Cardiac rehabilitation programs are designed to improve patients’ functional capacity, as well as to educate them and to monitor their cardiovascular risk factors.
AimThe study aims to evaluate the effects of cardiac rehabilitation programs in patients with coronary disease over a 12-month follow-up period with regard to control of cardiovascular risk factors.
MethodsThis was a prospective study of patients diagnosed with coronary disease who completed an exercise-based cardiac rehabilitation program between January 2008 and December 2009 and who were not lost to follow-up. Patients were evaluated at an early stage (first medical consultation in phase II of the program) and 3, 6 and 12 months later, the following parameters being assessed: weight and body mass index, waist circumference, lipid profile, HbA1c in diabetic patients, blood pressure, smoking status and physical activity (using the International Physical Activity Questionnaire).
ResultsIn the sample of 256 patients (76.2% male, mean age 67 years), dyslipidemia proved to be the most prevalent risk factor (74.2%), followed by overweight (71.5%). There was a statistically significant improvement (p<0.05) in all risk factors studied at the end of phase II of the program, which was maintained at 6 and 12 months of follow-up, with the exception of body mass index (loss of statistical significance at 6-month assessment, p=0.92).
ConclusionThis study highlights the need for cardiac rehabilitation programs in the context of secondary prevention of cardiovascular disease and the importance of implementing strategies that promote long-term maintenance of their benefits.
Os Programas de Reabilitação Cardíaca visam melhorar a capacidade funcional do doente com patologia cardíaca assim como educar e acompanhar no controlo dos seus fatores de risco cardiovasculares.
ObjetivoAvaliar os efeitos de um programa de Reabilitação Cardíaca em doentes com doença cardíaca isquémica ao longo de 12 meses de follow-up no que se refere ao controlo dos fatores de risco cardiovascular.
MétodosEstudo prospetivo que inclui doentes com diagnóstico de doença cardíaca isquémica que completaram programa de Reabilitação Cardíaca baseado no exercício entre janeiro de 2008 a dezembro de 2009, sem perda de dados no follow-up. Foram avaliados num momento inicial (primeira consulta da Fase II) aos 3, 6 e 12 meses depois, com registo dos seguintes parâmetros: índice de massa corporal, circometria abdominal, perfil lipídico, HbA1c nos doentes diabéticos, tensão arterial, tabagismo e nível de atividade física (através do International Physical Activity Questionnaire).
ResultadosAmostra de 256 doentes (76,2%; idade média: 67 anos); a dislipidemia revelou-se o fator de risco mais prevalente (74,2%) seguido de excesso ponderal (71,5%). No final da Fase II ocorreu uma melhoria estatisticamente significativa (p<0,05) em todos os fatores de risco estudados, que se manteve aos 6 e 12 meses de follow-up, com a exceção do IMC (perda do significado estatístico na avaliação dos 6 meses; p=0,92).
ConclusãoEste estudo salienta a necessidade de programas de Reabilitação Cardíaca no contexto da prevenção secundária da doença cardiovascular e a importância de implementar estratégias que potenciem a manutenção dos benefícios a longo prazo.
acute coronary syndrome
body mass index
blood pressure
coronary artery disease
cardiac rehabilitation program
cardiovascular
Cardiovascular Prevention and Rehabilitation Unit
high-density lipoprotein cholesterol
international physical activity questionnaire
low density lipoprotein cholesterol
total cholesterol
triglycerides
waist circumference
Cardiovascular (CV) disease is the leading cause of morbidity and mortality in Portugal, which highlights the impact of atherosclerosis on public health and the need to implement primary and secondary prevention measures.1 Cardiac rehabilitation programs (CRPs) were established to promote early recovery after an acute event and were designed to fully reintegrate patients into society. Their aims are to inform patients about their condition and to educate them on ways to prevent recurrence by controlling CV risk factors and prescribing physical exercise based on CV risk stratification in order to improve their functional capacity and quality of life.2
The last 10 years have seen growing evidence of the benefits of CRPs in coronary artery disease (CAD), with mortality reduced by 20–30% compared to patients not undergoing cardiac rehabilitation.3–7 Despite these proven benefits, data from a 2007 survey by the European Association of Cardiovascular Prevention and Rehabilitation show that Portugal, together with Spain and Eastern European countries, enroll less than 5% of eligible candidates on such programs, compared to the European average of 30%.3
There are few studies assessing the long-term effects of CRPs in terms of maintaining the preventive measures instituted in their initial phase, especially with regard to the situation in Portugal.
