A coronary fistula is a connection between one of the coronary arteries and a cardiac chamber or great artery. It is a rare defect and usually occurs in isolation. Two-dimensional echocardiography has an important role in diagnosis but coronary or CT angiography is essential to delineate the anatomy. Surgery is the traditional therapeutic approach but percutaneous closure is now the recommended method, with excellent results and few complications in experienced centers.
MethodsWe describe our experience with percutaneous treatment of 15 coronary fistulas in 12 patients between 1996 and 2011. Eight (67%) were males and the median age was 25 years. The most frequent symptoms were murmur and/or fatigue. All fistulas were congenital. Five patients (42%) had concomitant cardiac disease: pulmonary atresia with intact ventricular septum (1), patent ductus arteriosus (1), ostium secundum atrial septal defect (1), stenotic bicuspid aortic valve (1), and critical pulmonary stenosis operated in the neonatal period (1). Three patients had two fistulas, while the others had a single lesion. All fistulas were hemodynamically significant. They originated in the territory of the right coronary (10), left coronary (3) and circumflex (2), draining into the right ventricle (5), pulmonary artery (6), right atrium (2) coronary sinus (1) and left ventricle (1). Embolization materials included standard coils, controlled-release coils, microcoils (standard, GDC or IDC) and an Amplatzer® duct occluder.
ResultsEmbolization was achieved in all patients. There was no mortality. One patient with a large fistula and a very small right coronary artery distally to the origin of the fistula had a right ventricular infarction. In three patients there were minor complications: inadvertent coil embolization, recovered in the same procedure (1), transient arrhythmia (1) and femoral pseudo-aneurysm (1). In a mean follow-up of 4.9 years (1 month to 14 years), there were no procedure-related complications. Echocardiographic and/or angiographic control showed complete and permanent occlusion in ten patients and minimal residual flow in two patients through small collaterals with no hemodynamic significance.
ConclusionPercutaneous embolization represents an effective form of treatment for selected coronary fistulas. A wide range of embolization devices must be available to ensure the best therapeutic approach.
Uma fístula coronária é uma conexão entre uma artéria coronária e uma cavidade cardíaca ou grande vaso. É um defeito raro e que geralmente ocorre de forma isolada. Apesar da ecocardiografia bidimensional ter um papel importante no diagnóstico, a angiotomografia computorizada ou a angiografia coronária, é essencial para a delineação da anatomia. A cirurgia é o tratamento tradicional, mas o encerramento percutâneo é actualmente o método recomendado, com excelentes resultados e baixa morbilidade em grupos com experiência em embolização terapêutica.
População E MétodosDescrevemos a experiência do nosso centro no tratamento percutâneo de 15 fístulas coronárias em 12 doentes entre 1996 e 2011. Oito (67%) eram do sexo masculino. A idade mediana foi 25 anos. Os motivos de referência mais frequentes foram sopro e/ou cansaço. Todas as fistulas eram de origem congénita. Cinco doentes (42%) tinham patologia cardíaca concomitante: atrésia da pulmonar com septo interventricular intacto (1), canal arterial persistente (1), comunicação interauricular ostium secundum (1), estenose aórtica em válvula aórtica biscúspide (1), estenose pulmonar crítica operada no período neonatal (1). Três doentes tinham duas fístulas coronárias e nos restantes a lesão era única. As fístulas eram hemodinamicamente significativas, com origem no território da coronária direita (n=10), da coronária esquerda (n=3) e da circunflexa (n=2) e drenavam para o ventrículo direito (n=5), artéria pulmonar (n=6), aurícula direita (n=2), seio coronário (n=1) e ventrículo esquerdo (n=1). O material de embolização incluiu coils standard, coils de libertação controlada, microcoils (simples, GDC ou IDC) e um dispositivo Amplatzer® Duct Occluder.
ResultadosA embolização da fístula foi obtida em todos os doentes. Não houve mortalidade. Ocorreu enfarte do ventrículo direito num doente com fístula de grandes dimensões e coronária direita de diâmetro muito reduzido distalmente à emergência da fístula. Em três casos ocorreram complicações minor: embolização inadvertida de coil, recuperado no mesmo procedimento (1), arritmia transitória (1) e pseudo-aneurisma femoral (1).
