We present a rare case of a levoatrial cardinal vein identified during the work-up of a patient with coarctation of the aorta. Early diagnosis and repair in the neonatal period prevented future manifestations of left-to-right shunt and the need for reoperations, in contrast with the later-age presentation of this congenital anomaly. An integrative approach was crucial for prompt detection, intraoperative confirmation and complete one-stage repair.
Os autores apresentam um caso raro de diagnóstico de uma veia levoatriocardinal identificada na avaliação incial de um recém-nascido com coartação da aorta. O diagnóstico e tratamento no período neonatal permitiram evitar as manifestações de shunt esquerdo-direito tardias e a necessidade de reintervenção no futuro. A abordagem multi-imagem integrada foi essencial para o diagnóstico precoce desta malformação congénita, confirmação intraoperatória e reparação completa num único procedimento.
Levoatrial cardinal vein is a rare congenital anomalous connection between the left atrium and the systemic venous system, classically described in association with severe left heart hypoplasia or obstruction, particularly mitral atresia and interrupted aortic arch.1 The levoatrial cardinal vein is usually regarded as a collateral pathway enabling pulmonary venous decompression and further attenuation of putative severe pulmonary venous hypertension in the context of a small, restrictive or absent atrial septal defect.2,3 This vessel has also been described in association with other more common congenital heart defects without left ventricular hypoplasia.4 As an isolated anomaly, levoatrial cardinal vein may be diagnosed in adulthood as a cause of left-to-right shunt and right heart overload.5,6
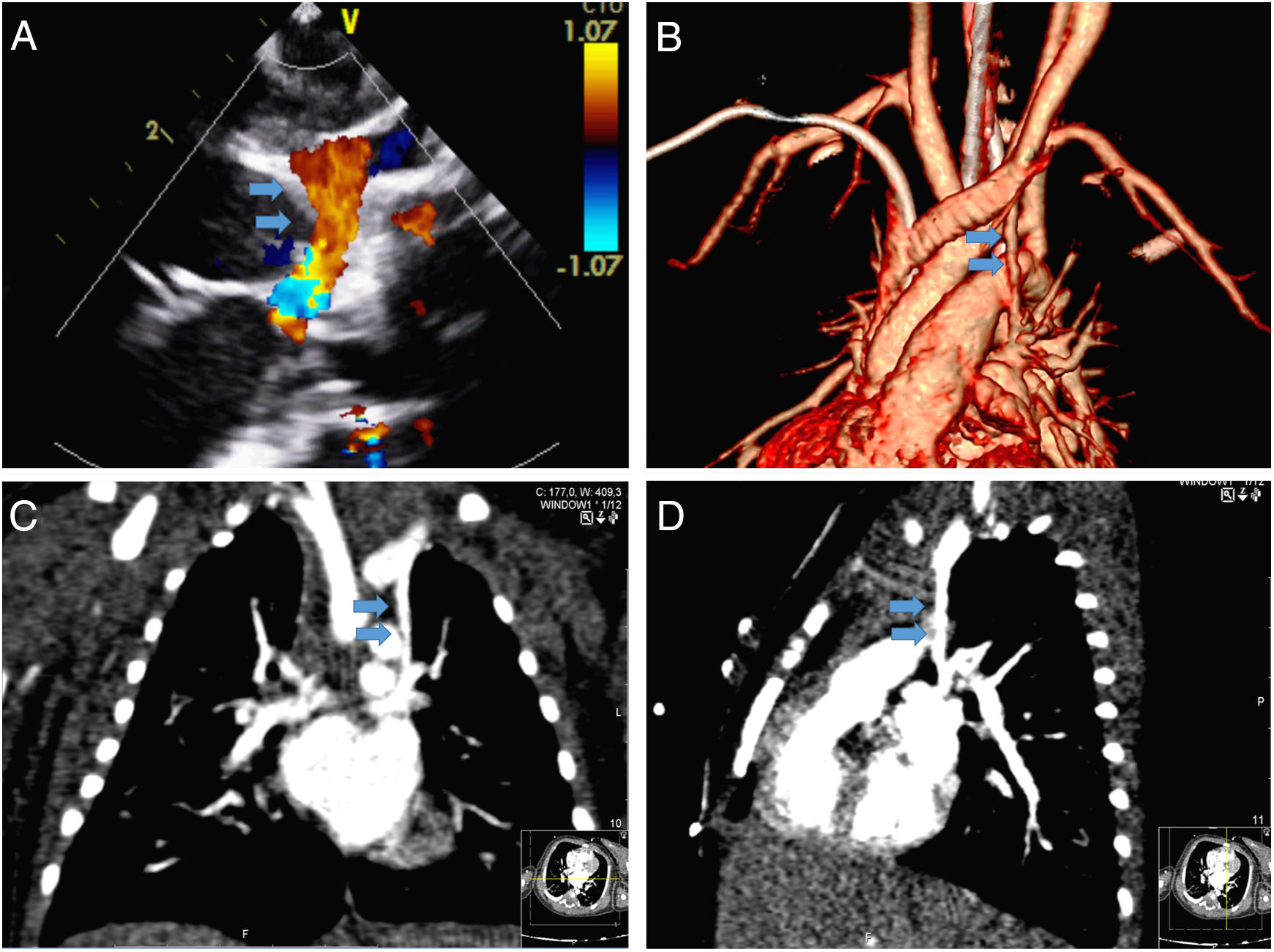
Case reportA two-day-old newborn, with birth weight of 3745 g, was admitted to the neonatal intensive care unit in cardiogenic shock. A diagnosis of ductal-dependent coarctation of the aorta was made and prostaglandin E1 was initiated. The echocardiographic examination also detected an anomalous left-sided vessel, with ascending flow, communicating with the brachiocephalic vein (Figure 1A