The Cardiovascular Prevention and Rehabilitation Unit (CVPRU) of Centro Hospitalar do Porto – Hospital de Santo António is coordinated by a physiatrist and a cardiologist, and also includes specialists in vascular surgery, urology, psychiatry and endocrinology, as well as physiotherapists, nutritionists and nurses. The CRPs at the CVPRU consist of three distinct, consecutive phases, as recommended in international guidelines.8 Patients are referred to a CRP from cardiology outpatient clinics or during hospitalization in cardiology wards.
Phase I, begun in the hospital, includes the patient's medical history, investigation of comorbidities and education of patients and their carers concerning their condition and CV risk factors; patients are also encouraged to return to activity, under supervision, as soon as possible.
Phase II begins 2–3 weeks after hospital discharge, with assessment by the specialist in physical medicine and rehabilitation in the CVPRU. The educational process continues and an overall clinical evaluation is performed that includes the patient's medical history and cardiorespiratory, neurological and musculoskeletal exams, as well as functional assessment. Diagnostic exams are then scheduled (exercise testing and laboratory tests) for stratification of CV risk, on which an exercise program is based according to the current guidelines.9 Patients are also referred for other consultations at the CVPRU depending on clinical indications, such as nutrition, psychiatry, smoking cessation, urology and vascular surgery. This stage usually lasts 8 weeks but can vary between 6 and 12 weeks depending on clinical needs and the patient's response to exercise. It consists of weekly educational sessions on subjects related to CV risk factors and disease, and therapeutic exercise sessions. The latter are held twice weekly under the supervision of the physiatrist and cardiologist, in accordance with international guidelines on the level of supervision and monitoring appropriate to each case.9 In addition, patients are advised to exercise during the rest of the week, based on the general principles of the program, and are encouraged to increase their level of activity in a safe manner. Each session lasts between 60 and 90minutes; the exercise protocol includes a warm-up period, aerobic training (treadmill and arm and leg ergometers), strength training (using dumbbells, exercise balls and other strength training equipment), a cool-down period and flexibility exercises. The intensity of each exercise component is determined for each individual patient based on their exercise heart rate calculated by the Karvonen formula9 using the data obtained from exercise testing; this is complemented by the patient's rating of perceived exertion on the Borg scale.9 Each session includes a brief clinical assessment, including a questionnaire on relevant symptoms and compliance with medical therapy. Any change in drug therapy, including optimization of dosage when indicated, is the responsibility of the CVPRU's cardiologist in consultation with the attending cardiologist.
During phase III (follow-up), the patient is assessed and encouraged to maintain exercise, healthy behaviors and compliance with prescribed therapy. Follow-up is by outpatient consultations in the physical medicine and rehabilitation clinic, with laboratory tests and functional reassessment through exercise testing at 6 and 12 months after the beginning of phase II, which serves as the basis for a review of the training components prescribed, particularly their intensity, adjusted on the basis of the exercise heart rate whenever necessary.
The present study aims to assess the effects of a CRP in CAD patients over a 12-month follow-up period with regard to control of CV risk factors.
MethodsStudy populationThe population consisted of patients diagnosed with CAD who had completed an exercise-based CRP (minimum of 8 supervised sessions) between January 2008 and December 2009 and who were not lost to follow-up.
The patients were assessed four times: an initial evaluation (first consultation at beginning of phase II of the CRP), and at 3, 6 and 12 months.
Cardiovascular risk factorsCV risk factors were defined in accordance with the European Society of Cardiology guidelines on cardiovascular disease prevention.8
Determination of lipid profile included measurement of total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C) and triglycerides (TG), based on the following references values8: TC <175mg/dl, LDL-C <100mg/dl, HDL-C >45mg/dl and TG <150mg/dl. Laboratory tests were performed on blood samples collected after 12hours’ fasting.
Body composition was assessed by weight, waist circumference (WC) and body mass index (BMI). Obesity was defined according to the internationally recognized classification of BMI ≥30 (weight in kilograms/height in meters squared), and those with BMI 25–29.9kg/m2 were classified as overweight or pre-obese. WC was considered high if >80cm in women and >94cm in men.
