The literature concerning the effects of cardiac rehabilitation (CR) on field tests results is inconsistent.
PurposeTo perform a systematic review with meta-analysis on field tests results after programs of CR.
MethodsStudies published in PubMed and Web of Science databases until May 2016 were analyzed. The standard difference in means correct by bias (Hedges’ g) was used as effect size (g) to measure que amount of modifications in performance of field tests after CR period. Potential differences between subgroups were analyzed by Q-test based on ANOVA.
ResultsFifteen studies published between 1996 and 2016 were included in the review, 932 patients and age ranged 54.4-75.3 years old. Fourteen studies used the six-minutes walking test to evaluate the exercise capacity and one study used the Shuttle Walk Test. The random Hedges's g was 0.617 (p<0.001), representing a drop of 20% in the performance of field test after CR. The meta-regression showed significantly association (p=0.01) to aerobic exercise duration, i.e., for each 1-min increase in aerobic exercise duration, there is a 0.02 increase in effect size for performance in the field test.
ConclusionField tests can detect physical modification after CR, and the large duration of aerobic exercise during CR was associated with a better result.
A literatura mostra-se inconsistente sobre o efeito da reabilitação cardiovascular (RVC) nos resultados de testes de campo.
ObjetivoFazer uma revisão sistemática com meta-análise sobre os resultados de testes de campo usados em programas de RCV.
MétodosForam analisados estudos publicados nas bases de dados PubMed e Web of Science até maio de 2016. O tamanho do efeito (g) foi definido como a diferença média padronizada corrigida por viés (g de Hedges) e foi usado para medir a quantidade de modificações no desempenho do teste após o período de RCV. Diferenças potenciais entre os subgrupos foram testadas pelo teste Q baseado na análise de variância.
ResultadosCompuseram a revisão 15 estudos publicados entre 1996 e 2016, com amostra total de 932 pacientes e idade entre 54,4 e 75,3 anos. Catorze estudos usaram o teste de caminhada de 6 min para avaliar a capacidade de exercício e um estudo usou o Shuttle Walk Test. O g de Hedges pela análise aleatória foi de 0,617 (p < 0,001), representou aumento de 20% no desempenho do teste de campo após a RCV. A metarregressão mostrou associação significativa (p = 0,01) para a duração do exercício aeróbio, ou seja, para cada aumento de 1 min na duração do exercício ocorre o aumento de 0,02 no efeito para o desempenho no teste de campo.
ConclusãoTestes de campo identificam mudanças após a RCV e a maior duração do exercício aeróbio durante a RCV se associa com um melhor resultado.
Physical exercise is important in cardiovascular rehabilitation (CR). The physical assessment of patients before starting treatment is thus essential.1–5 In this respect, cardiopulmonary exercise testing (CPET) measures several variables related to cardiorespiratory function, including peak oxygen consumption (VO2 max),6,7 and is considered the gold standard for determining VO2 max.8–13 However, because it is complex and requires maximum effort, CPET is not commonly used in clinical practice.8,9,11,13–24 For example, 12% of patients with coronary artery disease are unable to perform the test with maximal effort.25 Therefore, field tests have been developed to predict VO2 max and to identify functional limitations, enabling VO2 max to be used more regularly in clinical practice.
Several field tests are used in CR. The 6-minute walk test (6MWT; the longest distance walked in 6 minutes),26,27 provides firm evidence of response to clinical changes.10 It correlates with VO2 max in CPET in patients with heart failure28–30 and is sensitive to changes in perception of disease symptoms.31 Moreover, the Shuttle Walk Test (longest distance walked in a 10-meter corridor with gradual increase in intensity) has been used in post-operative coronary artery bypass grafting (CABG) patients,32 heart failure patients33 and in Chagas disease.34
Step tests are also used in patients with respiratory diseases35 suspected coronary obstruction36 and in elderly patients with heart failure.37–39 They require little space and are easy to transport and simple to perform.40
However, the literature on the effects of CR programs on field test performance is inconsistent. Conducting further trials is important and other research models would enable an integrated analysis of published results. In this context, systematically reviewing the literature makes it possible to search for and include references using defined and robust strategies, and a meta-analysis allows a mathematical model to be used to identify potential variables affecting outcome. We did not find any meta-analyses focusing on field tests and CR. As such, the aim of this study was to systematically review the literature on field tests used in CR programs and to perform a meta-analysis to identify (1) the effect of CR on field test performance and (2) training variables that may influence CR effect.
