Implementing integrated systems for emergency care of patients with acute ischemic stroke helps reduce morbidity and mortality. We describe the process of organizing and implementing a regional system to cover around 3.7 million people and its main initial results.
MethodsWe performed a descriptive analysis of the implementation process and a retrospective analysis of the following parameters: number of patients prenotified by the pre-hospital system; number of times thrombolysis was performed; door-to-needle time; and functional assessment three months after stroke.
ResultsThe implementation process started in November 2005 and ended in December 2009, and included 11 health centers. There were 3574 prenotifications from the prehospital system. Thrombolysis was performed in 1142 patients. The percentage of patients receiving thrombolysis rose during the study period, with a maximum of 16%. Median door-to-needle time was 62 min in 2009. Functional recovery three months after stroke was total or near total in 50% of patients.
ConclusionsThe regional system implemented for emergency care of patients with acute ischemic stroke has led to health gains, with progressive improvements in patients’ access to thrombolysis, and to greater equity in the health care system, thus helping to reduce mortality from cerebrovascular disease in Portugal. Our results, which are comparable with those of international studies, support the strategy adopted for implementation of this system.
A implementação de sistemas integrados de resposta emergente ao doente com acidente vascular cerebral agudo contribuem para a redução da sua morbimortalidade. Descreve-se o processo de implementação de um sistema regional que assegura resposta a cerca de 3,7 milhões de cidadãos e os seus principais resultados iniciais.
MétodosRealiza-se uma análise descritiva do processo de implementação do sistema regional e uma análise retrospetiva dos parâmetros avaliados. Os parâmetros analisados foram: evolução do número de doentes com suspeita de acidente vascular cerebral orientados pelo sistema de emergência médica pré-hospitalar; número de trombólises realizadas; evolução anual do número de trombólises realizadas; tempo porta-agulha; avaliação funcional aos três meses pós-acidente vascular cerebral.
ResultadosA implementação do sistema regional integrado de resposta emergente ao doente com acidente vascular cerebral agudo iniciou-se a 1 de novembro de 2005 e ficou concluído em dezembro de 2009, com 11 unidades de saúde. Foram orientados pelo sistema de emergência médica pré-hospitalar 3.574 doentes. A trombólise endovenosa foi realizada em 1.142 doentes. A percentagem de doentes submetidos a trombólise aumentou durante o período, com um valor máximo de 16%. A mediana do tempo porta-agulha foi de 62 minutos em 2009. A recuperação funcional aos três meses foi total ou quase total em 50% dos casos.
ConclusõesO sistema regional de resposta emergente ao doente com acidente vascular cerebral agudo implementado na região Norte traduziu-se em ganhos em saúde, com progressivo maior acesso dos doentes a técnicas eficazes de tratamento e uma melhoria progressiva da equidade do sistema, contribuindo para a redução da mortalidade por doença cerebrovascular verificada no país no período em apreço. Os resultados alcançados, que podem ser favoravelmente comparados com outros internacionais, corroboram a estratégia adotada.
Morbidity and mortality from stroke continue to be very high.1–3 The development and implementation of integrated local, regional or national systems to provide emergency care for acute ischemic stroke is essential to improve the prognosis of these patients and is the best way to achieve overall improvements in clinical outcomes. Such systems should include campaigns to raise public awareness of the signs of stroke, emergency triage by telephone, emergency pre-hospital services for rapid initial stabilization and transport, a policy of bypassing health centers without specific facilities for treatment of acute stroke victims, the implementation of protocols for rapid identification of patients with acute stroke during hospital triage, the formation of emergency hospital teams for assessment and treatment of stroke victims, and the establishment of clinical assessment and treatment protocols, and priority routing for access to imaging facilities, laboratory testing, and procedures to restore vascular patency.2–11
We describe the process of implementing a regional system to cover around 3.7 million people and the main results of its initial period of operation.
MethodsThe authors present a descriptive analysis of the process of implementing a fast-track regional system to provide emergency care for stroke patients (“Via Verde do AVC”) both outside and inside the hospital, which began operating in November 2005. We also present a retrospective analysis of the following parameters, assessed up to 31 December 2009: number of patients prenotified by the prehospital system; total number of patients with stroke and number with ischemic stroke treated in each health center; the number of times thrombolysis was performed each year; door-to-needle time; and functional assessment three months after stroke, using the Rankin scale.