Blood pressure (BP) values were recorded and considered high if >130/80mmHg in two consecutive assessments.
With regard to diabetic patients, capillary blood glucose and HbA1c were used to assess diabetes control, fasting blood glucose ≥110mg/dl and HbA1c ≥6.5% being considered abnormal.
Patients’ smoking habits were recorded, those who did not smoke at all being considered non-smokers.
Levels of physical activity were assessed using the International Physical Activity Questionnaire (IPAQ), which has been validated in the Portuguese population.10 This is designed to quantify (in METs/min/week) the amount of exercise taken in a week performing various activities (including household chores, employment, sport and recreation).
Statistical analysisThe data from this prospective study were recorded and analyzed using SPSS version 17.0. Qualitative variables are presented as percentages and quantitative variables as means±standard deviation. Quantitative variables were compared using the Student's t-test and qualitative variables by the McNemar test. Values of p<0.05 were considered statistically significant.
ResultsOf a total of 329 patients, 73 were lost to follow-up. The study population thus included 256 patients, most of whom (81.6%) were referred for CRP during hospitalization in the cardiology ward. The majority were men (76.2%), and mean age was 61.1±10.6 years (30–83). The most common admission diagnosis (65.3%) was acute coronary syndrome (ACS) (Table 1).
Patient characteristics.
| n | % | |
| Provenance | ||
| Hospitalization | 209 | 81.6 |
| Outpatient clinic | 47 | 18.4 |
| Age | ||
| <40 years | 9 | 3.5 |
| 40–59 years | 101 | 39.5 |
| 60–79 years | 143 | 55.9 |
| ≥80 years | 3 | 1.1 |
| Gender | ||
| Male | 195 | 76.2 |
| Female | 61 | 23.8 |
| Diagnosis | ||
| ACS | 167 | 65.3 |
| Post-angioplasty | 38 | 14.8 |
| Post-ICD implantation | 15 | 5.9 |
| Post-CABG | 16 | 6.3 |
| Angina | 13 | 5 |
| Heart failure | 6 | 2.3 |
| Post-CRT implantation | 1 | 0.4 |
| Total | 256 | |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; CRT: cardiac resynchronization therapy; ICD: implantable cardioverter-defibrillator.
The prevalence and changes in CV risk factors over the study period are presented in Tables 2–4.
Prevalence of cardiovascular risk factors.
| n | % | |
| BMI ≤25kg/m2 | 183 | 71.5 |
| BMI >25 to <30kg/m2 | 131 | 51.2 |
| BMI ≥30kg/m2 | 51 | 19.9 |
| WC 94–102cm (M) | 76 | 29.7 |
| WC >102cm (M) | 63 | 24.6 |
| WC 80–88cm (F) | 9 | 3.5 |
| WC >88cm (F) | 48 | 18.8 |
| Dyslipidemia | 190 | 74.2 |
| Hypertension | 160 | 62.5 |
| Smoking | 73 | 28.5 |
| Diabetes | 88 | 34.4 |
| Sedentary lifestyle | 119 | 46.5 |
BMI: body mass index; F: female; M: male; WC: waist circumference.
Comparison of cardiovascular risk factors at different assessments.