MethodsSearch strategy and selection of trialsTwo researchers (CFT and RRP) independently conducted a literature review in the MEDLINE/PubMed and Web of Science databases. Articles were selected from their date of publication up to May 2016. Doubts concerning article selection were resolved jointly by the researchers based on the proposed inclusion criteria. Medical descriptors standardized by Medical Subject Heading were used, along with terms and expressions in the title or abstract. The following inclusion criteria were taken into account: (1) articles in English, including randomized and non-randomized clinical trials; (2) human subjects (men and/or women over 18 years of age); (3) diagnosis of heart disease; (4) participants in outpatient CR programs; (5) exercise capacity evaluated by means of exercise tests independently of CPET; (6) presence of training-prescription variables; (7) control group.
Trials included in the systematic reviewWe initially identified 1767 articles in both databases, of which 259 were excluded because they were duplicates and 1318 were excluded after analysis of the title and abstract. After reading the remaining trials in full, 15 were used for this review (Figure 1).
Data extraction and quality analysisThe data on trial quality, journal impact factor, year of publication, gender, age, weight, height, body mass index (BMI), ejection fraction (EF), VO2 max, training volume, training intensity, type of training, training location, type of field test used and field test results were independently extracted by two evaluators (CFT and RRP) to a specific spreadsheet. General concordance was 0.92 using Cohen's kappa coefficient. Discordances were resolved by face-to-face discussion. The comparison of field-test values between the experimental and control groups of the trials included was the primary outcome.
Trial quality was assessed using the Physiotherapy Evidence Database (PEDro) scale, which has been reported to be valid56 and reproducible.57 Scoring was performed twice and any doubts were resolved jointly. Articles were not excluded based on the quality result.
Statistical analysisCalculation of the effect sizeEffect size (g) was used to quantify changes in field test performance following the CR period (aerobic training or aerobic+resistance training). Effect size was defined as the standardized mean difference, corrected for bias (Hedges's g), in field test performance for the experimental and control groups. We initially calculated the paired difference (experimental mean-control mean) and the standard deviation (SD) of the paired difference (experimental SD2+control SD2-2×inter-trial correlation×experimental SD×control SD)1/2 to determine the standardized mean difference (SMD). We then determined the SMD (paired difference×(2-2×inter-trial correlation))1/2÷(paired difference of SD) and standard error (SE) of the SMD ((1/n+SMD2÷(2×n))1/2×(2-2×inter-trial correlation))1/2. Finally, the correction factor obtained with the formula 1-{3÷[4× (n total-2)-1]} was multiplied by the SMD to obtain Hedges's g. When the study reported only the SE, the SD was calculated by multiplying the SE by the square root of the sample number, n. No study provided inter-trial group data (correlation between data from the experimental and control groups), so this value was assumed to be 0.5 for all studies. Positive g values indicated increased performance compared to the control group values.
The Q-statistic was calculated to determine whether the degrees of similarity among the effect sizes were significant. It was converted into a standardized measurement of heterogeneity (I2 statistic) and values of 25%, 50% and 75% indicated low, moderate or high heterogeneity, respectively. Risk of bias was analyzed by funnel plot vs. SMD. Publication bias was analyzed using Egger's non-parametric regression (two-tailed) and the method proposed by Duval and Tweedie.
Subset and moderator variable analysesMeta-analysis and meta-regression were performed using the Comprehensive Meta-Analysis program (version 2.2, Biostat Inc., Englewood, NJ, USA) using a random-effects model and Hedges's g correction factor. For significant heterogeneity, moderator variable analysis was used to explain the g-value variability in the outcomes. Potential moderator variables included age, gender, BMI, weight, height, baseline EF, baseline VO2, training time, weekly frequency, duration of aerobic exercise, quality of the trials (PEDro scale), journal impact factor and year of publication of the study.
