The functional significance of coronary lesions can be assessed in the cardiac catheterization laboratory by determination of fractional flow reserve (FFR), thus overcoming one of the major limitations of conventional angiography. The aim of this study was to analyze the long-term clinical course of patients with intermediate coronary stenosis (50–70%) deferred for intervention based on FFR <0.80.
MethodsBetween May 1999 and December 2009, 300 lesions in 231 patients (mean age 65±10 years, 68% male and 75.3% with multivessel disease) were studied by FFR. Intervention was deferred in 282 (94%) lesions and 18 were treated based on FFR <0.80. We assessed the occurrence of major adverse cardiovascular events (MACE), defined as cardiovascular death, non-fatal acute coronary syndrome and target lesion revascularization (TLR).
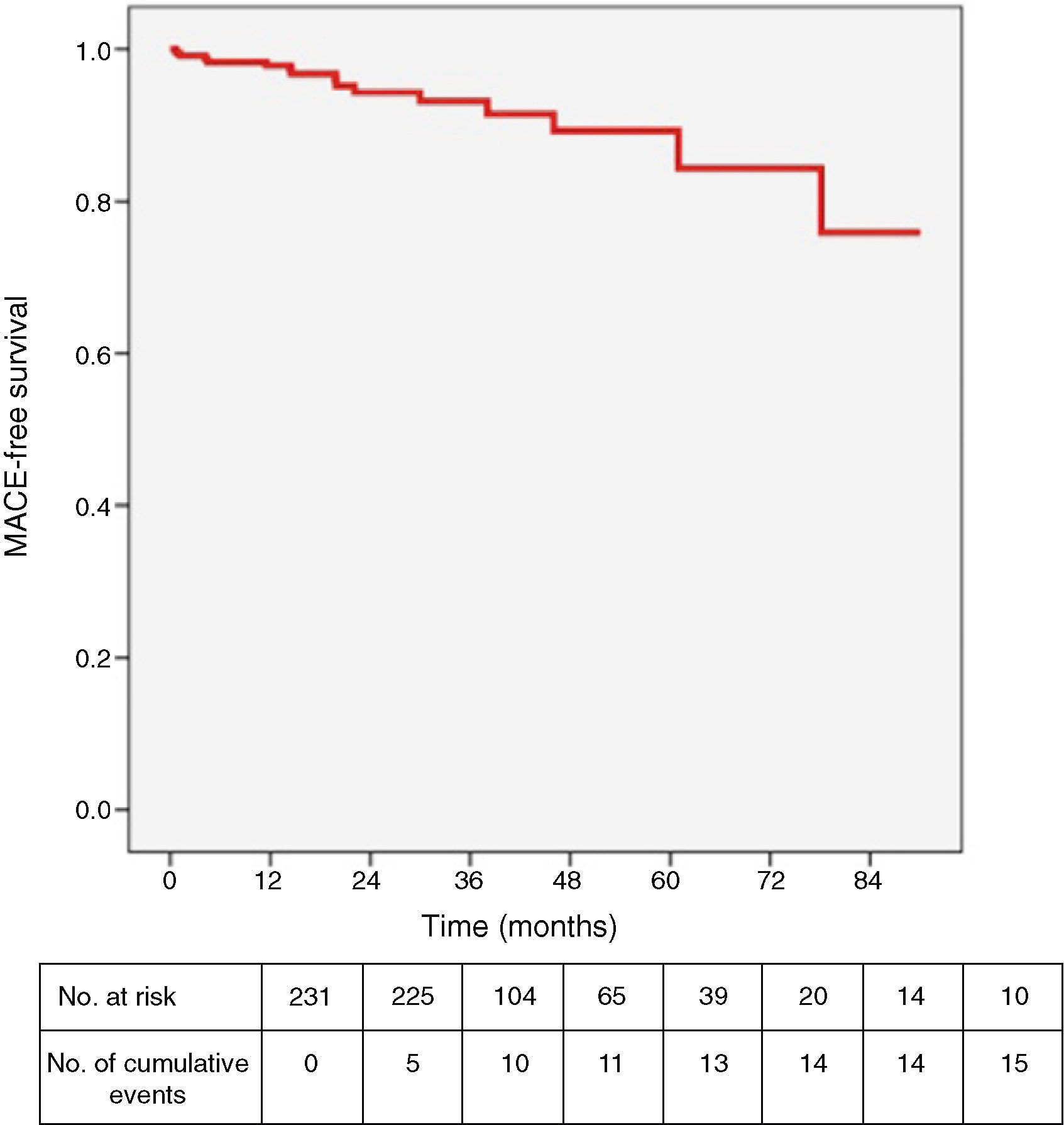
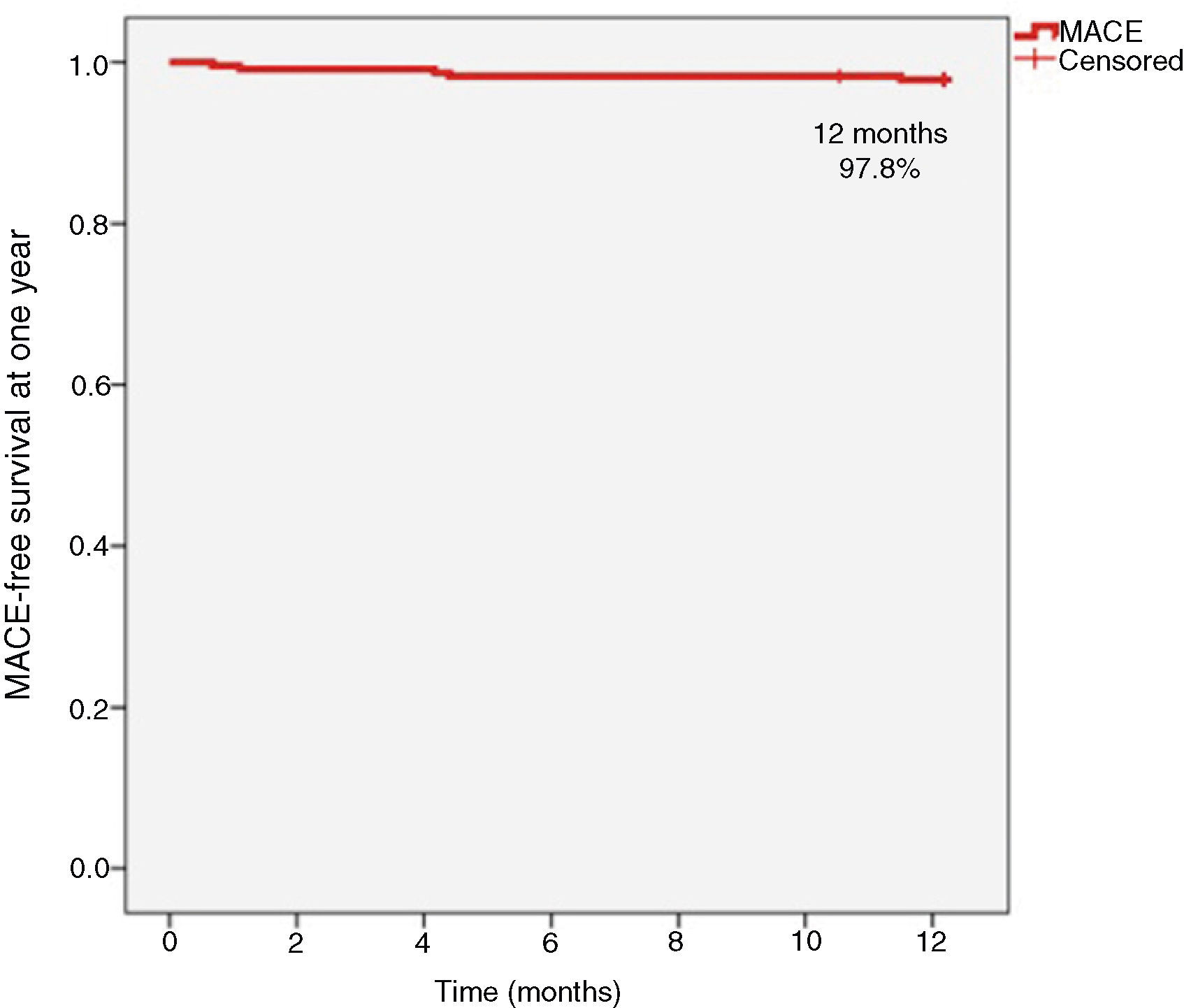
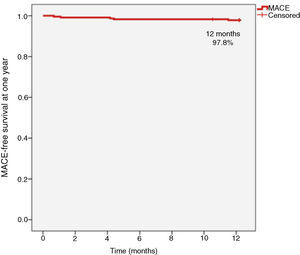
ResultsDuring a median follow-up of 637 days (interquartile range 455–1160), there were 15 (6.5%) MACE in the subgroup of patients with target lesion intervention deferred based on FFR: one cardiovascular death, four hospitalizations for acute coronary syndrome and 14 TLR (12 patients were treated percutaneously and two underwent coronary artery bypass grafting). MACE-free survival at one year follow-up was 97.8%.