| Risk factor | Initial % (n) | 3-month % (n) | p | 6-month % (n) | p | 12-month % (n) | p |
| BMI ≥25kg/m2 | 71.5 (183/256) | 60.6 (155/256) | <0.001 | 59 (151/256) | <0.001 | 61.3 (157/256) | <0.001 |
| Obesity | 19.9 (51/256) | 15.2 (39/256) | 0.002 | 16 (41/256) | 0.013 | 16.4 (42/256) | 0.049 |
| WC >88cm (F) | 78.7 (48/61) | 72.1 (44/61) | 0.125 | 67.2 (41/61) | 0.016 | 63.9 (39/61) | 0.008 |
| WC >102cm (M) | 32.3 (63/195) | 20 (39/195) | <0.001 | 24.1 (47/195) | 0.006 | 24.6 (48/195) | 0.004 |
| Hypertension | 25.8 (66/256) | 4.3 (11/256) | <0.001 | 9.8 (25/256) | <0.001 | 7.8 (20/256) | <0.001 |
| TC ≥175mg/dl | 26.2 (67/256) | 12.5 (32/256) | <0.001 | 18.8 (48/256) | 0.069 | 18.4 (47/256) | 0.047 |
| LDL-C ≥100mg/dl | 55.1 (141/256) | 32 (82/256) | <0.001 | 36.3 (93/256) | <0.001 | 37.1 (95/256) | <0.001 |
| HDL-C ≤45mg/dl | 71.9 (184/256) | 38.2 (149/256) | <0.001 | 53.1 (136/256) | <0.001 | 52 (133/256) | <0.001 |
| Triglycerides ≥150mg/dl | 42.2 (108/256) | 22.7 (58/256) | <0.001 | 28.5 (73/256) | <0.001 | 25 (64/256) | <0.001 |
| Smoking | 28.5 (73/256) | 3.9 (10/256) | <0.001 | 7 (18/256) | <0.001 | 7 (18/256) | <0.001 |
| HbA1c ≥6.5% | 55.7 (49/88) | 30.7 (27/88) | <0.001 | 44.3 (39/88) | 0.093 | 38.6 (34/88) | 0.003 |
| Sedentary lifestyle | 46.5 (119/265) | 11 (4.3) | <0.001 | 8.6 (22/256) | <0.001 | 9.8 (25/256) | <0.001 |
F: females; HDL-C: high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol; M: males; TC: total cholesterol.
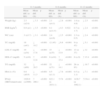
Changes in cardiovascular risk factors over 12-month follow-up.
| 0–3 months | 0–6 months | 0–12 months | |||||||
| Mean diff. (± SD) | Mean diff. (%) | p | Mean diff. (± SD) | Mean diff. (%) | p | Mean diff. (± SD) | Mean diff. (%) | p | |
| Weight (kg) | 2.5 (±2.8) | ↓ 3.3 | <0.001 | 2.1 (±4.1) | ↓ 2.8 | <0.001 | 1.9 (± 4.8) | ↓ 2.5 | <0.001 |
| BMI (kg/m2) | 0.9 (±1) | ↓ 3.5 | <0.001 | 0.1 (±11.5) | ↓ 0.3 | 0.922 | 0.7 (± 1.7) | ↓ 2.4 | <0.001 |
| WC (cm) | 3 (±3.7) | ↓ 3.1 | <0.001 | 2.4 (±4.6) | ↓ 2.5 | <0.001 | 2.3 (± 0.5) | ↓ 2.4 | <0.001 |
| TC (mg/dl) | 18 (±41) | ↓ 10.2 | <0.001 | 12 (45) | ↓ 6.8 | <0.001 | 9 (± 43) | ↓ 5.1 | <0.001 |
| LDL-C (mg/dl) | 19 (±34) | ↓ 17.6 | <0.001 | 15 (±35) | ↓ 13.9 | <0.001 | 13 (± 37) | ↓ 12 | <0.001 |
| HDL-C (mg/dl) | 5 (±10) | ↑ 12.8 | <0.001 | 6 (±10) | ↑ 15.4 | <0.001 | 6 (± 9) | ↑ 15.4 | <0.001 |
| TG (mg/dl) | 32 (±69) | ↓ 20.5 | <0.001 | 22 (±71) | ↓ 14.1 | <0.001 | 26 (± 83) | ↓ 16.7 | <0.001 |
| HbA1c (%) | 0.8 (±0.9) | ↓ 11.3 | <0.001 | 0.5 (±1.1) | ↓ 7.6 | <0.001 | 0.5 (± 1.1) | ↓ 7.1 | <0.001 |
| IPAQ (METs/min/week) | 1920.9 (±1909) | ↑ 206.1 | <0.001 | 622.1 (± 2031.1) | ↑174 | <0.001 | 1438.7 (± 1902.1) | ↑154.4 | <0.001 |
BMI: body mass index; diff.: difference; HDL-C: high density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low density lipoprotein cholesterol; METs: metabolic equivalents; SD: standard deviation; TC: total cholesterol; TG: triglycerides.
At admission, dyslipidemia was the most prevalent CV risk factor (74.2%) in the study population.