Subset analysis included the variables type of exercise (aerobic, aerobic+resistance), type of aerobic exercise (walking, bicycle, walking and/or bicycle), type of training (continuous, progressive), training place (home or clinic), type of disease and procedure (angina, myocardial infarction, heart failure, angioplasty and coronary artery bypass grafting). Any differences between subsets were analyzed by Q test based on the analysis of variance (ANOVA).
ResultsDescription of included trialsThe general details of the trials included are described in Table 1. We identified 15 trials published between 1996 and 2016. The total sample consisted of 932 patients (701 men and 191 women). In one trial48 with 40 participants, the number of men and women was not specified. The mean age was between 54.4 and 75.3 years. Fourteen trials used the 6MWT to assess exercise capacity and one study used the Shuttle Walk Test.48 For the statistical analysis of subsets and moderator variables, we therefore considered only trials that used the 6MWT. Only seven studies42,43,45,49,52,54,55 used CPET in combination with field testing.
Trials included in the systematic review of the literature.
| Author and year | Country | Sample | Training characteristic – CR at clinic and at home | Test result |
|---|---|---|---|---|
| McKelvie et al.41 | Canada | HF | 6MWT | |
| EG=90 M and W (64.8 years) | EG=supervised CR at clinic, walking, stationary bicycle, arm ergometer, 60-70% max. HR, 30 min, resistance exercises with equipment 40-60% of 1RM, 1-3 sets, 10-15 reps, 3 times/wk, 12 wk | EG baseline=434±66.5 m, EG final=456±71 m | ||
| CG=91 M and W (66.1 years) | CG=monthly visits and encouragement to continue usual physical activity | CG baseline=421±75.84 m, CG final=436±70 m | ||
| Jónsdóttir et al.42 | Iceland | HF | 6MWT | |
| EG=21 M and W (68 years) | EG=supervised CR at clinic, bicycle, 50% maximum load (W), 15 min, muscle strengthening with circuit, 20-25% of 1RM, 2 times/wk, 20 wk | EG baseline=489.3±75 m, EG final=526.4±71.9 m | ||
| CG=22 M and W (69 years) | CG=not reported in the text | CG baseline=489.2±66.33 m, CG final=494.6±66.4 m | ||
| Freimark et al.43 | Israel | HF | 6MWT | |
| EG=44 M and W (62 years) | EG=supervised CR at clinic, treadmill, stair machine and bicycle, 45 min, 60-70% of max HR, 2 times/wk, 18 wk | EG baseline=316.0±84.5 m, EG final=443.6±83.8 m | ||
| CG=12 M and W (61 years) | CG=not reported in the text | CG baseline=320.0±99.6 m, CG final=281.7±126.6 m | ||
| Chan et al.44 | China | HF | 6MWT | |
| EG=30 M and W (75.3 years) | EG=supervised CR at clinic, aerobic exercises 90 min, 60-80% of heart-rate reserve, 3 times/wk, 6 wk | EG baseline=232.7±110.1 m, EG final=360.2±106.9 m | ||
| CG=28 M and W (73.5 years) | CG=medical recommendation | CG baseline=205.8±87.7 m, CG final=299.9±56.2 m | ||
| Brubaker et al.45 | USA | HF | 6MWT | |
| EG=30 M and W (70.4 years) | EG=supervised CR at clinic, treadmill or bicycle, 30-40 min, 40-70% of heart-rate reserve, 3 times/wk, 16 wk | EG baseline=406.3±30.6 m, EG final=461.77±29.9 m | ||
| CG=29 M and W (69.9 years) | CG=telephone calls from investigators asking about changes in drug treatment every 2 weeks for 16 weeks. They were not asked about exercising | CG baseline=375.51±39.68 m, CG final=423.06±23.8 m | ||
| Gary et al.46 | USA | HF | 6MWT | |