Num seguimento médio de 4,9 anos (um mês a 14 anos) não se registaram intercorrências relacionadas com o procedimento. O controlo por ecocardiograma e/ou angiografia coronária mostrou que em dez doentes houve ocorreu oclusão eficaz e permanente das fístulas, enquanto que dois doentes mantiveram fluxo residual mínimo, por pequenos vasos acessórios, sem repercussão hemodinâmica.
ConclusãoAs embolizações terapêuticas representam uma forma eficaz de abordagem de fístulas coronárias seleccionadas. Estas anomalias têm características muito variáveis, pelo que é necessário dispor de um grande leque de dispositivos para seleccionar a opção mais eficaz.
A coronary fistula is a connection between one of the coronary arteries and a cardiac chamber or great artery.1–4 It is a rare defect and usually occurs in isolation, but is the most common hemodynamically significant congenital coronary anomaly.5 Its precise incidence is unknown, but is estimated at 0.3–0.8% on the evidence of diagnostic cardiac catheterization.1,6 Most coronary fistulas are congenital in origin, but they may occur after cardiac surgery or trauma.4,10 They are usually asymptomatic in the first decades of life, particularly if small,4 but then symptoms and complications increase in frequency. Complications include coronary steal from adjacent myocardium, thrombosis, embolism, heart failure, atrial fibrillation, endocarditis or endarteritis, rupture and arrhythmias.1,2 The main differential diagnosis is with patent ductus arteriosus and arteriovenous fistulas.7
Two-dimensional and color Doppler echocardiography has an important role in the diagnosis of coronary fistulas, but coronary or computed tomography (CT) angiography is essential to delineate the anatomy. Surgery is the traditional therapeutic approach but percutaneous closure is an alternative with good results and few complications in experienced centers.4 Fistulas should always be closed if there is significant hemodynamic compromise.4,8
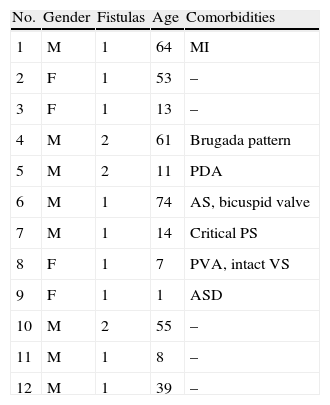
MethodsWe describe our experience with percutaneous treatment of 15 coronary fistulas in 12 patients between 1996 and 2011. Eight (67%) were males and the median age was 25 years (Table 1).
Demographic characteristics of the study population.
| No. | Gender | Fistulas | Age | Comorbidities |
| 1 | M | 1 | 64 | MI |
| 2 | F | 1 | 53 | – |
| 3 | F | 1 | 13 | – |
| 4 | M | 2 | 61 | Brugada pattern |
| 5 | M | 2 | 11 | PDA |
| 6 | M | 1 | 74 | AS, bicuspid valve |
| 7 | M | 1 | 14 | Critical PS |
| 8 | F | 1 | 7 | PVA, intact VS |
| 9 | F | 1 | 1 | ASD |
| 10 | M | 2 | 55 | – |
| 11 | M | 1 | 8 | – |
| 12 | M | 1 | 39 | – |
AS: aortic stenosis; ASD: atrial septal defect; MI: myocardial infarction; PDA: patent ductus arteriosus; PS: pulmonary stenosis; PVA: pulmonary valve atresia; VS: ventricular septum.
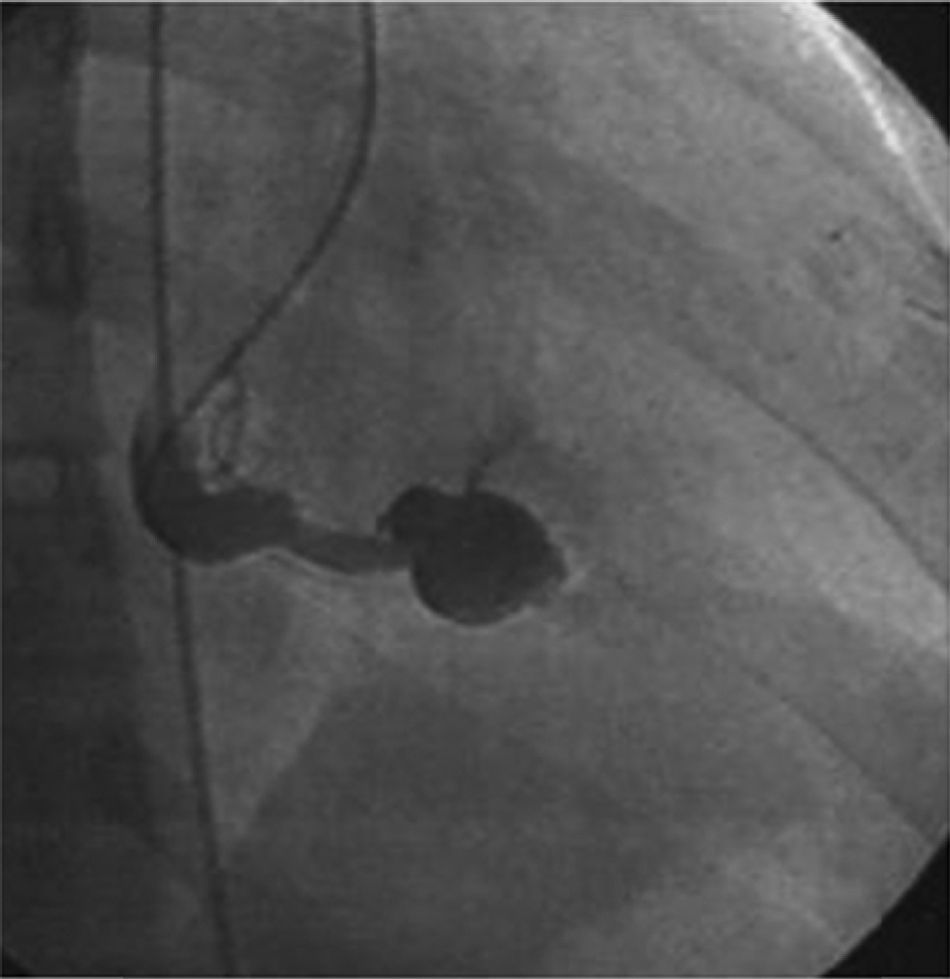
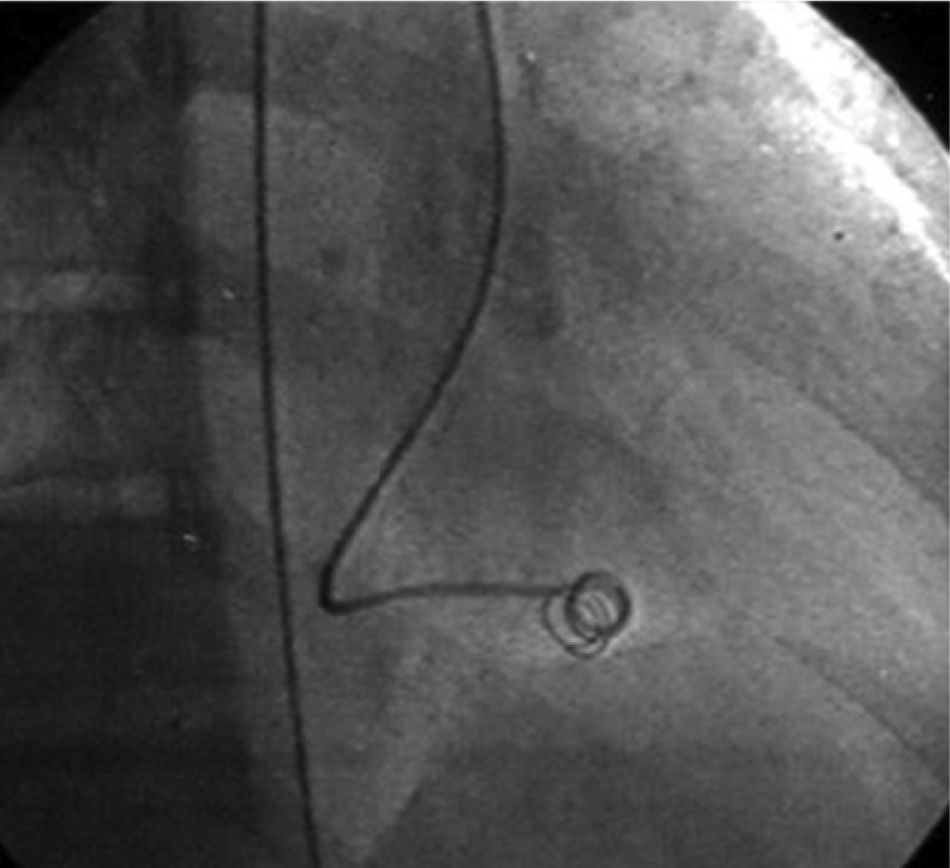