At the end of phase II of the CRP (at 3 months), there were mean reductions of 18mg/dl in TC (10.2%, p<0.001), 19mg/dl in LDL-C (17.6%, p<0.001) and 19mg/dl in TG (17.6%, p<0.001). As a result, the number of patients with TC >190mg/dl almost halved (from 26.2% to 12.5%, p<0.001), and the number with LDL-C >100mg/dl fell from 55.1% to 32% (p<0.001). Statistically significant reductions were maintained at 6 and 12 months in TC (6.8% and 5.1%, respectively, p<0.001), LDL-C (13.9% and 12%, p<0.001) and TG (14.1% and 16.7%, p<0.001), compared to the initial assessment values.
There was also a statistically significant increase in HDL-C levels at 3 months, the proportion of patients with HDL-C <45mg/dl decreasing from 71.9% to 38.2% (p<0.001), as well as at 6 and 12 months, an increase being maintained throughout the study period.
ObesityBMI >25kg/m2 was the second most common risk factor (71.5%) in the study population, 19.9% of patients being classified as obese (BMI ≥30kg/m2). At 3 months, there was a mean reduction of 2.5kg in weight (3.3%, p<0.001), 3.5% in BMI (p<0.001) and 3cm in WC (3.7%, p<0.001) in the overall population. Thus, the number of obese patients decreased by 19.9% to 15.2% (p=0.002) and the number of those with BMI ≥25kg/m2 decreased from 71.5% to 60.6% (p=0.003). However, although a statistically significant reduction in weight was observed at all assessments, the greatest weight loss was seen at the 3-month assessment, with only small reductions at subsequent assessments (2.8% at 6 months and 2.5% at 12 months in the overall population compared to initial values). With regard to BMI, the significant decrease observed at 3 months was virtually nonexistent at 6 months (0.3%, p=0.92), the change in BMI compared to initial values no longer being significant. However, there was a further statistically significant reduction at 12 months (2.4%, p<0.001), the number of patients with BMI ≥25kg/m2 decreasing from 71.5% to 61.3% (p<0.001) and the proportion of obese patients from 19.9% to 16.4% (p=0.049).
Initial assessment revealed that 78.7% of women had WC >88cm and 32.3% of men had WC >102cm. At 3 months, there was a statistically significant reduction in WC of 3cm (3.7%, p<0.001), which was less pronounced at 6- and 12-month assessment, although still statistically significant compared to initial values.
HypertensionOf the total population, 62.5% had a history of hypertension and initial assessment showed that 25.8% had high BP.
At 3 months, only 4.3% had uncontrolled hypertension (p<0.001), this figure rising to 9.8% (p<0.001) at 6 months and 7.8% (p<0.001) at 12 months. Thus, although the change was most pronounced at the end of phase II, statistical significance was maintained throughout follow-up.
DiabetesIn the study population, 34.4% of patients were diabetic and 55.7% of these had HbA1C >6.5% on initial assessment.
At 3 months, there was a mean reduction of 0.8% in HbA1C (11.3%, p<0.001) and the number of patients with HbA1C >6.5% almost halved (from 55.7% to 30.7%, p<0.001). There was a mean reduction of 0.5% in HbA1c (7.6%, p<0.001) at 6 months, and a further 0.5% (7.1%, p<0.001) at 12 months, still statistically significant changes.
SmokingOf the study population, 28.5% were smokers. At 3 months, only 3.9% of patients still smoked (p<0.001), an 86.3% reduction in the proportion of current smokers. At 6 months, 7% were smokers (p<0.001), with a similar percentage at 12 months (p<0.001).
Sedentary lifestyleAt the start of the study, 46.5% of individuals were sedentary, based on the scores obtained on the IPAQ. At 3 months, an increase of over 200% was observed in levels of weekly physical activity (2852.7 METs/min/week), as reported on the IPAQ, resulting in a reduction from 46.5% to 11% in the number of sedentary individuals (p<0.001). A mean increase of 174% (p<0.001) in weekly physical activity levels compared to the initial assessment was seen at 6- and 12-month assessments, the proportion classified as sedentary being 8.6% (p<0.001) and 9.8% (p<0.001), respectively.
DiscussionThe main aim of this study was to assess the long-term effects of an exercise-based CRP in CAD patients with regard to the modifiable CV risk factors of obesity, waist circumference, hypertension, dyslipidemia, diabetes, smoking and sedentary lifestyle.
