The elderly population admitted for acute myocardial infarction is increasing. This group is not well studied in international trials and is probably treated with a more conservative approach.
ObjectivesTo evaluate the presentation and treatment of myocardial infarction according to age, particularly in very elderly patients.
MethodsWe studied 1242 consecutive patients admitted with acute myocardial infarction, assessing in-hospital, 30-day and one-year mortality during follow-up for each age-group. Patients were divided into four groups according to age: <45 years (7.6%); 45–64 years (43.3%); 65–74 years (23.4%); and ≥75 years (25.7%).
ResultsElderly patients had a worse risk profile (except for smoking), more previous history of coronary disease and a worse profile on admission, with the exception of lipid profile, which was more favorable. With regard to treatment of the elderly, although less optimized than in other age-groups, it was significantly better compared to other registries, including for percutaneous coronary angioplasty. Both complications and mortality were worse in the older groups. In elderly patients (≥75 years), adjusted risk of mortality was 4.9–6.3 times higher (p<0.001) than patients in the reference age-group (45–64 years). In these patients, the independent predictors of death were left ventricular function and renal function, use of beta-blockers being a predictor of survival.
ConclusionsElderly patients represent a substantial proportion of the population admitted with myocardial infarction, and receive less evidence-based therapy. Age is an independent predictor of short- and medium-term mortality.
A população idosa admitida com enfarte continua a aumentar, sendo este grupo mal estudado nos ensaios internacionais e provavelmente tratados de uma forma mais conservadora.
ObjectivosAvaliar a apresentação e tratamento do enfarte do miocárdio de acordo com a idade, em particular nos mais idosos.
MétodosEstudo de 1242 doentes consecutivos admitidos por enfarte agudo do miocárdio. Ava-liámos a ocorrência de mortalidade intra-hospitalar, aos 30 dias e ao 1.° ano de seguimento em relação ao respectivo grupo etário. Os doentes foram caracterizados em quatro grupos etário: < 45 anos (7,6%); 45 – 64 anos (43,3%), 65 – 74 anos (23,4%) e ≥ 75 anos (25,7%).
ResultadosOs doentes mais idosos têm um pior perfil de risco (excepto tabagismo), mais história prévia de doença coronária e pior perfil de apresentação, exceptuando-se o perfil lipídico que é mais favorável. Relativamente ao tratamento dos idosos, este não foi tão optimizado comparativamente com outros grupos etários, embora seja melhor do que o reportado em outros registos, incluindo a realização de angioplastia coronária. Quer as complicações, quer as diferentes mortalidades consideradas foram piores no grupo com mais idade. Nos indivíduos com ≥ 75 anos, o risco de mortalidade ajustado é 4,9 – 6,3 vezes superior (p<0,001) comparativamente com o grupo etário de referência dos 45-64 anos. Nos indivíduos mais idosos, os principais factores predizentes independentes de mortalidade são a função ventricular esquerda e função renal, sendo a utilização de bloqueadores beta factor predizente de sobrevivência.
ConclusãoOs idosos representam uma percentagem importante da população admitida por enfarte, recebendo menos terapêuticas com evidências científicas, sendo a idade um factor predizente independente de mortalidade a curto e médio-prazo.
The elderly have become the fastest growing patient population in recent years and represent a substantial proportion of those admitted for acute coronary syndrome (ACS), coronary artery disease being a major cause of death in this age-group.1–3 Although the evidence is not as strong since the elderly are usually under-represented in most randomized clinical trials, they are a high-risk population and ACS treatment should be the same as for other age-groups. Nevertheless, various international studies have shown that the therapeutic approach tends to be more conservative in elderly patients.4–7
The aim of the present study was to evaluate the form of presentation and treatment of myocardial infarction (MI) according to age, particularly in very elderly patients, as well as to identify predictors of short- and medium-term mortality in this age-group.
MethodsWe performed a retrospective analysis of 1242 consecutive patients with MI admitted to the intensive care unit of a tertiary center, who were included in a prospective single-center ACS registry between January 2005 and December 2008. All patients included were aged ≥18 years and were alive at the time of admission. They presented symptoms suggestive of acute myocardial ischemia and at least one of the following: electrocardiographic alterations consistent with ACS and/or elevated biomarkers of myocardial necrosis. Cases were classified as ST-elevation MI or non-ST elevation ACS (infarction or unstable angina).
The following variables were analyzed: demographic characteristics, coronary risk factors, previous heart disease, laboratory data at admission, in-hospital treatment and complications (cardiopulmonary arrest, stroke or transient ischemic attack, cardiogenic shock, mechanical complications – septal or free wall rupture, cardiac tamponade or acute mitral regurgitation – and major bleeding). Major bleeding was defined as intracranial, life-threatening or requiring transfusion. All surviving patients were followed up by telephone at 30 days and at one year, information being obtained in 99.6%. Overall in-hospital, 30-day and one-year mortality was assessed.
The patients were divided into groups according to their age at admission: <45 years (n=94); 45–64 years (n=538); 65–74 years (n=291); and ≥75 years (n=319).
Statistical analysisContinuous variables are expressed as means±standard deviation and were compared using ANOVA or the Kruskal–Wallis test if they presented a non-normal distribution. Those with a non-normal distribution (total and HDL cholesterol, triglycerides, admission blood glucose, admission creatinine and peak CK) were transformed logarithmically to improve their normality and used in the subsequent statistical analysis. Categorical variables are expressed as percentages and were compared using the chi-square test or Fisher's exact test as appropriate. Predictors of mortality were determined by univariate and multivariate logistic regression analysis. A value of p<0.05 was considered statistically significant. The statistical analysis was performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA).
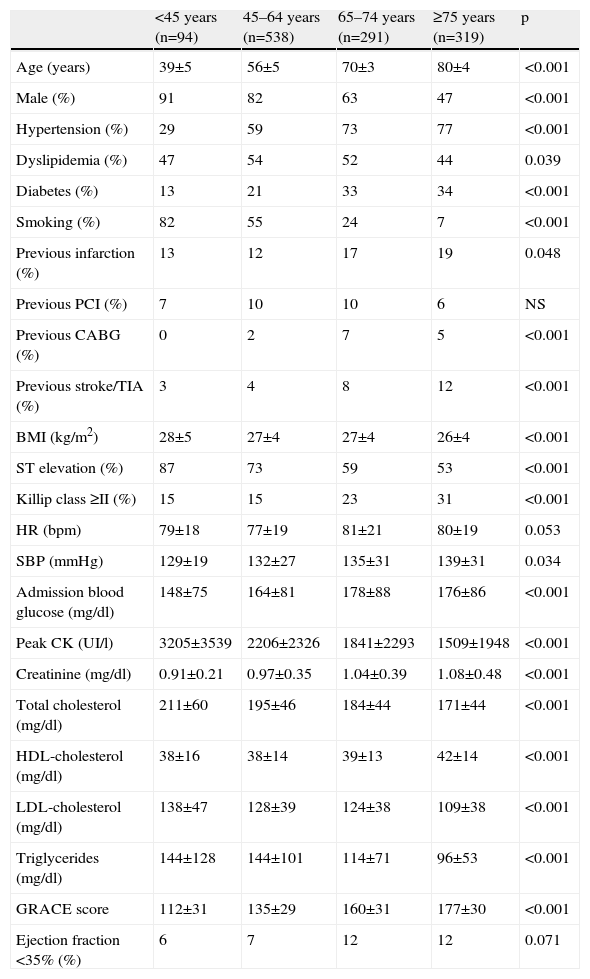
ResultsThe baseline characteristics of the patients by age-group are shown in Table 1. Almost 50% were aged ≥65 and 25.7% were aged ≥75 years; the proportion of women rose with age. Among risk factors for coronary disease, the prevalence of hypertension and diabetes increased with age, while the prevalence of smoking fell. With regard to cardiovascular history, previous cerebrovascular disease, MI and coronary artery bypass grafting (CABG) also increased with age, although no significant differences were found in previous percutaneous coronary intervention.
Clinical characteristics of groups according to age.
| <45 years (n=94) | 45–64 years (n=538) | 65–74 years (n=291) | ≥75 years (n=319) | p | |
| Age (years) | 39±5 | 56±5 | 70±3 | 80±4 | <0.001 |
| Male (%) | 91 | 82 | 63 | 47 | <0.001 |
| Hypertension (%) | 29 | 59 | 73 | 77 | <0.001 |
| Dyslipidemia (%) | 47 | 54 | 52 | 44 | 0.039 |
| Diabetes (%) | 13 | 21 | 33 | 34 | <0.001 |
| Smoking (%) | 82 | 55 | 24 | 7 | <0.001 |
| Previous infarction (%) | 13 | 12 | 17 | 19 | 0.048 |
| Previous PCI (%) | 7 | 10 | 10 | 6 | NS |
| Previous CABG (%) | 0 | 2 | 7 | 5 | <0.001 |
| Previous stroke/TIA (%) | 3 | 4 | 8 | 12 | <0.001 |
| BMI (kg/m2) | 28±5 | 27±4 | 27±4 | 26±4 | <0.001 |
| ST elevation (%) | 87 | 73 | 59 | 53 | <0.001 |
| Killip class ≥II (%) | 15 | 15 | 23 | 31 | <0.001 |
| HR (bpm) | 79±18 | 77±19 | 81±21 | 80±19 | 0.053 |
| SBP (mmHg) | 129±19 | 132±27 | 135±31 | 139±31 | 0.034 |
| Admission blood glucose (mg/dl) | 148±75 | 164±81 | 178±88 | 176±86 | <0.001 |
| Peak CK (UI/l) | 3205±3539 | 2206±2326 | 1841±2293 | 1509±1948 | <0.001 |
| Creatinine (mg/dl) | 0.91±0.21 | 0.97±0.35 | 1.04±0.39 | 1.08±0.48 | <0.001 |
| Total cholesterol (mg/dl) | 211±60 | 195±46 | 184±44 | 171±44 | <0.001 |
| HDL-cholesterol (mg/dl) | 38±16 | 38±14 | 39±13 | 42±14 | <0.001 |
| LDL-cholesterol (mg/dl) | 138±47 | 128±39 | 124±38 | 109±38 | <0.001 |
| Triglycerides (mg/dl) | 144±128 | 144±101 | 114±71 | 96±53 | <0.001 |
| GRACE score | 112±31 | 135±29 | 160±31 | 177±30 | <0.001 |
| Ejection fraction <35% (%) | 6 | 7 | 12 | 12 | 0.071 |
BMI: body mass index; CABG: coronary artery bypass grafting; HR: heart rate; PCI: percutaneous coronary intervention; SBP: systolic blood pressure; TIA: transient ischemic attack.
In terms of presentation, heart rate was comparable in the four age-groups but systolic blood pressure increased with age. Signs of heart failure were more common in the older age-groups, and the GRACE score also rose with age. ST-elevation MI was more frequent among the younger age-groups. Admission blood glucose was higher among the elderly, as was serum creatinine, but lipid profile and peak CK were worse among the younger patients.
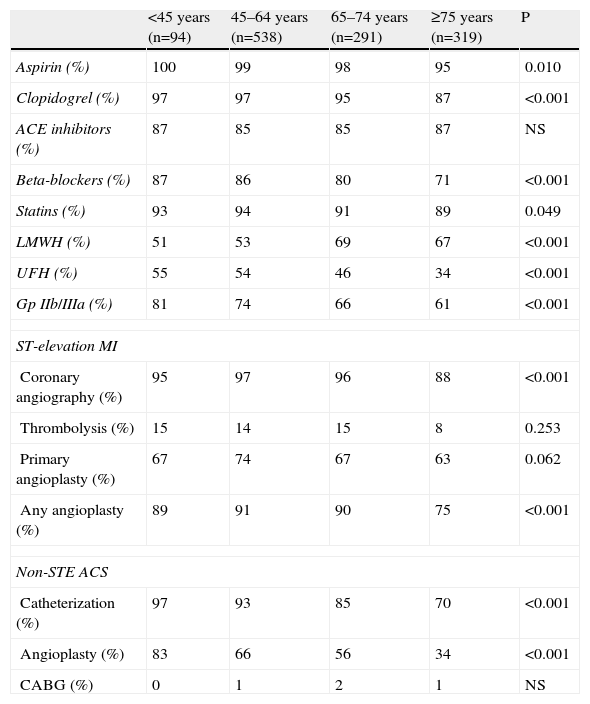
With regard to treatment (Table 2), elderly patients received less drug therapy, with the exception of angiotensin-converting enzyme (ACE) inhibitors. Regarding anticoagulants, low molecular weight heparin was used preferentially in the older age-groups. Use of thrombolysis as the initial reperfusion method was similar between groups. Frequency of percutaneous coronary angioplasty in both ST-elevation MI and non-ST elevation ACS decreased with advancing age. CABG was performed in very few cases, with no differences between groups.
Treatment by age-group.
| <45 years (n=94) | 45–64 years (n=538) | 65–74 years (n=291) | ≥75 years (n=319) | P | |
| Aspirin (%) | 100 | 99 | 98 | 95 | 0.010 |
| Clopidogrel (%) | 97 | 97 | 95 | 87 | <0.001 |
| ACE inhibitors (%) | 87 | 85 | 85 | 87 | NS |
| Beta-blockers (%) | 87 | 86 | 80 | 71 | <0.001 |
| Statins (%) | 93 | 94 | 91 | 89 | 0.049 |
| LMWH (%) | 51 | 53 | 69 | 67 | <0.001 |
| UFH (%) | 55 | 54 | 46 | 34 | <0.001 |
| Gp IIb/IIIa (%) | 81 | 74 | 66 | 61 | <0.001 |
| ST-elevation MI | |||||
| Coronary angiography (%) | 95 | 97 | 96 | 88 | <0.001 |
| Thrombolysis (%) | 15 | 14 | 15 | 8 | 0.253 |
| Primary angioplasty (%) | 67 | 74 | 67 | 63 | 0.062 |
| Any angioplasty (%) | 89 | 91 | 90 | 75 | <0.001 |
| Non-STE ACS | |||||
| Catheterization (%) | 97 | 93 | 85 | 70 | <0.001 |
| Angioplasty (%) | 83 | 66 | 56 | 34 | <0.001 |
| CABG (%) | 0 | 1 | 2 | 1 | NS |
ACE: angiotensin-converting enzyme; CABG: coronary artery bypass grafting; Gp IIb/IIIa: glycoprotein IIb/IIIa receptor antagonists; LMWH: low molecular weight heparin; MI: myocardial infarction; Non-STE ACS: non-ST elevation acute coronary syndrome; UFH: unfractionated heparin.
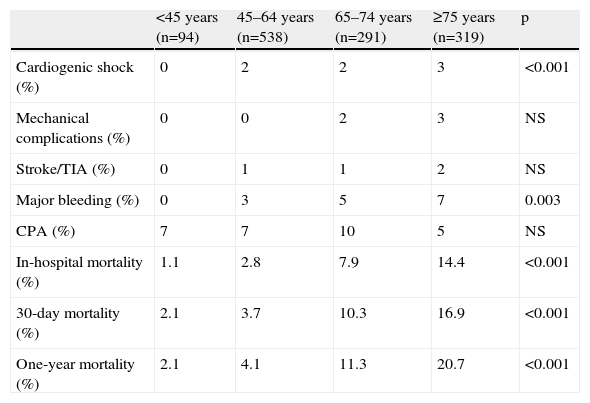
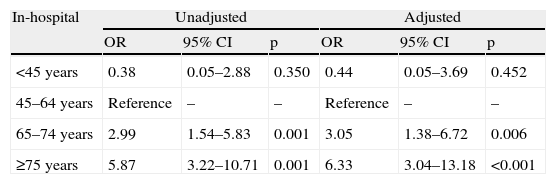
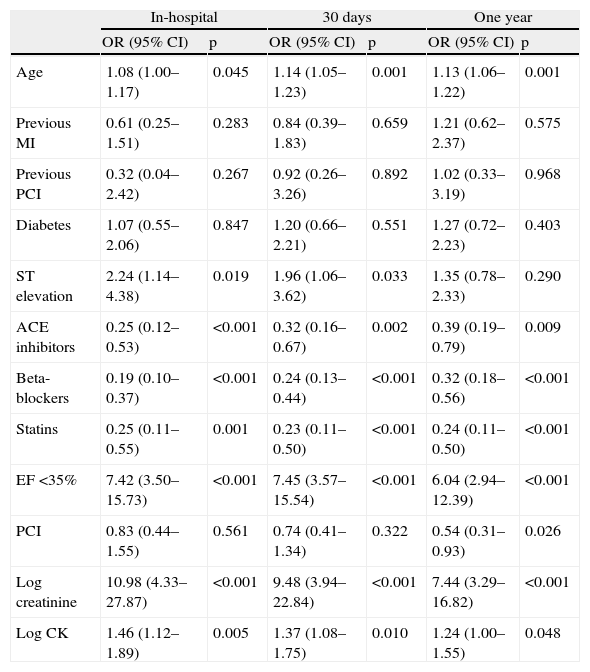
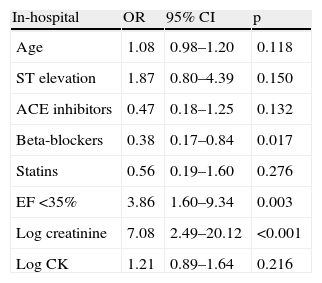
Complications, including cardiopulmonary arrest, mechanical complications and stroke or transient ischemic attack, were not significantly different between groups (Table 3). Cardiogenic shock and major bleeding occurred more frequently in the elderly. In-hospital, 30-day and one-year mortality increased with age, with a particularly high risk in the elderly. Mortality risk adjusted for GRACE risk score (Table 4) remained significantly higher in the elderly. It should be noted that the youngest age-group did not present a better prognosis than the reference age-group (45–64 years). In the oldest age-group, independent predictors of short- and medium-term mortality were poor left ventricular function (ejection fraction <35%) and renal function (Tables 5 and 6). Even in this age-group, age continued to be a predictor of mortality. Use of beta-blockers reduced the risk of in-hospital and 30-day mortality, and was thus a predictor of survival.
Complications and outcomes by age-group.
| <45 years (n=94) | 45–64 years (n=538) | 65–74 years (n=291) | ≥75 years (n=319) | p | |
| Cardiogenic shock (%) | 0 | 2 | 2 | 3 | <0.001 |
| Mechanical complications (%) | 0 | 0 | 2 | 3 | NS |
| Stroke/TIA (%) | 0 | 1 | 1 | 2 | NS |
| Major bleeding (%) | 0 | 3 | 5 | 7 | 0.003 |
| CPA (%) | 7 | 7 | 10 | 5 | NS |
| In-hospital mortality (%) | 1.1 | 2.8 | 7.9 | 14.4 | <0.001 |
| 30-day mortality (%) | 2.1 | 3.7 | 10.3 | 16.9 | <0.001 |
| One-year mortality (%) | 2.1 | 4.1 | 11.3 | 20.7 | <0.001 |
CPA: cardiopulmonary arrest; TIA: transient ischemic attack.
Age-group as a predictor of in-hospital, 30-day and one-year mortality (unadjusted and adjusted for GRACE risk score variables).
| In-hospital | Unadjusted | Adjusted | ||||
| OR | 95% CI | p | OR | 95% CI | p | |
| <45 years | 0.38 | 0.05–2.88 | 0.350 | 0.44 | 0.05–3.69 | 0.452 |
| 45–64 years | Reference | – | – | Reference | – | – |
| 65–74 years | 2.99 | 1.54–5.83 | 0.001 | 3.05 | 1.38–6.72 | 0.006 |
| ≥75 years | 5.87 | 3.22–10.71 | 0.001 | 6.33 | 3.04–13.18 | <0.001 |
| 30 days | Unadjusted | Adjusted | ||||
| OR | 95% CI | p | OR | 95% CI | p | |
| <45 years | 0.56 | 0.13–2.45 | 0.444 | 0.65 | 0.14–2.96 | 0.573 |
| 45–64 years | Reference | – | – | Reference | – | – |
| 65–74 years | 2.98 | 1.66–5.34 | <0.001 | 2.88 | 1.49–5.56 | 0.002 |
| ≥75 years | 5.28 | 3.09–9.00 | <0.001 | 4.91 | 2.65–9.11 | <0.001 |
| One year | Unadjusted | Adjusted | ||||
| OR | 95% CI | p | OR | 95% CI | p | |
| <45 years | 0.51 | 0.12–2.21 | 0.368 | 0.54 | 0.12–2.46 | 0.428 |
| 45–64 years | Reference | – | – | Reference | – | – |
| 65–74 years | 3.00 | 1.71–5.25 | <0.001 | 2.78 | 1.49–5.20 | 0.001 |
| ≥75 years | 6.12 | 3.69–10.14 | <0.001 | 5.72 | 3.20–10.21 | <0.001 |
Predictors of in-hospital, 30-day and one-year mortality in patients aged ≥75 years (univariate analysis).
| In-hospital | 30 days | One year | ||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Age | 1.08 (1.00–1.17) | 0.045 | 1.14 (1.05–1.23) | 0.001 | 1.13 (1.06–1.22) | 0.001 |
| Previous MI | 0.61 (0.25–1.51) | 0.283 | 0.84 (0.39–1.83) | 0.659 | 1.21 (0.62–2.37) | 0.575 |
| Previous PCI | 0.32 (0.04–2.42) | 0.267 | 0.92 (0.26–3.26) | 0.892 | 1.02 (0.33–3.19) | 0.968 |
| Diabetes | 1.07 (0.55–2.06) | 0.847 | 1.20 (0.66–2.21) | 0.551 | 1.27 (0.72–2.23) | 0.403 |
| ST elevation | 2.24 (1.14–4.38) | 0.019 | 1.96 (1.06–3.62) | 0.033 | 1.35 (0.78–2.33) | 0.290 |
| ACE inhibitors | 0.25 (0.12–0.53) | <0.001 | 0.32 (0.16–0.67) | 0.002 | 0.39 (0.19–0.79) | 0.009 |
| Beta-blockers | 0.19 (0.10–0.37) | <0.001 | 0.24 (0.13–0.44) | <0.001 | 0.32 (0.18–0.56) | <0.001 |
| Statins | 0.25 (0.11–0.55) | 0.001 | 0.23 (0.11–0.50) | <0.001 | 0.24 (0.11–0.50) | <0.001 |
| EF <35% | 7.42 (3.50–15.73) | <0.001 | 7.45 (3.57–15.54) | <0.001 | 6.04 (2.94–12.39) | <0.001 |
| PCI | 0.83 (0.44–1.55) | 0.561 | 0.74 (0.41–1.34) | 0.322 | 0.54 (0.31–0.93) | 0.026 |
| Log creatinine | 10.98 (4.33–27.87) | <0.001 | 9.48 (3.94–22.84) | <0.001 | 7.44 (3.29–16.82) | <0.001 |
| Log CK | 1.46 (1.12–1.89) | 0.005 | 1.37 (1.08–1.75) | 0.010 | 1.24 (1.00–1.55) | 0.048 |
ACE: angiotensin-converting enzyme; EF: ejection fraction; MI: myocardial infarction; PCI: percutaneous coronary intervention.
Independent predictors of in-hospital, 30-day and one-year mortality in patients aged ≥75 years (multivariate analysis).
| In-hospital | OR | 95% CI | p |
| Age | 1.08 | 0.98–1.20 | 0.118 |
| ST elevation | 1.87 | 0.80–4.39 | 0.150 |
| ACE inhibitors | 0.47 | 0.18–1.25 | 0.132 |
| Beta-blockers | 0.38 | 0.17–0.84 | 0.017 |
| Statins | 0.56 | 0.19–1.60 | 0.276 |
| EF <35% | 3.86 | 1.60–9.34 | 0.003 |
| Log creatinine | 7.08 | 2.49–20.12 | <0.001 |
| Log CK | 1.21 | 0.89–1.64 | 0.216 |
| 30 days | OR | 95% CI | p |
| Age | 1.16 | 1.06–1.27 | 0.002 |
| ST elevation | 1.67 | 0.76–3.67 | 0.200 |
| ACE inhibitors | 0.59 | 0.23–1.54 | 0.285 |
| Beta-blockers | 0.46 | 0.22–0.97 | 0.042 |
| Statins | 0.43 | 0.16–1.19 | 0.105 |
| EF <35% | 4.46 | 1.87–10.64 | 0.001 |
| Log creatinine | 6.13 | 2.30–16.30 | <0.001 |
| Log CK | 1.18 | 0.89–1.57 | 0.257 |
| One year | OR | 95% CI | p |
| Age | 1.14 | 1.05–1.24 | 0.002 |
| ACE inhibitors | 0.67 | 0.28–1.60 | 0.369 |
| Beta-blockers | 0.56 | 0.29–1.11 | 0.098 |
| Statins | 0.45 | 0.18–1.12 | 0.085 |
| EF <35% | 3.64 | 1.59–8.31 | 0.002 |
| Log creatinine | 4.42 | 1.83–10.68 | 0.001 |
| Log CK | 1.23 | 0.95–1.58 | 0.115 |
| PCI | 0.64 | 0.33–1.24 | 0.184 |
ACE: angiotensin-converting enzyme; EF: left ventricular ejection fraction; PCI: percutaneous coronary intervention.