| EG=12 M and W (59 years) | EG=supervised CR at clinic, 30-60 min, 50-70% heart-rate reserve, 3 times/wk, 12 wk, muscle strengthening with TheraBand, 2-3 sets, 12-15 reps | EG baseline=364.3±80 m, EG final=410.7±91.5 m | ||
| CG=12 M and W (61 years)+24 | CG=5 to 6 home visits in the 12-wk period | CG baseline=306.6±121.3 m, CG final=309.7±135.4 m | ||
| Babu et al.47 | India | HF | 6MWT | |
| EG=14 M and W (56.9 years) | EG=unsupervised CR at home, walking 10-80 min, between 4 and 6 on the Modified Borg Scale, 7 times/wk, 8 wk | EG baseline=429.33±125.15 m, EG final=514.53±135.12 m | ||
| CG=13 M and W (58.8 years) | CG=medical recommendations at hospital discharge | CG baseline=310.23±121.11 m, CG final=357.15±147.95 m | ||
| Asbury et al.48 | England | Angina | ISWT | |
| EG=20 (65.1 years) | EG=supervised CR at clinic, circuit, 40-75% of heart-rate reserve, 80 min, 1 time/wk, 8 wk | EG baseline=248.2±121.7 m, Final=305±115.8 m | ||
| CG=20 (65.1 years) | CG=monitoring of symptoms for 8 wk | CG baseline=222±78.4 m, Final=248.5±80 m | ||
| Chen et al.49 | Taiwan | Angioplasty and CABG | 6MWT | |
| EG=21 M and W (69.7 years) | EG=supervised CR at clinic, bicycle, 30 min, 60-80% of heart-rate reserve, 3 times/wk, 12 wk, muscle strengthening with free weights and equipment, 30 min, 40-60% of 1RM, 12-15 reps | EG baseline=354.6±63.7 m, EG final=373.3±62.4 m | ||
| CG=15 M and W (65.1 years) | CG=drug treatment and medical appointments if needed | CG baseline=329.7±47 m, CG final=323.9±146.2 m | ||
| Sawatzky et al.50 | Canada | pre-operative CABG | 6MWT | |
| EG=8 M and W (64 years) | EG=supervised CR at clinic, walking and bicycle, 60 min, 85% VO2 max, muscle strengthening with body weight and TheraBand, 2 times/wk, 16 wk | EG baseline=342±79 m, EG final=474±101 m | ||
| CG=7 M and W (63 years) | CG=3-hour meeting with nurse and anesthesiologist, recommendations for healthy lifestyle habits | CG baseline=337±52 m, CG final=357±27 m | ||
| Begot et al.51 | Brazil | MI | 6MWT | |
| EG=41 M and W (59 years) | EG=unsupervised CR at home, walking 20-40 min, 4 times/wk, 4 wk | EG baseline=460±106 m, EG final=536±106 m | ||
| CG=45 M and W (57 years) | CG=General information on healthy lifestyle habits and importance of continuing the physical activity started at the hospital | CG baseline=457±73 m, CG final=487±73 m | ||
| Chrysohoou et al.52 | Greece | HF | 6MWT | |
| EG=33 M and W (63 years) | EG=supervised CR at clinic, bicycle, 45 min, 80-100% VO2, 3 times/wk, 12 wk, muscle strengthening with equipment, 30-90% of 1RM, 3 sets, 10-15 reps | EG baseline=422±77 m, EG final=476±82 m | ||
| CG=39 M and W (56 years) | CG=usual medical treatment | CG baseline=406±64 m, CG final=423±65 m | ||
| Peixoto et al.53 | Brazil | MI | 6MWT | |
| EG=45 M and W (56.8 years) | EG=unsupervised CR at home, walking, 20-40 min, 4-5 on the Modified Borg Scale, 4 times/wk, 4 wk | EG baseline=434.2±86.3 m, EG final=519.7±79.3 m | ||
| CG=43 M and W (56 years) | CG=standard treatment and instructions to continue physical activity started during hospitalization | CG baseline=439.1±78.4 m, CG final=452.1±111.2 m | ||
| Piotrowicz et al.54 | Poland | HF | 6MWT | |
| EG=75 M and W (54.4 years) | EG=CR with remote clinical monitoring, Nordic walking, starting with 10 min (VO2<14 ml/kg/min); 15 min (VO2=14-20); 20 min (VO2>20) progressing to 45-60 min, 5 times/wk, 8 wk | EG baseline=428±93 m, EG final=480±87 m | ||
| CG=32 M and W (62.1 years) | CG=standard treatment and recommendations on changes in lifestyle and self-care | CG baseline=439±76 m, CG final=465±91 m | ||