Health centers that fulfilled all of the following requirements were included in the system: the pre-hospital emergency system was aware that the center was able to receive and treat acute ischemic stroke patients, and had a direct telephone link to the emergency medical team of the Via Verde fast-track system; members of the pre-hospital emergency response team had had specific training, including in recognizing the signs of stroke, deciding whether the patient should be handled by the Via Verde, and awareness of the association between time since stroke onset and prognosis; the health center had a Via Verde emergency team on call 24 hours a day, 365 days a year; computed tomography (CT) imaging and reporting were permanently available; there was a permanently available hemostasis and thrombosis laboratory; fibrinolytic drugs could, when indicated, be administered immediately and monitored; there were ward beds designated for acute stroke patients; and there was a system for data collection, monitoring and local auditing of the system.
The implementation process was coordinated by the Regional Health Authority of the North region and the North branch of INEM.
Data on pre-hospital emergencies were obtained from INEM, while data on the health centers and patients’ neurological and functional status three months after stroke were obtained from the health centers where the patients were admitted and treated.
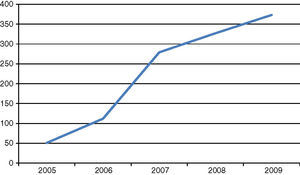
ResultsImplementation of the system began on November 1, 2005. It initially included three health centers in the region, but was subsequently extended to cover 11 centers by December 2009 (Table 1).
Date of implementation of the Via Verde fast-track system in different health centers.
| Institution | Beginning of operation |
| Centro Hospitalar de S. João | November 1, 2005 |
| CH do Porto | November 1, 2005 |
| CH Entre-o-Douro e Vouga | November 1, 2005 |
| Hospital de Braga | February 5, 2007 |
| CH Trás-os-Montes e Alto Douro | March 14, 2007 |
| ULS Matosinhos | June 1, 2007 |
| CH VN Gaia/Espinho | March 3, 2008 |
| ULS Nordeste | January 19, 2009 |
| Centro Hospitalar de Guimarães | April 20, 2009 |
| CH Tâmega e Sousa | June 22, 2009 |
| ULS Alto Minho | December 2, 2009 |
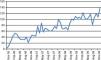
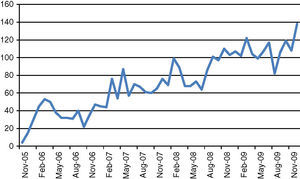
The growth in numbers of patients prenotified by INEM's Via Verde system was paralleled by the increased number of health centers able to deal with acute stroke patients and hence improved access to specialized care (Figure 1). Over the four-year study period, a total of 3574 patients with suspected acute stroke were prenotified by the pre-hospital system, 1311 (37%) of them in the last year under analysis (2009), demonstrating the progressive and sustained growth in use of the system.
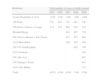
During the study period a total of 35439 cases of stroke, 16242 (46%) of them ischemic, were diagnosed and treated in the health centers participating in the system (Tables 2 and 3).
Total numbers of cases of stroke treated in participating health centers, by year and by center.
| Institution | Total number of cases of stroke treated | ||||
| 2005 | 2006 | 2007 | 2008 | 2009 | |
| Centro Hospitalar S. João | 1238 | 1283 | 1402 | 1366 | 1469 |
| CH Porto | 722 | 802 | 719 | 667 | 736 |
| CH Entre-o-Douro e Vouga | 514 | 678 | 668 | 620 | 578 |
| Hospital Braga | 848 | 867 | 779 | ||
| CH Trás-os-Montes e Alto Douro | 497 | 507 | 466 | ||
| ULS Matosinhos | 260 | 455 | 456 | ||
| CH VN Gaia/Espinho | 655 | 746 | |||
| ULS Nordeste | 156 | ||||
| CH Alto Ave | 867 | ||||
| CH Tâmega e Sousa | 801 | ||||
| ULS Alto Minho | 735 | ||||
| Total | 4479 | 4769 | 9248 | 7145 | 9798 |
Total numbers of cases of ischemic stroke treated in participating health centers, by year and by center.
| Institution | Total number of cases of ischemic stroke treated | ||||
| 2005 | 2006 | 2007 | 2008 | 2009 | |
| Centro Hospitalar S. João | 932 | 954 | 1000 | 970 | 1081 |
| CH Porto | 427 | 493 | 412 | 427 | 433 |
| CH Entre-o-Douro e Vouga | 312 | 407 | 420 | 404 | 410 |
| Hospital Braga | 590 | 608 | 585 | ||
| CH Trás-os-Montes e Alto Douro | 396 | 401 | 466 | ||
| ULS Matosinhos | 196 | 329 | 346 | ||
| CH VN Gaia/Espinho | 548 | 641 | |||
| ULS Nordeste | 100 | ||||
| CH Alto Ave | 693 | ||||
| CH Tâmega e Sousa | 623 | ||||
| ULS Alto Minho | 638 | ||||
| Total | 1671 | 1854 | 3014 | 3687 | 6016 |
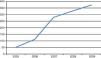
Thrombolysis was performed in a total of 1142 patients, 112 in 2006 and 373 in 2009, an increase of 333% (Figure 2).