The increasing number of elderly patients presents challenges for diagnostic and therapeutic approaches in ACS. The definition of “elderly” has changed, now referring to patients aged 75 or over, whereas those in the 65–74 age-group are treated in a similar way to younger patients. The elderly are not only a high-risk group in terms of prognosis but also have an increased risk of treatment-related complications, which significantly affects their management.3 Most of the patients admitted for ACS in the present study, a population that is representative of the real world, were aged between 45 and 75 years, a similar finding to previous registries, including the GRACE registry.3 Gender distribution, prevalence of cardiovascular risk factors and history of heart disease also followed a previously described pattern, with women predominant in the oldest age-group and a higher prevalence of predictors of poor prognosis such as hypertension, diabetes, MI, stroke or transient ischemic attack and previous CABG. This explains the higher risk profile of this age-group and justifies a more aggressive approach. By contrast, this group had a low prevalence of smoking, explained by the fact that smokers rarely reach an advanced age due to associated comorbidities.
With regard to type of ACS, ST-elevation MI was more common in the younger patients, non-ST elevation ACS being more frequent in the elderly, as reported in other registries; this may be related to a higher prevalence of previous MI and revascularization, as well as multivessel disease, at more advanced ages. However, overall, our population had a greater prevalence of ST-elevation MI compared to other registries.3
Despite the demonstrated benefits of beta-blockers, statins and ACE inhibitors,8–10 only the last of these had a similar rate of use in all age-groups, the other drugs being used less, which confirms that the elderly receive less evidence-based therapy, even though the rates observed in our registry are considerably higher than in other multicenter registries, particularly for ACE inhibitors and statins.3 Single or dual antiplatelet therapy is also less often administered in the very elderly, which may be partly explained by the fact that these patients less frequently undergo coronary angioplasty. Unfractionated heparin was more often prescribed in younger patients, while low molecular weight heparin was preferred in the elderly; this may be related to the greater incidence of non-ST elevation MI, less coronary angioplasty and higher bleeding risk in the elderly. This decision may also have been influenced by the fact that low molecular weight heparins are easier to administer since they do not require monitoring and are safer. Use of thrombolysis was similar in all age-groups; while slightly less common in the oldest age-group, this did not reach statistical significance.
Other registries have suggested that the lower use of coronary angioplasty in the very elderly may be related to selection bias since these patients, being seriously ill and with more comorbidities, are more likely to be admitted to centers without cardiac catheterization facilities.11 Nevertheless, our study, in a single center with access to a hemodynamic laboratory at all times, confirmed that the bias is not explained by lack of such access and that the elderly are in fact less often treated by angioplasty. The explanation would thus appear to be the presence of comorbidities, cognitive impairment and functional limitations, among other factors, influencing the indication for revascularization and introducing bias into the results. We would point out, however, that angioplasty was performed in a high percentage (71%) of elderly patients who underwent coronary angiography; it can thus be concluded that once the decision to adopt an invasive strategy in the elderly is made, a significant proportion undergo angioplasty.
Major cardiovascular and bleeding events were more frequent among the elderly, who had a higher initial risk profile and received fewer standard therapies. Mortality remained high even after adjustment for the GRACE risk score, age thus being an independent predictor of short- and medium-term mortality in ACS patients. In-hospital mortality risk was 6.3 times higher in the very elderly compared to the 45–64 age-group, and renal function and left ventricular function were the strongest predictors of short- and medium-term mortality in the elderly.
