to declare.