and Video 1). At this time, the possibility of a vertical vein consistent with anomalous pulmonary venous drainage was considered, however the four pulmonary veins could be seen entering the left atrium, which excluded the differential diagnosis of a partial anomalous pulmonary venous connection. For further clarification, computed tomography (CT) angiography was performed, and three-dimensional CT reconstructions showed an anomalous vein connecting the left atrium to the brachiocephalic vein. Additionally, the left upper pulmonary vein appeared to be draining into the caudal portion of this vessel (Figure 1B-D and Video 2).
Sequential imaging approach to definitive diagnosis of a levoatrial cardinal vein in a neonate: pre-operative assessment. (A) Visualization of an abnormal ascending flow in the left superior vena cava position during the work-up echocardiogram for suspected coarctation of the aorta; (B-D) computed tomography confirming an abnormal venous connection between the left atrium and brachiocephalic vein (blue arrows).
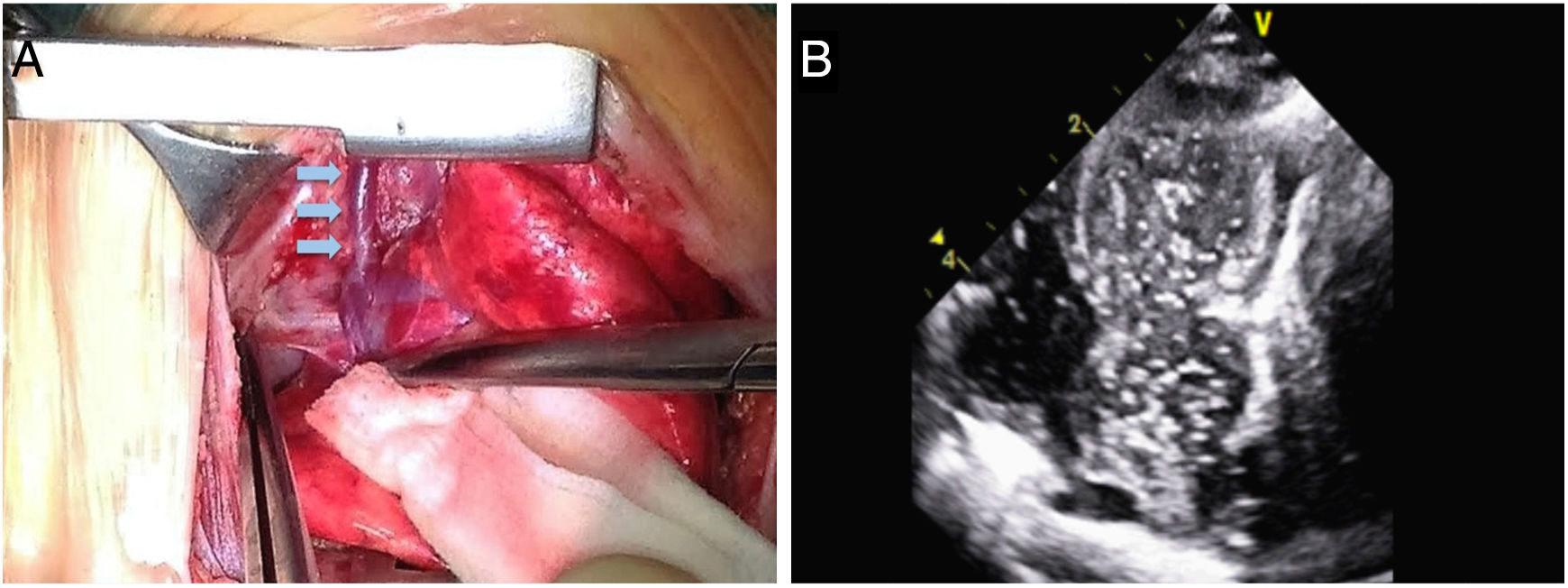
On the sixth day of life a left lateral thoracotomy was performed. After coarctation repair, the anterior aspect of the right pulmonary hilum was inspected. The suspected levoatrial cardinal vein was identified, isolated and cannulated and an intraoperative subcostal transthoracic echocardiogram was performed. The continuity of the levoatrial cardinal vein with the left atrium was confirmed by echocardiographic contrast injection (bubble test), which showed this was not an exclusive pathway for left superior pulmonary venous drainage (Figure 2A and B). Ligation of the levoatrial cardinal vein could then be safely performed above the connection of the pulmonary vein and below the brachiocephalic vein, redirecting the upper pulmonary venous return into the left atrium. The postoperative course was uneventful.
Sequential imaging approach to definitive diagnosis of a levoatrial cardinal vein in a neonate: intraoperative assessment. (A) Visualization of the levoatrial cardinal vein by direct inspection during surgery (blue arrows); (B) confirmation of the continuity of the levoatrial cardinal vein with the left atrium by echocardiographic contrast injection.
Levoatrial cardinal vein is a very rare congenital anomaly. It is an embryologic remnant of the fetal venous system and typically represents an escape drainage route of pulmonary venous blood in severe left-sided obstructive malformations. To our knowledge this is the first report of simultaneous correction in the neonatal period of a persistent levoatrial cardinal vein and severe extracardiac left-sided obstructive disease.
This abnormality may be easily missed in an echocardiographic assessment. The main differential diagnoses are a partial anomalous pulmonary vein connection, as the levoatrial cardinal vein can be confused with a vertical vein draining the left pulmonary veins, and persistent left superior vena cava. The latter can be differentiated on echocardiography by the direction of the flow, which is descending from the brachiocephalic vein into the coronary sinus in left superior vena cava and ascending in a levoatrial cardinal vein. The presence of four pathways of inflow into the left atrium on the echocardiogram excludes the differential diagnosis of a partial anomalous pulmonary venous connection. The normal anatomy of the four pulmonary veins can be further confirmed on CT angiography. Accurate differential diagnosis is essential for determination of the treatment strategy. This case report further illustrates the usefulness of intraoperative functional imaging as an adjuvant for diagnostic confirmation.
A levoatrial cardinal vein may be a source of persistent left-to-right shunt and cause clinical manifestations of chronic right heart volume overload later in life.
The multimodal imaging approach used in this case was of paramount importance for the correct diagnosis and prompt repair of this rare congenital anomaly in the early neonatal period. This straightforward procedure enabled us to eliminate the left-to-right shunt created by this pathway and to avoid future procedures. An integrative approach was crucial for prompt detection, intraoperative confirmation and complete one-stage repair.
Conflicts of interestThe authors have no conflicts of interest to declare.