A high proportion of our study population had dyslipidemia at admission (74.2%), which is in agreement with the literature.12,13 The relationship between TC, LDL-C and HDL-C levels and atherosclerosis is based on solid evidence. Triglycerides are also linked to greater risk of CAD, although their role in atherosclerotic CV disease is less well established.8,14 The risk associated with hypercholesterolemia is progressive and reducing TC by 10% lowers the incidence of CAD by 25% at five years.11 At the end of phase II of the CRP (3 months), the mean reduction in TC was over 10% and hence a significant reduction in CV risk can be assumed. However, there are conflicting results in the literature on the long-term effects of CRPs on lipid profile; some studies report that the benefits are not statistically significant in the long term,13 while others are in agreement with our results, with statistically significant benefits being maintained.12 Among the explanations that have been put forward for successful outcomes is the fact that some programs include nutritional support and educational sessions, leading to more consistent benefits. Both components were included in our CRP.
The prevalence of obesity is so high worldwide that the World Health Organization (WHO) considers it to be the global epidemic of the 21st century. The latest data for Portugal15 indicate a prevalence of overweight and obesity of 53.6%. The study population presented an even higher prevalence, reflecting their greater risk. Our results are in agreement with other studies that have also found a high rate of overweight and obesity in CAD patients.13
Various studies have shown that obesity alone increases CV mortality16 and that a 5% reduction in body weight reduces CV risk factors, while a 10% reduction has significant effects on lipid profile, hypertension control, insulin resistance and coagulation profile.17,18
It is now recognized that body fat, particularly visceral fat, is a metabolically active organ that synthesizes and releases into the bloodstream a variety of compounds that play an important role in cardiovascular hemostasis.19 In Portugal, most women have WC >88cm, while the proportion of men at similar risk is considerably lower (38% have WC >102cm).20 The data from our study follow the same pattern of a predominance of women with high WC.
At the end of phase II of the program, there had been a statistically significant reduction in weight-related parameters. Similar results are found in the literature,21,22 which confirms the efficacy of these programs in reducing risk factors, although the benefits obtained were significantly less at 6 and 12 months. Some studies have reported no statistically significant improvement in these parameters in the long term13; one possible reason is the absence of specific weight-loss components in CRPs.21,22 Our program included dietary advice by a nutritionist for all patients but no specific measures were adopted for obese patients in the exercise component.
As in most countries, hypertension is a major public health issue in Portugal, given its high prevalence (42%), low treatment rate (39%) and low percentage of controlled patients (11%).11
In our patient population, 62.5% had hypertension as a CV risk factor and on initial assessment 25.8% had high BP. Thus, most patients had controlled BP at the start of the CRP, which may be explained by the fact that most were under optimized antihypertensive therapy, having been referred following hospitalization in the cardiology department.
There is strong evidence of the clinical benefits of BP lowering in hypertensive patients,8,11 and the benefits of exercise-based CRPs in BP control are well established.23–25 The CRP had a positive impact in reducing hypertension throughout the study period, which was statistically significant at all assessments, and at 12 months only 7.8% had uncontrolled hypertension.
The WHO estimates that 300 million people worldwide will suffer from diabetes by 2025. In Portugal, 6.5% of the adult population has diabetes (over 300000 individuals), and this figure is undoubtedly an underestimate, since it does not include undiagnosed individuals.11 Diabetes is a well-established risk factor for CV disease; although diabetic patients are likely to have other conventional CV risk factors such as hypertension and dyslipidemia, the 3-5-fold increase in CV risk associated with diabetes appears to be independent of other risk factors.11
At the start of the study, 34.4% of patients had a history of diabetes, which was poorly controlled in over half (HbA1C >6.5%). This figure is well above that published for Portugal, which could reflect a higher prevalence of this risk factor in CAD patients or underdiagnosis of the disease in the general population. The benefits of exercise and CRPs on blood glucose levels are well documented in the literature26,27 and our study showed a reduction in almost half of the patients with poor glycemic control.