ConclusionThese results, in a real-world population, support the current trend to base the decision to treat on functional rather than purely anatomical criteria, in order to improve safety and efficiency.
No laboratório de cardiologia de intervenção é possível efetuar avaliação do significado funcional de lesões coronárias com recurso à determinação da fração do fluxo de reserva coronária por guia de pressão (FFR) e assim ultrapassar uma das limitações principais da angiografia convencional.
O objetivo foi analisar a evolução clínica a longo prazo de doentes submetidos a cateterismo cardíaco no qual se detetaram estenoses coronárias de gravidade intermédia (50-70%) e nas quais a intervenção foi diferida com base no resultado de FFR <0,80.
MétodosEntre maio de 1999 e dezembro de 2009 foram avaliadas por FFR 300 lesões em 231 doentes (idade média 65 ± 10 anos, 68% sexo masculino e 75% doença multivaso). Das 300 lesões estudadas por FFR, a intervenção foi diferida em 282 (94%), tendo sido intervencionadas 18, por apresentarem FFR <0,80. Avaliámos a ocorrência de eventos cardiovasculares major (MACE), definidos como o end point combinado de morte cardiovascular, síndrome coronária aguda (SCA) não fatal e revascularização da lesão alvo (TLR).
ResultadosAo longo de uma mediana de seguimento de 637 [IQR 455-1160] dias ocorreram 15 (6,5%) MACE no subgrupo de doentes com lesão alvo diferida com base no valor do FFR: uma morte cardiovascular, quatro internamentos por SCA e 14 TLR (12 doentes revascularizados de forma percutânea e dois submetidos a CABG). A sobrevida livre de MACE a um ano foi de 97,8%.
ConclusãoOs achados deste estudo relativo a uma população do mundo real consolidam a tendência atual para que a decisão de intervir se baseie em critérios funcionais e não meramente anatómicos, que garantam segurança e eficiência.
Angiography plays a central role in the diagnosis and treatment of coronary artery disease, but as a luminographic technique it has important limitations, particularly its inability to assess the arterial wall and the functional significance of stenosis. Angiographic study complemented by intravascular ultrasound (IVUS) shows a poor correlation between anatomy and physiological assessment of the hemodynamic significance of lesions.1–3
Inducible ischemia on noninvasive testing is an important prognostic marker in patients with ischemic heart disease and should be assessed before a patient undergoes invasive treatment.4,5 The presence of ischemia significantly affects the medium-term clinical course of patients with coronary stenosis of similar angiographic severity.6
Furthermore, myocardial perfusion imaging is insufficiently accurate to assess the relative importance of each lesion in patients with multivessel disease,7 or the functional significance of different lesions within the same vessel.