The percentage of patients with ischemic stroke admitted to the participating centers who underwent thrombolysis generally rose, with a maximum of 16% in Centro Hospitalar Entre-o-Douro e Vouga. It should be noted that the figures presented refer to the entire calendar year, and the fact that some centers joined the system late in the year would have affected this percentages. This explains, for example, why the proportion of patients diagnosed with ischemic stroke receiving thrombolysis in 2009 was only 0.31% in ULS de Alto Minho, which only joined the system on December 2 of that year. Analysis of the ischemic stroke patients undergoing thrombolysis in the seven hospitals which were fully integrated in the system at the beginning of 2009 shows a mean percentage of 8.75%, compared to 5.88% in 2006 (Table 4).
Percentage of patients with ischemic stroke receiving thrombolysis, by year and by center.
| Institution | Ischemic stroke patients receiving thrombolysis (%) | ||||
| 2005 | 2006 | 2007 | 2008 | 2009 | |
| Centro Hospitalar S. João | 3.11 | 6.5 | 9.3 | 10.4 | 8.88 |
| CH Porto | 3.51 | 5.0 | 8.25 | 4.44 | 6.46 |
| CH Entre-o-Douro e Vouga | 2.24 | 6.14 | 14.52 | 15.84 | 14.15 |
| Hospital Braga | 8.30 | 9.53 | 8.89 | ||
| CH Trás-os-Montes e Alto Douro | 8.84 | 9.97 | 8.97 | ||
| ULS Matosinhos | 3.57 | 7.29 | 10.69 | ||
| CH VN Gaia/Espinho | 3.83 | 6.08 | |||
| ULS Nordeste | 6.0 | ||||
| CH Alto Ave | 1.44 | ||||
| CH Tâmega e Sousa | 1.60 | ||||
| ULS Alto Minho | 0.31 | ||||
Door-to-needle times improved in all the participating centers over the study period, with reduced median times in most cases. The overall median time was 62 min in 2009, which would be 60 min if one center with a much longer time (112 min) is excluded (Table 5).
Door-to-needle time, in min.
| Institution | 2005 | 2006 | 2007 | 2008 | 2009 |
| Centro Hospitalar S. João | 103 | 83 | 77 | 72 | 65 |
| CH Porto | 66 | 58 | 53 | 63 | 73 |
| CH Entre-o-Douro e Vouga | 60 | 50 | 45 | 41 | 43 |
| Hospital Braga | – | – | 50 | 50 | 53 |
| CH Trás-os-Montes e Alto Douro | – | – | 85 | 90 | 87 |
| ULS Matosinhos | – | – | 60 | 60 | 60 |
| CH VN Gaia/Espinho | – | – | – | 59 | 57 |
| ULS Nordeste | – | – | – | – | 60 |
| CH Alto Ave | – | – | – | – | 76 |
| CH Tâmega e Sousa | – | – | – | – | 112 |
| ULS Alto Minho | – | – | – | – | – |
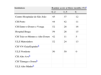
Neurological and functional recovery was assessed three months after stroke using the Rankin scale. Around 50% of patients receiving thrombolysis had a Rankin score of 0–2, while mortality was 11–14% (Table 6).
Assessment of functional recovery three months after stroke using the Rankin scale.