Smoking is the main factor in reduced life expectancy and is responsible for over 50% of avoidable deaths, half of which are due to atherothrombotic disease. In Portugal, 19.6% of the population over the age of 10 are daily smokers.11 The link between active and passive smoking and risk of developing CAD, cerebrovascular disease or peripheral vascular disease is well established. The incidence of myocardial infarction is six times higher in women and three times higher in men who smoke 20 cigarettes a day than in those who have never smoked.11 The harmful effects are cumulative, in terms of both daily consumption and duration of the habit (exposure time). The INTERHEART study28 showed a strong correlation between the number of cigarettes and risk of ACS – five cigarettes a day increases the risk by 38%, while 40 a day increases it by 900% – and halving daily consumption also halves ACS risk. Smoking cessation is thus a priority in cardiac rehabilitation, and is even more important in the presence of atherothrombotic disease and in patients undergoing invasive procedures such as coronary bypass surgery, angioplasty or vascular surgery.19 CRPs therefore represent an excellent opportunity to stress the importance of smoking cessation.
In our study, the percentage of smokers had fallen by more than half at the end of follow-up. These results are in agreement with other studies showing higher rates of smoking cessation among individuals participating in CRPs.29
Exercise is crucial for primary, secondary and tertiary prevention of most of the common chronic and/or degenerative diseases found in contemporary societies, especially those with western lifestyles, particularly with regard to the causes and consequences of atherosclerosis.11 In 1997, Portugal had the highest prevalence of sedentary lifestyles (87.8%) of 15 European Union countries.30
The number of sedentary patients fell dramatically over the course of our study and at 12-month follow-up, only 9.8% maintained a sedentary lifestyle; levels of weekly physical activity increased by 174%. These results are a further illustration of the importance of CRPs in these patients.
On assessment at the end of phase II, a considerable and statistically significant improvement was seen in all CV risk factors, which is in agreement with the results reported in the literature31–35 that show consistent benefits in these patients from exercise-based CRPs.
There was an overall improvement in the parameters related to control of CV risk factors, which remained statistically significant throughout the 12 months of follow-up, albeit with some reduction in the benefits obtained. This reduction was mainly seen at the 6-month assessment, which may be due to a waning of the initial level of motivation associated with the acute event. The relative improvement observed at 12 months may have resulted from the reinforcement of healthy behaviors and preventive measures (particularly in terms of diet and exercise) that took place at the 6-month assessment in view of the worsening of parameters compared to the favorable changes seen at the end of phase II.
The difficulty in maintaining such benefits is particularly evident in anthropometric data, since BMI was the parameter that showed the least change, the improvement seen in the first 3 months being virtually cancelled out in subsequent assessments. These results are similar to other studies that have reported greater difficulty in maintaining statistically significant differences for these parameters.13 The main reason suggested, as pointed out above, is the lack of specific preventive measures when prescribing exercise for obese patients.
We feel the study is important in that it assesses the long-term effects of CRPs in a sizable patient population, including changes in CV risk factors. There are few works in the literature presenting similar research, and most assess risk factors over a shorter time period and analyze a narrower range of parameters. This is also the first study in Portugal reporting CRP results at 12 months in a population of this size.
The lack of a control group is a limitation of the study, but since studies comparing usual care versus cardiac rehabilitation have consistently demonstrated the benefits of CRPs,35 we are confident that our results can be attributed specifically to participation in a CRP.
ConclusionCRPs are thus successful in treating patients with coronary disease, with benefits being maintained in subsequent months. Nevertheless, there is a reduction in these benefits once the hospital-supervised stage has ended, and it is therefore important to implement new strategies that will encourage patient compliance throughout the various phases of the program. It should be explained to patients that the benefits are often lost after phase II unless they adhere strictly to the preventive measures prescribed. Other interventions could be implemented, including a 3-monthly supervised exercise session accompanied by an educational component, in order to reinforce the basic concepts underlying prevention and health promotion, and monthly telephone calls and online communication to promote closer contact between the patient and the CRP team. It is also essential to make patients aware that they are responsible for their treatment and rehabilitation, since the latter will mainly depend on their own actions.
In our opinion, this study highlights the importance of these programs for secondary prevention of atherosclerotic disease and supports their applicability in clinical practice. There is thus a need to increase the referral rate to the CRPs currently available in Portugal and to establish new centers, in order to provide the care that is essential for full recovery after an acute event and for prevention of cardiovascular disease.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Magalhães, S, et al., Efeitos a longo prazo de um programa de reabilitação cardíaca no controlo dos fatores de risco cardiovasculares. Rev Port Cardiol 2013. http://dx.doi.org/10.1016/j.repc.2012.08.005.