Many percutaneous procedures are performed in the absence of documented ischemia, with 54.5% of patients in international registries arriving at the catheterization laboratory without prior noninvasive ischemia testing.8
The functional significance of coronary lesions can be assessed in the interventional cardiology laboratory by measurement of fractional flow reserve (FFR) using a pressure guide wire. The primary indication for FFR measurement is to determine the physiological significance of coronary lesions of intermediate angiographic severity (50–70%).9
FFR is the percentage of blood flow through a stenosis compared to the flow that would be obtained in the absence of stenosis and is calculated by the ratio between mean pressure distal to the stenosis and mean aortic pressure (the pressure upstream of the stenosis) during maximal hyperemia induced pharmacologically, usually with adenosine.10,11 Since it is not influenced by disease at the level of the microcirculation, FFR assesses the significance of coronary lesions at the epicardial level only, which is where percutaneous coronary intervention (PCI) is performed. Another advantage is that it assesses the significance of each individual lesion in each vessel.11
In the absence of epicardial lesions, the normal value of FFR is 1 and the cutoff for detection of ischemia is 0.75, with a sensitivity of 90% and specificity of 100%. Values below 0.75 are almost always associated with myocardial ischemia, while stenoses showing FFR >0.80 rarely are; there is a thus a gray area for FFR between 0.75 and 0.80.12 An FFR cutoff of 0.80 has recently been proposed that would bring sensitivity for ischemia detection closer to 100%.13,14
The DEFER study showed that it is safe to defer treatment of functionally non-significant coronary lesions,15,16 and the FAME study demonstrated that in multivessel disease, treatment of epicardial lesions guided by FFR measurement reduces medium-term ischemic complications compared to treatment guided by angiography.17
The aim of this study was to analyze the long-term clinical course of patients undergoing cardiac catheterization in an interventional cardiology unit, in whom detection of intermediate coronary stenosis (50–70%) meant there was no clear indication for intervention, which was deferred if FFR was ≥0.80.