| Institution | Rankin score at three months (%)a | ||
| 0–2 | 3–5 | 6 | |
| Centro Hospitalar de São João | 45 | 37 | 12 |
| CH Porto | 44 | 42 | 11 |
| CH Entre-o-Douro e Vouga | 52 | 28 | 16 |
| Hospital Braga | 59 | 26 | 15 |
| CH Trás-os-Montes e Alto Douro | 42 | 11 | 5 |
| ULS Matosinhos | 52 | 24 | 13 |
| CH VN Gaia/Espinhob | |||
| ULS Nordeste | 50 | 50 | 0 |
| CH Alto Aveb | |||
| CH Tâmega e Sousab | |||
| ULS Alto Minhob | |||
Mortality from cerebrovascular disease in Portugal remains very high; the country has one of the highest standardized mortality rates from stroke per 100000 population in Europe. However, recent years have seen a significant decrease in this indicator, with deaths in men falling from 115 per 100000 population in 2004 to 69 in 2011, while the equivalent figure for women fell from 90 to 54.1
Part of this reduction may be due to the implementation of regional emergency care systems such as the one for stroke patients in the North region of Portugal, described here, as suggested by recent studies.2–5,10,12
There is evidence that such systems, focusing on the signs and symptoms of acute stroke and the specific requirements for emergency treatment, are able to direct patients to health centers with the facilities to provide comprehensive care for these patients, as well as prenotifying the center before their arrival, thus reducing door-to-needle time and increasing the number of patients receiving thrombolysis, which in turn improves prognosis and reduces mortality.2–6,13,14 This is corroborated by our findings, which show a progressive increase in the number of patients with access to thrombolysis as more health centers gained the capability to provide emergency care for acute stroke patients. The decentralized, regional strategy that has been followed, not restricted to large hospitals, as well as extension of the therapeutic window from 3 to 4.5 hours, means that the entire population of the North region, even in rural areas, is now covered by the system, thereby improving equity in the health care system. It was decided to upgrade the facilities and organization of emergency departments that were already classified as ‘general’ or ‘medical and surgical’, since these already had greater capacity and the technical and human resources needed for the diagnosis and treatment of acute stroke patients, such as permanently available CT imaging and neurology departments.
Another key factor in regional emergency care systems is the establishment of acute stroke teams on call 24 hours a day in participating centers. These teams are responsible for the initial assessment of patients prenotified by the pre-hospital system, providing rapid and effective diagnostic testing, and ensuring that thrombolysis is administered when appropriate.15
Recent studies show that in the USA and Europe, only 4–10% of ischemic stroke patients receive thrombolysis, while in Canada and Australia the figures are 2% and 3%, respectively.11,13,16 Our findings are generally similar, with most centers in the regional system equaling or, in some cases, regularly surpassing these figures. These results may be partly due to the greater number of hospitals included in the network implemented in the North region, which has enabled more patients to be treated within the therapeutic window and thus be more likely to receive thrombolysis, as well as to prenotification by the pre-hospital system, the establishment of systems to identify patients with acute stroke during triage in the emergency department, the availability of acute stroke teams in emergency departments, and the introduction of protocols for priority routing in the emergency department and in diagnostic exams.
In a recent study involving over 25000 acute stroke patients in over 1000 hospitals between 2003 and 2009, median door-to-needle time was 78 min.17 It is, however, recommended in some countries that this figure should be kept below 60 min, given the demonstrated association between prognosis and time between stroke onset and thrombolysis.5,17 A series of recommendations have been put forward to minimize this delay, including prenotification by the pre-hospital emergency system and activation of acute stroke teams, specific protocols for triage and priority routing of stroke patients in the emergency department, immediate access to CT and/or magnetic resonance imaging, rapid access to thrombolytic agents in the emergency department, and continuous monitoring and auditing of the system.2–6,12,14,15 The good results of the acute stroke emergency response system implemented in the North region of Portugal may be due to the fact that most of these recommendations were followed. It should be noted that the establishment of this system did not require major investment, but merely dissemination of information, training of all personnel involved, and organizational improvements.
The considerable efforts made by the participating health centers in order to meet the demanding requirements of the Via Verde fast-track system, as well as the exemplary commitment and dedication of the medical personnel involved in this pioneering project, have been essential for its success.
ConclusionThe acute stroke emergency response system implemented in the North region, in operation since the end of 2005, has led to health gains, with progressively greater access to effective treatment and improvements in the equity of the health care system, and has contributed to the reduction in mortality from cerebrovascular disease seen in Portugal during the period under analysis. Our findings also underline the importance of implementing most of the guidelines on this subject, particularly prenotification by the pre-hospital emergency system, early identification of acute stroke patients by triage staff in the emergency department, the establishment of dedicated teams available in the emergency department to assess and treat stroke patients, and rapid access to diagnostic exams and thrombolysis when appropriate. All these recommendations, which when properly implemented lead to health gains, are essentially organizational improvements and do not require major investment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Soares-Oliveira M, Grupo de AVC da Administração Regional de Saúde do Norte, Araújo F. Implementação de um sistema regional de resposta emergente ao acidente vascular cerebral: primeiros resultados. Rev Port Cardiol. 2014;33:329–335.