| Safiyari-Hafizi et al.55 | Canada | HF | 6MWT | |
| EG=20 M and W (57.8 years) | EG=supervised CR at home, interval walking, 10-50 min, 80-85% peak VO2 followed by active recovery of 40-50% peak VO2, 2 times/day to 5 times/wk, 12 wk; muscle strengthening with gym bands, 10 exercises, resistance by length of band, 1-3 sets, 15 reps, 1-3/wk. | EG baseline=275±37.9 m, EG final=312.2±42.1 m | ||
| CG=20 M and W (58.9 years) | CG=encouragement to practice moderate exercise | CG baseline=259.6±25.1 m, CG final=235.2±28.6 m | ||
Legend: 1RM: one-repetition maximum; 6MWT: 6-minute walk test; CABG: coronary artery bypass grafting; CG: control group; CR: cardiovascular rehabilitation; EG: experimental group; HF: heart failure; HR: heart rate; ISWT: Incremental Shuttle Walk Test; M: men; m: meters, max: maximum; MI: myocardial infarction; min: minute(s); VO2: oxygen consumption; W: women; wk: week(s).
Ten trials were conducted in patients with heart failure,41–47,52,54,55 two in patients following myocardial infarction,51,53 one in patients with angina,48 one in post-angioplasty and CABG patients49 and one in pre-operative CABG patients.50
CR was unsupervised in only one47 of the 10 trials conducted in patients with heart failure. Mean training duration lasted from six44 to 20 weeks42 in two,42,43 three,41,44–46 four,52 five54,55 and seven47 weekly sessions. In one study,55 patients with functional capacities less than 3 metabolic equivalent of tasks (METs) trained daily (5-10 minutes); those at 3-5 METs trained once or twice a day (15 minutes); and those at >5 METs trained for three to five sessions/week (20-30 minutes). All of the trials used aerobic exercises in the CR program, including walking,41,47,55 Nordic walking,54 exercise bicycle,41–43,45,52 treadmill,43,45 stair machine,43 and arm ergometer,41 while one study44 did not specify the type of exercise. Seven trials41,42,46,49,50,52,55 used muscle-strengthening exercises, including three studies with equipment,41,49,52 three with gym bands46,50,55 and one with circuit.42 The duration of aerobic exercise ranged from 1047 to 90 minutes.44
Two trials51,53 were conducted in patients following myocardial infarction, although CR was unsupervised and the aerobic exercise was walking (four weeks, four times a week). In addition, one trial48 was conducted in angina patients in a supervised program (circuit, once a week for eight weeks), another was conducted in post-angioplasty and CABG patients (three times a week for 12 weeks; aerobic exercises on bicycle and resistance exercises with body weight and equipment),49 while a third50 was conducted in pre-operative CABG patients (twice a week for 16 weeks; aerobic exercises on bicycle and walking and resistance exercises with body weight and gym bands). In general, duration of aerobic exercise ranged from 1054,55 to 80 minutes.48
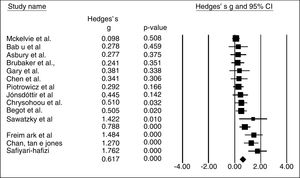
Field test and meta-analysisFigure 2 shows the effect size of the 15 trials. The data were analyzed in meters, taking into account the pre- and post-test means and SDs of the control and experimental groups, as well as the number of subjects in each session. The data were found to be heterogeneous (Q=42.0; degrees of freedom=14; I2=66.7%; p<0.001). Hedges's g using the random model was 0.617 (0.373-0.86; p<0.001), which meant a 20% increase in test performance after cardiovascular rehabilitation.
