Aortic disease can be highly variable in terms of lesion morphology, clinical presentation and etiology.
We present the case of a young man who suffered a gunshot injury at the age of 12, resulting in paraplegia. Later a murmur was detected and at age 25 a pseudoaneurysm was diagnosed, with fistulization to the left pulmonary artery. Given his good functional status, he was initially managed by a conservative strategy, with regular follow-up. At age 35 left ventricular dilatation was observed with tachycardia and systolic dysfunction, and he was referred for transcatheter aortic valve replacement. Currently, at age 41, he is well in cardiovascular terms, with a good procedural result and professionally active.
A patologia da aorta é muito variada no que diz respeito à morfologia, apresentação clínica e etiologia.
Apresenta-se o caso de um homem baleado aos 12 anos, tendo ficado paraplégico. Posteriormente foi detetado um sopro cardíaco e, aos 25 anos, um pseudoaneurisma da aorta torácica descendente, com fistulização para a artéria pulmonar esquerda. Mantido inicialmente em seguimento, com bom status funcional, observa-se aos 35 anos aumento do volume do ventrículo esquerdo, associado a taquicardia e diminuição da função sistólica. Neste contexto, foi decidida intervenção percutânea, com colocação de prótese aórtica percutânea (TEVAR). Atualmente, com 41 anos, permanece assintomático do ponto de vista cardíaco, mantendo-se bom resultado da implantação da prótese.
Aortic disease can be highly variable in terms of lesion morphology, clinical presentation and etiology. Pseudoaneurysm of the thoracic aorta is an uncommon condition, the main predisposing factors for which are thoracic surgery and trauma. Clinical presentation varies, depending on size, speed of development and involvement of adjacent structures, ranging from a clinical picture suggesting acute aortic or coronary syndrome to sudden death, or it may be completely asymptomatic.
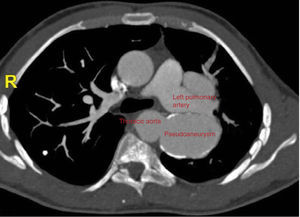
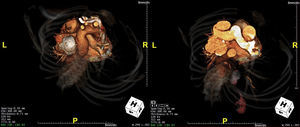
Case reportAt the age of 12, a young man had been accidentally shot in the anterior chest (4th-5th intercostal space), suffering spine injury that resulted in paraplegia. He retained functional autonomy in a wheelchair. At age 15 a mild cardiac murmur was detected during a routine consultation, but he had no cardiovascular symptoms. At the age of 25, although he was still asymptomatic, the murmur had worsened and become continuous, and he was referred for cardiological consultation. Chest X-ray during etiological study revealed a hypodensity in the left perihilar region. This finding was investigated by computed tomography (CT), which revealed a pseudoaneurysm, with fistulization to the left pulmonary artery (Figures 1–3).
Following joint medical and surgical evaluation, in view of the risks of intervention and the patient's clinical stability, it was decided to adopt a conservative strategy and to continue cardiology follow-up.
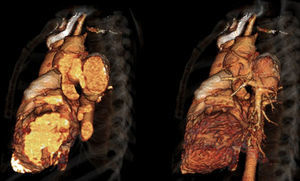
The patient remained active and working, with no cardiac symptoms during outpatient follow-up. In 2007, at age 35, left ventricular dilatation and systolic dysfunction (ejection fraction 41%) were observed, probably due to high output caused by the fistula. The case was accordingly re-evaluated and it was decided to intervene. A 28 mm×100 mm Valiant Thoracic Stent Graft was implanted percutaneously; the procedure was uneventful. He continued to be monitored in cardiology follow-up consultations, which showed good cardiovascular evolution, with recovery of left ventricular function (ejection fraction stable at 53%).
Currently, at age 41 and six years after the procedure, he is well, with no cardiovascular symptoms (Figures 4 and 5).
Discussion and conclusionsThis case illustrates the fact that several simple factors can make a significant difference to the outcome of a clinical case:
- -
The clinical picture, in this case a murmur that subsequently developed new characteristics, is of crucial importance in assessing a patient, even when advanced technologies are available;
- -
New technology that can help confirm or establish a diagnosis and aid in therapeutic decision-making (in this case CT and magnetic resonance imaging);
- -
Team work, in this case leading to the initial decision not to intervene, on the grounds that the benefits did not justify the risks;
- -
Thoracic endovascular aortic repair, which is now increasingly used and was an excellent option for this patient.
The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Neves D, Bettencourt N, Braga P, et al. Sopro de uma bala – lesão antiga, nova terapêutica. Rev Port Cardiol. 2015;34:423.e1–423.e3.