The most common etiology of tricuspid stenosis is rheumatic, and in most cases it is associated with valvular regurgitation. Interestingly, there have been reports of tricuspid stenosis without associated valvular regurgitation, mostly related to pacemaker leads. Percutaneous tricuspid valvuloplasty may be a therapeutic alternative to surgery in cases of pure tricuspid stenosis without other concomitant valvulopathies. We report the case of a 52-year-old woman with pacemaker lead-related tricuspid stenosis successfully treated with percutaneous valvuloplasty guided by 3D echocardiography.
A causa mais comum da estenose tricúspide é reumática, e na maioria dos casos está associada com insuficiência valvular. Curiosamente, tem havido relatos de estenose tricúspide sem insuficiência associada, sendo a maioria associados com electrocateteres de pacemaker. A plastia da valva tricúspide pode ser uma alternativa em casos de estenose valvular tricúspide pura, sem outras valvulopatias concomitantes. Relatamos o caso de uma mulher de 52 anos com estenose tricúspide associada a electrocateter de pacemaker tratada com sucesso com valvuloplastia percutânea guiada por ecocardiografia 3D.
We present the case of a 52-year-old woman with a history of congenital atrioventricular block requiring pacemaker implantation at the age of 22 years, who was admitted with dyspnea and lower limb edema. Transthoracic echocardiography revealed severe tricuspid valve stenosis (gradients over 10 mmHg) secondary to fibrosis of one of the valve leaflets located over the pacemaker lead. No tricuspid regurgitation was observed.
After medical and surgical assessment, it was decided that the patient was a candidate for percutaneous tricuspid valvuloplasty (PTV). This procedure was accepted by the patient, who gave her informed consent.
Before PTV, and given the fact that the patient was pacemaker-dependent, two epicardial leads were implanted in the right ventricle.
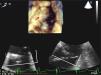
PTV was performed with general anesthesia and orotracheal intubation, and was monitored with real-time three-dimensional (RT3D) transesophageal echocardiography (TEE). In mid-esophageal plane at 25° with simultaneous multiplanar visualization (x-plane mode), long- and short-axis images of the tricuspid valve were obtained. In RT3D mode of the complete volume and using the cropping tool, a view of the tricuspid valve was then obtained from the right atrium (Figure 1). The maximum diameter of the annulus in long- and short-axis views was 30 and 20 mm, respectively.
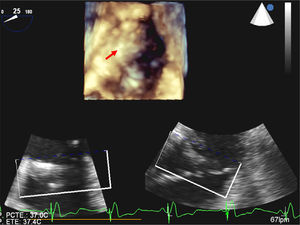
The approach was via the right femoral vein, and the tricuspid valve was crossed by a Glidecath MP catheter (Terumo Medical Corporation) and a straight guidewire. This was replaced by a pigtail catheter, and transvalvular gradients of 15 mmHg were observed. A stiff guidewire (Amplatz Super Stiff, Boston Scientific) was placed over this catheter, and a 30 mm×4 mm balloon valvuloplasty catheter (Tyshak, Numed Inc.) was introduced. Inflation was monitored by fluoroscopy (Figure 2) and RT3D-TEE. After inflation, a transvalvular gradient of 2.8 mmHg was measured by echocardiography. No tricuspid regurgitation was observed.
The patient was discharged after 48 hours without complications. Six months after the procedure, she was in NYHA functional class I with no clinical evidence of right heart failure. The transvalvular gradient by transthoracic echocardiography was 2 mmHg, and no tricuspid regurgitation was observed.
DiscussionThe most common etiology of tricuspid stenosis is rheumatic, and in most cases it is associated with valvular regurgitation.1 Interestingly, there have been reports of cases of tricuspid stenosis without associated valvular regurgitation, most of them pacemaker lead-induced.2 The pathophysiology of this tricuspid stenosis includes mechanical irritation of the leaflets by the leads, leading to fibrosis, calcification, endocarditis and/or thrombus formation.3
TVR may be a therapeutic alternative to surgery in cases of pure tricuspid stenosis without other concomitant valvulopathies.4 There are few data for this option, but the reported results are favorable.5
The implementation of PTV is complicated by the choice of balloon size, because the tricuspid annulus is oval in shape, but assumes a more circular shape on dilation. This makes it more difficult to assess the annulus with two-dimensional echocardiography and hence to choose a balloon for PTV.
RT3D-TEE gives a clear characterization of the morphology and abnormalities of the tricuspid valve,6 as well as providing short-axis views of the valve (simultaneously viewing the three leaflets and their junction with the annulus), enabling planimetry and calculating the area and size of the annulus with high accuracy.6
RT3D-TEE may thus be a helpful tool in monitoring TVR, providing a detailed image of the tricuspid valve. With this technique, balloon size can be selected with greater accuracy and the results of its implementation can be comprehensively assessed.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare