We report a case of intrapericardial teratoma, which is a rare primary cardiac tumor usually found in newborns and infants. Cardiac teratomas can cause respiratory failure, large accumulations of pericardial fluid and cardiac compression leading to death in the intrauterine or neonatal period. The case described is rare because it is of a 16-year-old asymptomatic girl with an intrapericardial tumor as an incidental echocardiographic finding. Cardiac magnetic resonance imaging showed a complex pericardial cyst. Due to the potential for malignant evolution, she was referred for surgery to remove the tumor and a diagnosis of teratoma was confirmed by histopathology. Clinical follow-up had a good outcome.
Descrevemos um caso de teratoma intrapericárdico, tumor cardíaco primário raro, usualmente encontrado em neonatos e lactentes. O teratoma pode causar insuficiência respiratória, grande acúmulo de líquido pericárdico e compressão cardíaca, levando à morte no período intrauterino ou neonatal. O presente caso é raro, pois se trata de uma jovem de 16 anos, assintomática, portadora de tumor intrapericárdico em achado ecocardiográfico. As características à ressonância magnética cardíaca sugeriram cisto pericárdico complexo. Ela foi submetida à cirurgia para retirada do tumor e o diagnóstico de teratoma foi firmado pelo estudo histopatológico. O acompanhamento clínico mostrou-se de boa evolução.
Primary cardiac tumors are rare, with an incidence ranging from 0.001% to 0.28% in autopsy studies.1,2 Around 75% are benign, most frequently myxomas, which account for 50% of cases. The other 25% are malignant, mainly sarcomas (angiosarcomas, rhabdomyosarcomas and fibrosarcomas). Less frequently reported are malignant teratoma, mesothelioma and lymphoma.1,2
Intrapericardial teratoma is a benign cardiac tumor of which fewer than 100 cases have been reported since 1890.3,4 In these reports, most cases were in females (1.6:1)5 and in fetuses, newborns and infants. Clinical presentation is dramatic, with fetal hydrops and respiratory and hemodynamic instability at birth.3,4
Case reportG.D.A, aged 16 years, healthy and with no relevant personal history, was referred to the cardiology department for pre-participation sports evaluation. On physical examination she was asymptomatic, with regular cardiac rhythm, no abnormalities on auscultation and no clinical signs of congestion or organ enlargement. The resting electrocardiogram was normal, but the transthoracic echocardiogram revealed a hypoechogenic image adjacent to the right atrium measuring approximately 6.5 cm×3.7 cm, extracardiac, with partially heterogeneous content and no hemodynamic repercussion, which was suspected to be a pericardial cyst. Biventricular function was preserved and there were no other abnormalities.
Given the suspicion of a cyst, cardiac magnetic resonance imaging (MRI) was requested for further clarification. The exam was performed without contrast and revealed a clearly delimited round extracardiac formation with the appearance of a cyst in contact with the lateral wall of the right atrium, without impairing filling and not invading adjacent structures. It measured 7.9 cm×8.6 cm×4.3 cm in its largest dimensions and had thin walls, multiple compartments in its interior and heterogeneous content.
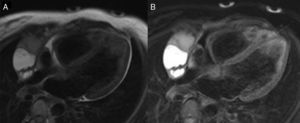
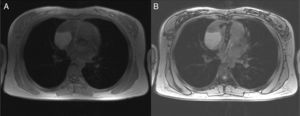
In view of the latter finding, the study also included double inversion recovery (DIR), DIR with fat saturation and in-phase and out-of-phase sequences. T2-weighted DIR sequences showed a mainly hyperintense signal in the contents of the cyst, which suggested a high-fat or bloody/high-protein liquid component. DIR imaging with fat saturation revealed a hypersignal that confirmed a liquid component (Figure 1). However, small hypointense areas were also visualized in its interior, suggesting a different type of tissue. A small but clearly visible hypointense area was detected in out-of-phase sequences, suggesting the presence of intravoxel fat, confirming different types of tissue in the interior of the cyst (Figure 2).
Cardiac magnetic resonance imaging with double inversion recovery (A) and double inversion recovery with fat saturation (B), showing areas of hyperintensity and hyposignal suggesting possible liquid, fat or bloody/high-protein components inside the compartments of the complex pericardial cyst.
Possible diagnoses were thus complex pericardial cyst, lesion of thymic origin, or bronchogenic cyst.
Given the findings suggestive of a complex cyst composed of different tissue types, which could include teratoma or mesothelioma, the patient was referred for resection, due to the potential for malignant evolution. Video-assisted thoracoscopic surgery was performed and the surgical specimen was sent for analysis. The final diagnosis was intrapericardial teratoma. The patient's postoperative course was uneventful.
DiscussionCardiac teratomas are rare and although they do occur in adulthood,3,4 they account for less than 1% of cardiac tumors in adults and there have been few cases reported in the literature.6–9 Most occur in newborns and children (around 15% of cardiac tumors in this age-group).4 They are slightly more common in females (1.6:1).5 The peak incidence in adults at presentation is between the second and third decades of life.6
Most primary cardiac teratomas emerge from the base of the heart into the anterior mediastinum and are found in the pericardium; intramyocardial forms are rare.6 They are usually adjacent to the right atrium, attached by a stalk to the root of the pulmonary artery and aorta. Blood supply is usually from the vasa vasorum, although it may occasionally be from the coronary arteries.