Table 2 shows the continuous variables analyzed by meta-regression. Only three variables showed significant results: duration of aerobic exercise (p=0.01), baseline VO2 max (p<0.01) and final VO2 max (p=0.01). In this context, for each 1-minute increase in duration of aerobic exercise, g increased by 0.02 in field test performance. This did not occur for baseline and final VO2 max. Instead, for each 1 ml/kg/min reduction in baseline VO2 max, g increased by 0.23, and for each 1 ml/kg/min reduction in final VO2 max, g increased by 0.08. Continuous variables, such as the intensity of aerobic and resistance training, and the number of sets and reps, were not subjected to meta-regression, since the data were presented in broad ranges, hindering meta-regression analysis and stratification for analysis by categorical variables.
Variables analyzed by meta-regression.
| Variable | Number of trials | Slope | p |
|---|---|---|---|
| Study quality | 15 | -0.11 | NS |
| Impact factor | 14 | -0.05 | NS |
| Year of publication | 15 | 0.02 | NS |
| Gender | 14 | -0.01 | NS |
| Age (years) | 15 | 0.003 | NS |
| BMI (kg/m2) | 9 | 0.04 | NS |
| Weight (kg) | 6 | -0.0003 | NS |
| Height (m) | 3 | 0.005 | NS |
| Baseline ejection fraction | 10 | 0.01 | NS |
| Baseline VO2 max (ml/kg/min) | 6 | -0.23 | <0.01 |
| Final VO2 max (ml/kg/min) | 6 | -0.08 | 0.01 |
| Training duration (weeks) | 15 | 0.01 | NS |
| Weekly frequency (days) | 14 | -0.07 | NS |
| Duration of aerobic exercise (minutes) | 12 | 0.02 | 0.01 |
BMI: body mass index; NS: not significant; VO2 max: maximum oxygen consumption.
Table 3 shows categorical variable subsets analyzed by the Q test based on ANOVA. In this group of variables, the duration of aerobic exercise was stratified into three categories (30-35 minutes, 45 minutes; >60 minutes). Duration of over 60 minutes had a significantly larger g than the 30-35 minute duration. In addition, a difference was noted in relation to the type of training; effect size was greater for progressive training than for continuous training.
Subset analysis by categorical variables.
| Variable | Category | No. of trials | Effect size (95% CI) | Comparison (Q test based on analysis of variance) |
|---|---|---|---|---|
| Type of training | Continuous | 4 | 0.27 (-0.11 to 0.65) | Progressive>continuous (p=0.03) |
| Progressive | 6 | 0.64 (0.3 to 0.98) | ||
| Type of exercise | Walking | 6 | 0.66 (0.23 to 1.10) | NS |
| Bike | 3 | 0.45 (-0.15 to 1.04) | ||
| Walking+bike | 4 | 0.66 (0.13 to 1.19) | ||
| Place of training | Home | 5 | 0.74 (0.30-1.18) | NS |
| Outpatient | 10 | 0.56 (0.27-0.85) | ||
| Disease | MI | 3 | 0.80 (0.21 to 1.40) | NS |
| HF | 10 | 0.64 (-0.33 to 0.96) | ||
| ANGIO/CABG | 2 | 0.32 (-0.42 to 1.05) | ||
| Training combination | Aerobics | 8 | 0.64 (0.30 to 0.98) | NS |
| Aerobics+resistance | 7 | 0.62 (0.24 to 1.01) | ||
95% CI: 95% confidence interval; ANGIO: angioplasty; Bike: exercise bicycle; CABG: coronary artery bypass grafting; HF: heart failure; MI: myocardial infarction; NS: not significant.
No publication bias was identified using Egger's regression (p=0.06) and the method proposed by Duval and Tweedie (K=15; Q=31.38).