MethodsStudy designThis was an observational, analytical, retrospective cohort study. Clinical data were collected from the Hospital Garcia de Orta interventional cardiology unit database, which is part of the National Interventional Cardiology Registry.
Patient selectionAll patients with intermediate coronary lesions, defined as 50–70% stenosis, consecutively assessed by FFR between May 1999 and December 2009 were included in the analysis. Major adverse cardiovascular events (MACE) were analyzed in the subgroup of patients in whom percutaneous intervention was deferred on the basis of FFR ≥0.80.
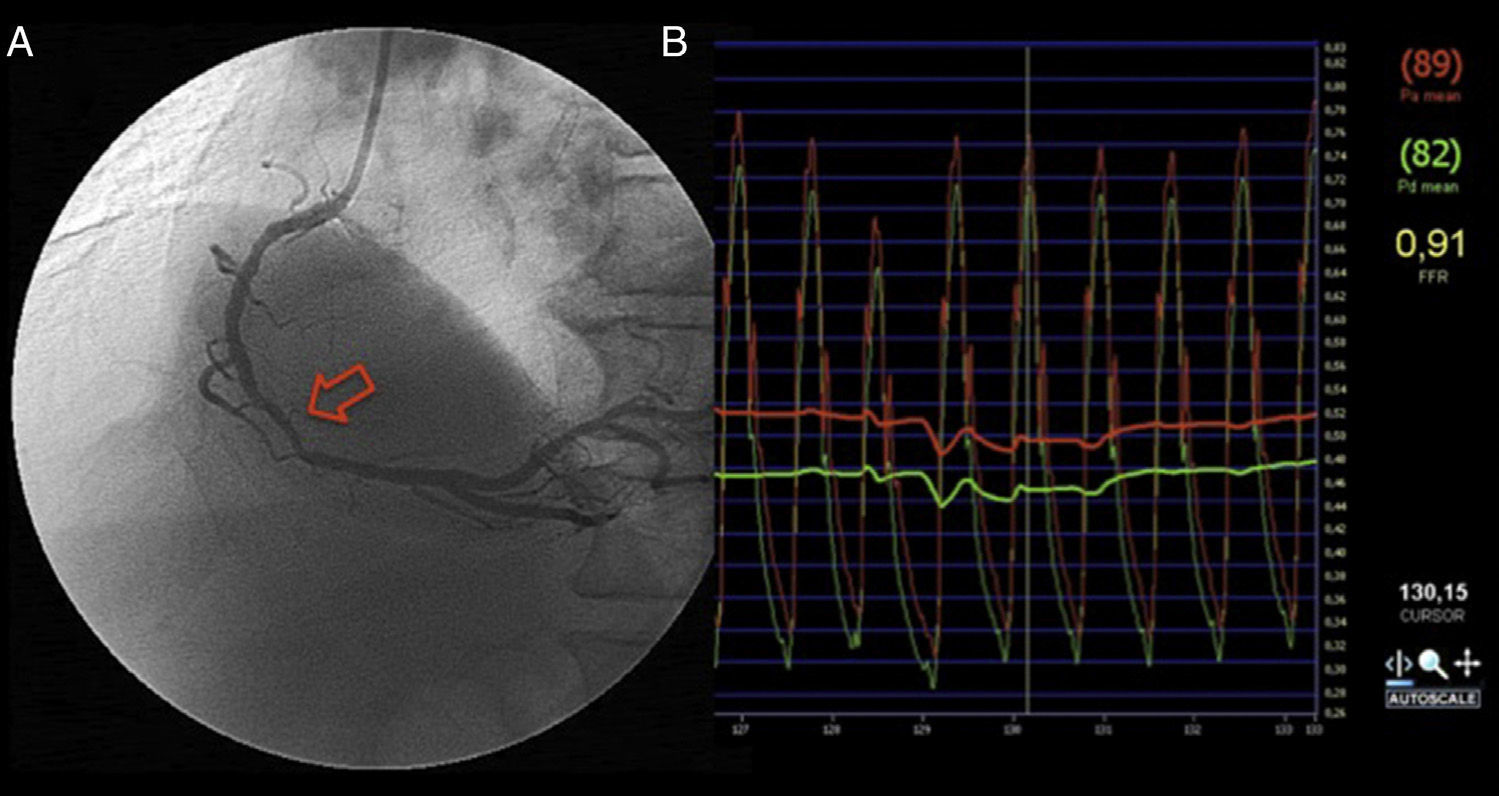
Calculation of fractional flow reserveFFR was measured using a 0.014″ pressure guide wire (Radi Medical System, Uppsala, Sweden), introduced via a 6F guide catheter positioned in the coronary ostium. The guide wire was calibrated according to the manufacturer's instructions and pressures equalized between the guide catheter and the pressure guide wire with both positioned in the coronary ostium. Following positioning of the guide wire distal to the lesion, hyperemia was induced through administration of adenosine, intracoronary or intravenous at the operator's discretion – a 50-μg bolus injected into the right coronary and 80 μg into the left coronary or intravenous infusion of 140 μg/kg/min for two minutes. Intervention was deferred in all cases of FFR ≥0.80.
Follow-up and clinical eventsClinical course was analyzed on the basis of patient records of follow-up consultations in the unit, together with telephone contact in some cases. The occurrence of MACE – cardiovascular death, acute coronary syndrome (ACS) and target lesion revascularization (TLR) (the first event being considered in the analysis) – was determined.
Deaths were classified as cardiac or non-cardiac, all being considered of cardiac etiology unless an unequivocal non-cardiac cause was established.
Up to 2007, myocardial infarction (MI) was defined according to the Joint European Society of Cardiology/American College of Cardiology Committee consensus document,18 and from 2007 onwards according to the definition of the ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction.19
TLR included percutaneous or surgical reintervention involving the proximal or distal 5 mm of a previously treated segment.