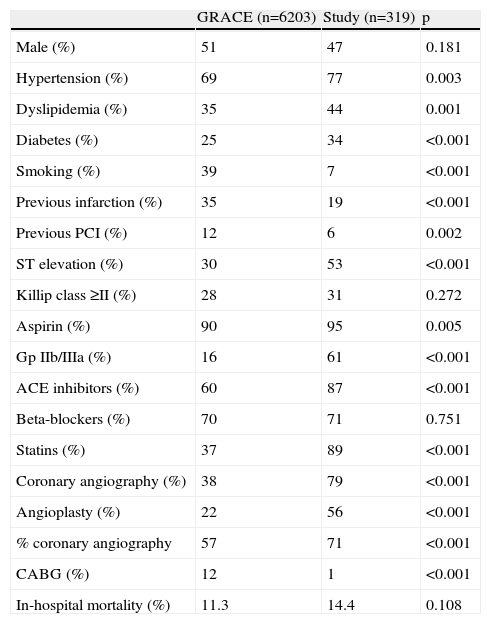
Comparison of our study's oldest age-group (≥75 years) with the GRACE registry population of the same age (Table 7)3 showed a higher frequency of presentation with ST-elevation MI in our population, a greater prevalence of coronary risk factors (except smoking), and a lower prevalence of previous MI or revascularization. With regard to treatment, there was more frequent use in our study population of all drugs with evidence-based benefits except beta-blockers, for which the figures were similar. Coronary angiography and angioplasty were performed considerably more frequently in our population, while CABG was significantly less frequent than in other studies. In our population, CABG was limited to cases with critical coronary anatomy, such as left main disease, whereas other cases with surgical indication were operated electively after the initial hospitalization. In-hospital mortality was slightly higher in our population. These differences from the GRACE registry may be partly explained by the fact that the inclusion period of the GRACE registry ended in 2002, several years before the start of our registry, which means ours reflects improvements in therapeutic management compared to international clinical practice up to 2002. The percentage of patients with ST-elevation MI in our population was also higher, such cases being associated with higher mortality. Furthermore, our study reflects the situation in a tertiary hospital with access to a hemodynamic laboratory, unlike some of the centers participating in the GRACE registry. Finally, the GRACE registry did not include all patients admitted, but only the first 10–20 consecutive patients per month in each center. Our registry included all patients, even those who died shortly after admission, which may explain the slightly higher in-hospital mortality despite improved treatment. We would emphasize that analysis of our population of very elderly patients showed increased use of effective therapies, but this could be further improved by the implementation of evidence-based therapies in clinical practice and the development of simple recommendations and standardized documents, as proposed by the American College of Cardiology.12 Such strategies should treat reperfusion therapy and optimized medical therapy as fundamental in the management of these patients, and should not exclude invasive procedures simply on the basis of the patient's age.
Comparison between elderly population (≥75 years) in the GRACE registry3 and the study population.
| GRACE (n=6203) | Study (n=319) | p | |
| Male (%) | 51 | 47 | 0.181 |
| Hypertension (%) | 69 | 77 | 0.003 |
| Dyslipidemia (%) | 35 | 44 | 0.001 |
| Diabetes (%) | 25 | 34 | <0.001 |
| Smoking (%) | 39 | 7 | <0.001 |
| Previous infarction (%) | 35 | 19 | <0.001 |
| Previous PCI (%) | 12 | 6 | 0.002 |
| ST elevation (%) | 30 | 53 | <0.001 |
| Killip class ≥II (%) | 28 | 31 | 0.272 |
| Aspirin (%) | 90 | 95 | 0.005 |
| Gp IIb/IIIa (%) | 16 | 61 | <0.001 |
| ACE inhibitors (%) | 60 | 87 | <0.001 |
| Beta-blockers (%) | 70 | 71 | 0.751 |
| Statins (%) | 37 | 89 | <0.001 |
| Coronary angiography (%) | 38 | 79 | <0.001 |
| Angioplasty (%) | 22 | 56 | <0.001 |
| % coronary angiography | 57 | 71 | <0.001 |
| CABG (%) | 12 | 1 | <0.001 |
| In-hospital mortality (%) | 11.3 | 14.4 | 0.108 |
ACE: angiotensin-converting enzyme; CABG: coronary artery bypass grafting; Gp IIb/IIIa: glycoprotein IIb/IIIa receptor antagonists; PCI: percutaneous coronary intervention.
The fact that this was a single-center study limits the extent to which its results can be generalized.
No data are available on medication during follow-up or subsequent treatment, which could affect medium-term mortality.
A larger sample would also help to confirm the results obtained.
No analysis of comorbidities was performed, which would have helped give a clearer picture of the clinical status of elderly patients.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Timóteo, A, et al. Impacto da idade no tratamento e resultados após enfarte agudo do miocárdio em particular nos muitos idosos. doi 10.1016/j.repc.2011.09.013.