DiscussionThe aim of this study was to determine the effect size and the variables that influence the results of field tests used in CR programs. The results showed a predominance of 6MWT, which was used in 14 of the 15 trials. The primary outcome was a 20% increase in final vs. baseline field test performance. In addition, performance was associated with progressive aerobic exercise training, longer duration of exercise, and baseline and final VO2 max values.
Aerobic exercise has been established as beneficial to patients with heart failure, through central (increased cardiac output, ventricular remodeling and modulation of the sympathetic nervous system) and peripheral mechanisms (increased peripheral muscle perfusion and increased extraction and use of oxygen).58 In patients with preserved EF, there was an increase in VO2 max due to improved muscle and microvascular function.59 In patients with coronary artery disease, aerobic exercise slows progression and reduces the size of atherosclerotic plaques, improves endothelial function and increases left ventricular EF after myocardial infarction.60 Therefore, our results in relation to the recommendation for aerobic exercise reinforce the data in the literature. Moreover, our study found that better field test performance was obtained based on progressive aerobic exercise, rather than maintaining the same load effort throughout the training period. In this context, as long as physical and clinical conditions allow the patient to handle relatively greater effort after a training period, a gradual increase in intensity may help improve performance. However, data from the references in this study were not conclusive about the best effort intensity or the progression model, because in most of the trials these data were given in broad ranges that did not enable suitable statistical analyses.
Regarding the duration of aerobic exercise, our results showed that the greatest effect occurred in direct relation to the duration of exercise. However, of the 15 trials included, nine used exercise duration of between 30 and 45 minutes; only two studies used one exceeding 60 minutes. Although our results showed that for every 1-minute increase in exercise duration, there was a 0.02 increase in g, this does not necessarily mean that extremely long exercise durations would be positive for the patient. Thus, it is hasty to assume that heart disease patients should perform aerobic exercise for more than 60 minutes. Other trials should therefore be conducted with durations greater than 60 minutes to better analyze results.
Regarding VO2 max, the meta-regression showed a significant relationship between both baseline and final values and field test performance. This suggests that patients with a lower physical fitness level at the start of CR respond better than patients with a higher level. Similarly, patients with a lower fitness level at the end of the CR had a better effect size. These patients tended to have a better response in the field test after CR. In line with our findings, a meta-analysis study61 demonstrated that baseline VO2 max was a predictor of exercise capacity after CR. In addition, the trial found that exercise intensity was another predictive variable of exercise capacity at the end of the rehabilitation program.
However, some other variables did not correlate with increased performance, such as gender, height, weight and BMI. Considering that 6MWT was predominantly used and can be affected by anthropometric differences, we could assume that being taller or heavier affected performance. However, one possible reason that this assumption was not confirmed may be due to the clinical characteristics of the samples. Because we included only trials with patients and not healthy individuals, differences in height, weight and gender did not have the statistical power to influence results. However, the trials did not report separate outcomes for gender or BMI cutoff points when they were present. Therefore, even though our study did not detect a relationship between these variables and test performance, confirmation is still needed. In addition to anthropometric variables, CR duration and weekly treatment frequency did not affect final performance. This may be explained by the difficulty of analysis due to the heterogeneity of protocols regarding the type of supervision, type of aerobic exercise, and duration and intensity of training.
In addition to the physiological variables or training variables, data related to journal impact factor, trial quality and year of publication were also analyzed. These analyses were included to detect bias in trials with different qualities, published in periodicals with different impact factors or published in different years. However, no relationships between these variables and the final outcome were identified.
ConclusionsThe primary outcome of this systematic review with meta-analysis was increased field test performance following CR, and that a longer duration of aerobic exercise equates to better performance. These results may contribute to the prescription of CR exercise sessions.
Sources of fundingThis study was partially funded by the Conselho Nacional de Desenvolvimento Científico e Tecnológico [Brazilian National Council for Scientific and Technological Development] – CNPq – Brazil (process 303566/2013-2).
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Travensolo C, Goessler K, Poton R, Pinto RR, Polito MD. Medida do desempenho físico por testes de campo em programas de reabilitação cardiovascular: revisão sistemática e meta-análise. Rev Port Cardiol. 2018;37:525–537.