Statistical analysisThe statistical analysis was performed using SPSS version 13.0 (SPSS Inc. Chicago, Ill). Continuous variables are expressed as means and standard deviation, or medians and interquartile range (IQR) in cases of abnormal distribution or homogeneity of variance. Categorical variables are expressed as frequencies and percentages. MACE-free survival at one year and throughout follow-up were analyzed using the Kaplan-Meier method.
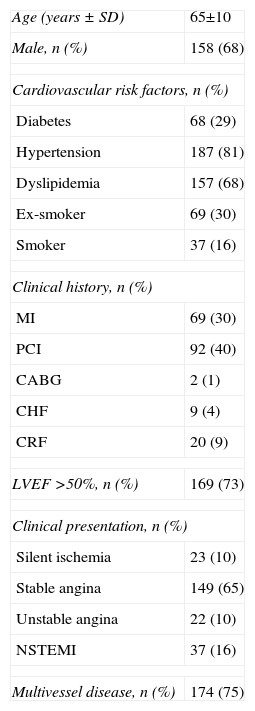
ResultsStudy populationThe sample consisted of 231 patients (300 lesions), 169 (73%) with a single lesion, 55 (24%) with two, and seven (3%) with three. Of the 300 lesions assessed by FFR, intervention was deferred in 282 (94%), and 18 were successfully treated based on FFR <0.80 (0.71±0.08). Mean age was 65±10 years, 158 (68%) were male, and 174 (75%) had multivessel disease. Referral was for stable angina in 65%, ACS in 25%, and silent ischemia detected on noninvasive testing in 10%. There was high prevalence of diabetes (29%), hypertension (81%), dyslipidemia (68%) and smoking (46%). In addition, 30% had a history of MI and 40% of PCI. Left ventricular function was preserved (ejection fraction >50%) in 73%. The demographic and clinical characteristics of the study population are shown in Table 1.
Demographic and clinical characteristics of the study population (n=231).
| Age (years ± SD) | 65±10 |
| Male, n (%) | 158 (68) |
| Cardiovascular risk factors, n (%) | |
| Diabetes | 68 (29) |
| Hypertension | 187 (81) |
| Dyslipidemia | 157 (68) |
| Ex-smoker | 69 (30) |
| Smoker | 37 (16) |
| Clinical history, n (%) | |
| MI | 69 (30) |
| PCI | 92 (40) |
| CABG | 2 (1) |
| CHF | 9 (4) |
| CRF | 20 (9) |
| LVEF >50%, n (%) | 169 (73) |
| Clinical presentation, n (%) | |
| Silent ischemia | 23 (10) |
| Stable angina | 149 (65) |
| Unstable angina | 22 (10) |
| NSTEMI | 37 (16) |
| Multivessel disease, n (%) | 174 (75) |
CABG: coronary artery bypass grafting; CHF: congestive heart failure; CRF: chronic renal failure; LVEF: left ventricular ejection fraction; MI: myocardial infarction; NSTEMI: non-ST-elevation myocardial infarction; PCI: percutaneous coronary intervention.
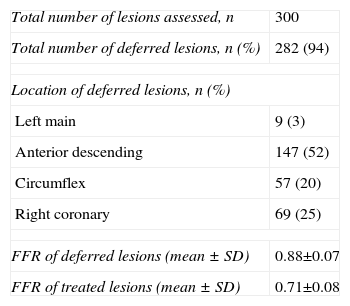
All 282 lesions deferred for intervention following FFR measurement presented 50–70% stenoses on visual assessment. Nine (3%) were located in the left main, 147 (52%) in the anterior descending, 57 (20%) in the circumflex, and 69 (25%) in the right coronary. Mean FFR was 0.88±0.07 (Table 2).
Coronary lesions and FFR.
| Total number of lesions assessed, n | 300 |
| Total number of deferred lesions, n (%) | 282 (94) |
| Location of deferred lesions, n (%) | |
| Left main | 9 (3) |
| Anterior descending | 147 (52) |
| Circumflex | 57 (20) |
| Right coronary | 69 (25) |
| FFR of deferred lesions (mean ± SD) | 0.88±0.07 |
| FFR of treated lesions (mean ± SD) | 0.71±0.08 |
FFR: fractional flow reserve.