Intrapericardial teratomas can assume large proportions, measuring up to 15 cm in their greatest diameter. They are pear-shaped, usually smooth-surfaced and lobulated. When opened, they present numerous multiloculated cysts and intervening solid areas. Microscopically, respiratory and gastrointestinal epithelium, cartilage, bone, neural tissue and other tissues originating from all three germ layers are found. These features distinguish teratomas from intrapericardial bronchogenic cysts, which only contain tissues of gastrointestinal and respiratory origin. Unlike ovarian teratomas, intrapericardial teratomas do not usually contain hair, sebaceous glands or keratinizing squamous epithelium. Like all teratomas, they have the potential for malignant transformation (around 15%).10 Although this evolution is uncommon, the possibility should be assessed in all cases.11
The most striking symptom is severe respiratory failure, usually secondary to pulmonary compression caused by the swelling of the pericardium due to the tumor and by the pericardial effusion that often accompanies teratomas.9 Rupture of the cystic areas into the pericardium, due to the multicystic nature of the tumor, associated with obstruction of venous return of the lymphatic system to the thoracic duct, leads to the development of pleural, peritoneal and pericardial effusions.
Cardiac function may also be impaired due to varying degrees of compression of the heart, great vessels, or superior vena cava by the tumor, which contributes to the severity of cardiorespiratory compromise. Direct compression of the trachea or esophagus is uncommon, and symptoms tend to be less severe in older patients, in whom the tumor may be an incidental radiographic finding.
Differential diagnosis should include tumors of the anterior mediastinum, enlarged thymus, other causes of pericardial effusion, and congenital cardiac defects.11 Differentiation from bronchogenic cyst is only possible on microscopic examination.4 Cardiac tumors such as rhabdomyoma, fibroma and myxoma are more common, but are found in the atria or ventricles, and are thus easy to distinguish from pericardial masses. Differential diagnosis between teratoma and other intrapericardial masses such as hemangioma or mesothelioma is not possible in utero.4
Chest X-ray in anteroposterior view shows an increased cardiac area and, in profile view, may show the trachea compressed by the anterior mediastinal mass, a finding that cannot be attributed to a normal thymus.
On transthoracic echocardiography, the presence of a large cardiothymic image or of mediastinal widening with pericardial effusion is indicative of an intrapericardial teratoma, and should prompt further diagnostic study.11
Surgical treatment is mandatory as soon as the diagnosis of teratoma is established,10 since despite its benign nature, there is a possibility of malignant transformation. Furthermore, if the tumor is not excised there is the risk of compression of adjacent structures, which may cause arrhythmias or pericardial effusion,9 as well as infection.6,9
Median sternotomy is the surgical access of choice and is performed without extracorporeal circulation, since the points of attachment of the tumor to the heart, especially to the ascending aorta, can be detached without difficulty. Resection should be complete, since otherwise a pericardial effusion may form with hemodynamic consequences, and careful review to detect possible other teratomas is essential.8,9
If the histological study reveals signs of malignancy, radiotherapy or chemotherapy can be associated with surgical resection.10
The case presented has some unusual features. Most intrapericardial teratomas are found in fetuses or newborns and when they occur in adults, this is usually in the second or third decades of life.6 This case, however, is of an asymptomatic 16-year-old girl, and resulted from an incidental diagnosis by transthoracic echocardiography of a pericardial cyst adjacent to the right atrium.
As described in another published case report,8 the role of transthoracic needle biopsy in diagnosis is controversial. If adopted, it should be discussed in a multidisciplinary approach, since it can cause serious complications and the material obtained may be insufficient for analysis.
Cardiac MRI was particularly important in our case, since it revealed a cyst with complex characteristics (septated and with heterogeneous content), which led to the hypothesis of a teratoma, followed by definitive diagnosis and surgical resection. There are two case reports in the literature in which the mass was assessed by computed tomography,8,9 but the advantage of MRI is its ability to characterize different tissue types. In T2-weighted DIR and DIR with fat saturation sequences, a mainly hyperintense signal was seen inside the compartments of the cyst, representing bloody or high-protein liquid content. However, a small area with hypointense signal was also observed in the middle of the hypersignal that was difficult to characterize. Further investigation with in-phase and out-of-phase sequences provided better definition of the small hypointense area, identifying it as intravoxel adipose tissue.
In-phase and out-of-phase sequences are routinely used to characterize microscopic areas of adipose tissue. The different hydrogen bonds in fat (CH2) and in water (H2O) cause protons to precess at different rates. With this sequence, usually a spoiled echo gradient, the image is acquired when the protons in fat and water are spinning in phase with each other (echo time 4.2 ms at 1.5 T) and out of phase (echo time 2.1 ms at 1.5 T). If microscopic fat is present, its signal is canceled out on the out-of-phase images.12,13 These techniques are mainly used to characterize tumors that contain intravoxel fat, such as hepatocellular tumors, adrenal adenoma, and clear-cell renal tumors. When first introduced they were widely used to quantify hepatic steatosis.12,13
In-phase and out-of-phase sequences were important in the case presented as they characterized different tissue components in the interior of the pericardial cyst, demonstrating its fat content and thus enabling the patient to be referred for surgery and providing the final pathological diagnosis.
ConsentThis case report was approved by the institution's ethics committee, reference HSL-RC 2015-03, on October 8, 2015.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Moura Garcia A, Nery Dantas Junior R, Chi CK, Rodrigues Parga J. Diagnóstico incidental tardio de teratoma intrapericárdico – relato de caso. Rev Port Cardiol. 2017;36:571.