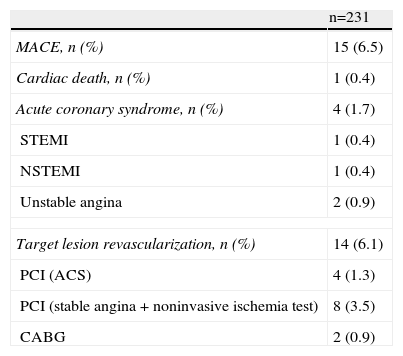
Follow-up data were obtained for all patients; median follow-up was 637 days (IQR 455–1160, minimum 33, maximum 4070). There were 15 (6.5%) MACE related to target lesions deferred for intervention on the basis of FFR (Table 3). Of these patients, four were hospitalized for ACS (two for unstable angina, one for non-ST-elevation MI [NSTEMI] and one for ST-elevation MI [STEMI]), all of whom underwent PCI. Angiographic worsening of the lesions was confirmed in those with unstable angina or STEMI. The presence of thrombus in the target-lesion artery was detected in the one case of NSTEMI, but this patient had a mechanical aortic valve prosthesis and presented a subtherapeutic INR (1.3) following discontinuation of anticoagulant therapy.
Major adverse cardiovascular events during follow-up.
| n=231 | |
| MACE, n (%) | 15 (6.5) |
| Cardiac death, n (%) | 1 (0.4) |
| Acute coronary syndrome, n (%) | 4 (1.7) |
| STEMI | 1 (0.4) |
| NSTEMI | 1 (0.4) |
| Unstable angina | 2 (0.9) |
| Target lesion revascularization, n (%) | 14 (6.1) |
| PCI (ACS) | 4 (1.3) |
| PCI (stable angina + noninvasive ischemia test) | 8 (3.5) |
| CABG | 2 (0.9) |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; NSTEMI: non-ST-elevation myocardial infarction; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction.
Two patients underwent coronary artery bypass grafting, one due to worsening of the target lesion and a positive noninvasive ischemia test; the other underwent surgical replacement of a severely stenosed aortic valve, together with grafting of the left internal mammary artery to the anterior descending artery, which presented an intermediate lesion visually quantified at 60%, with FFR 0.90. The latter procedure was the surgeon's decision, although no angiographic worsening of the lesion was observed at the time of surgery.
Angiography was performed in the other eight patients, followed by PCI, due to anginal symptoms and positive ischemia tests on myocardial scintigraphy. FFR was not measured in these patients to confirm disease progression, the operator's decision to intervene being based on angiographic findings (no conclusive angiographic worsening) and non-invasive ischemia testing. In one of these patients, the decision to intervene was based on morphological assessment by IVUS.
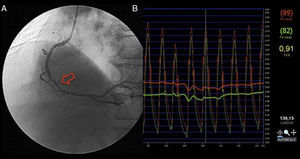
One sudden death occurred, six months after catheterization, which was attributed to cardiac cause, although no autopsy was performed. The patient was 65 years old, with 50% stenosis of the proximal anterior descending and 40% after the origin of the circumflex artery. FFR values were 0.84 in the anterior descending and 0.98 in the circumflex, and so it was decided to maintain medical therapy (Figure 1).
During the follow-up period, there were seven deaths of non-cardiac cause (four from cancer, two from ischemic stroke, and one associated with gastrointestinal bleeding).
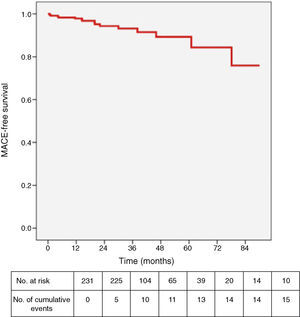
Figure 2 shows MACE-free survival throughout follow-up. At one-year follow-up (achieved in 99.6% of patients), MACE-free survival was 97.8% (0.4% cardiovascular death, 0.9% ACS and 1.7% TLR) (Figure 3).
DiscussionThe FAME study demonstrated that in patients with multivessel disease, treatment decisions guided by functional assessment through FFR measurement compared to those guided by angiography alone (PCI with drug-eluting stents only in lesions with FFR <0.80) reduced the combined rate of death, MI and TLR at two years.17 This study thus changed the traditional approach to PCI in multivessel disease.
However, study populations in randomized trials are often only a selection of patients treated in interventional cardiology laboratories and thus do not reflect the real world. The aim of the present study was to analyze our experience in terms of the long-term clinical course of patients with intermediate coronary lesions (50–70% stenosis) on invasive angiography in a broader, unselected population in whom intervention was deferred on the basis of FFR measurement.
Although in the FAME study,17 which included 509 patients randomized to PCI guided by FFR, there were nine cases of late MI at two years, only one (0.2%) was caused by a deferred lesion, the other eight (1.6%) being related to stents implanted in other lesions or to new lesions. Furthermore, of the 53 (10.4%) revascularizations during follow-up, only 16 (3.2%) were of deferred lesions, the remainder being due to in-stent restenosis or new lesions.
In the present study, with a median follow-up of 21 months, there was one (0.4%) death of presumed cardiac cause, and 14 patients (6.1%) underwent revascularization of lesions initially deferred based on FFR, including two with unstable angina, two with MI and two who underwent CABG. The others underwent PCI, due to symptoms associated with a positive noninvasive ischemia test even in the absence of confirmation of disease progression by FFR.
Despite a higher event rate in deferred lesions than in the FAME study, our study confirms the safety of basing therapeutic decisions on FFR. The greater number of events may be partly explained by the fact that our data reflect everyday clinical practice, an unselected population not subject to trial protocols; in some cases the decision to intervene was prompted by persistence of symptoms without angiographic worsening or was an elective indication in the context of concomitant valve surgery.
Other registries and retrospective observational studies of real-world populations also report higher revascularization rates of deferred lesions than FAME. Rieber et al.,20 in a five-year follow-up of 56 patients with chronic angina and intermediate lesions and using an FFR cutoff of ≥0.75, reported one cardiac death, four noncardiac deaths and five TLRs (8.9%).
In initial studies, notably DEFER, the FFR value taken as the cutoff for ischemia was 0.75.12,15 In FAME,14 the investigators opted for an FFR cutoff of 0.80 in order to avoid deferring treatment of ischemic lesions, and this was the value used in our study.
The one-year prognosis observed in patients with lesions initially deferred for intervention on the basis of FFR ≥0.80 supports the safety of FFR-guided decisions on revascularization of intermediate lesions, since only five MACE (2.2%) were associated with deferred lesions: 0.4% cardiovascular death, 0.9% ACS and 1.7% TLR.
Another important aspect that may influence the use of FFR as a guide in decisions to treat or defer intervention is the financial implications of adopting this technique. As in the FAME study, an economic evaluation was performed, which showed that FFR-guided treatment decisions are more cost-effective than those based on angiography. Apart from being associated with better outcomes, FFR measurement also reduces costs by avoiding unnecessary interventions.21 However, to date there has been no cost-effectiveness analysis of FFR adapted to the Portuguese health system.
Final remarksDespite the good results obtained, the present study has certain limitations. The fact that lesions were assessed by visual rather than quantitative coronary angiography lessens objectivity and may have led to over- or underestimation. Another potential weakness is that the study was based on a retrospective registry, with patients included indiscriminately. Lastly, the fact that it was a single-center study may reduce its external validity, as it merely represents the experience of this center and its operators.
ConclusionsThe findings of this study, in a real-world population, support the current trend to base the decision to intervene on functional rather than purely anatomical criteria, in order to improve safety and efficiency in the treatment of coronary artery disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Vilalonga Pereira L, Pereira H, Vinhas H, et al. Seguimento clínico a longo prazo de doentes com intervenção coronária diferida guiada pela medição da fração de fluxo de reserva coronária. Rev Port Cardiol. 2013;32:885–891.