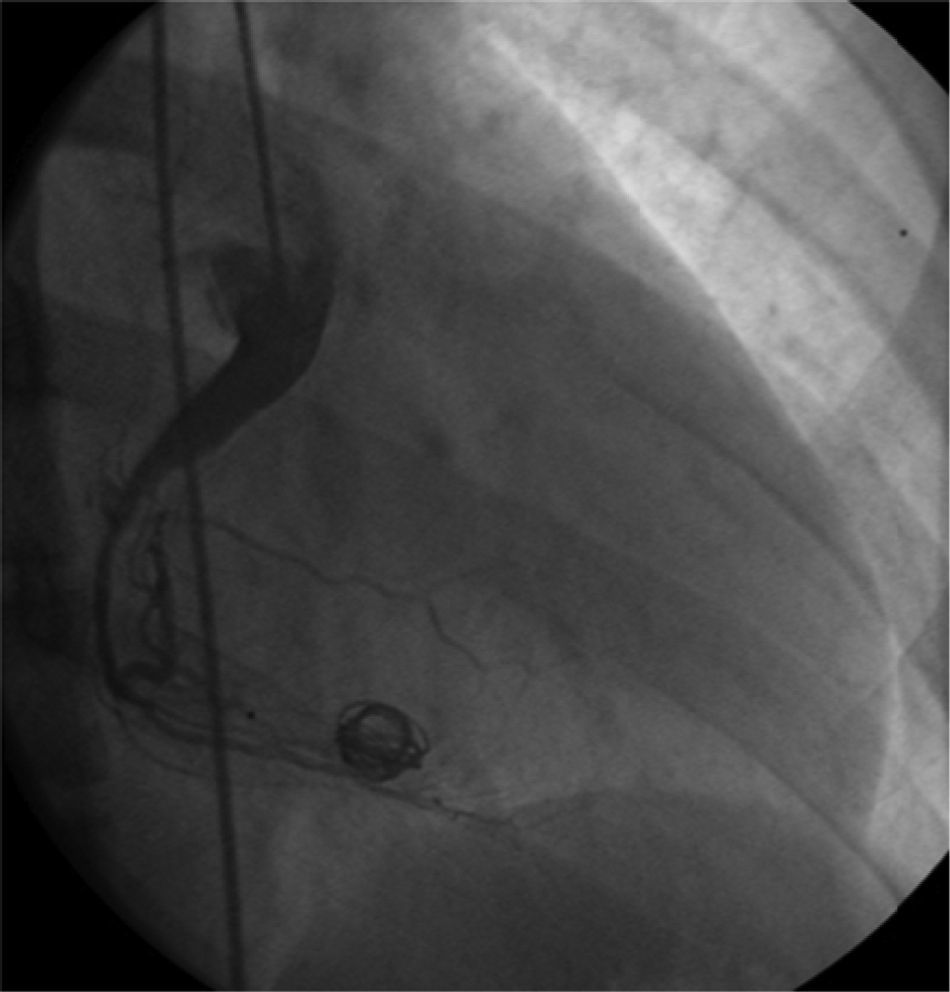
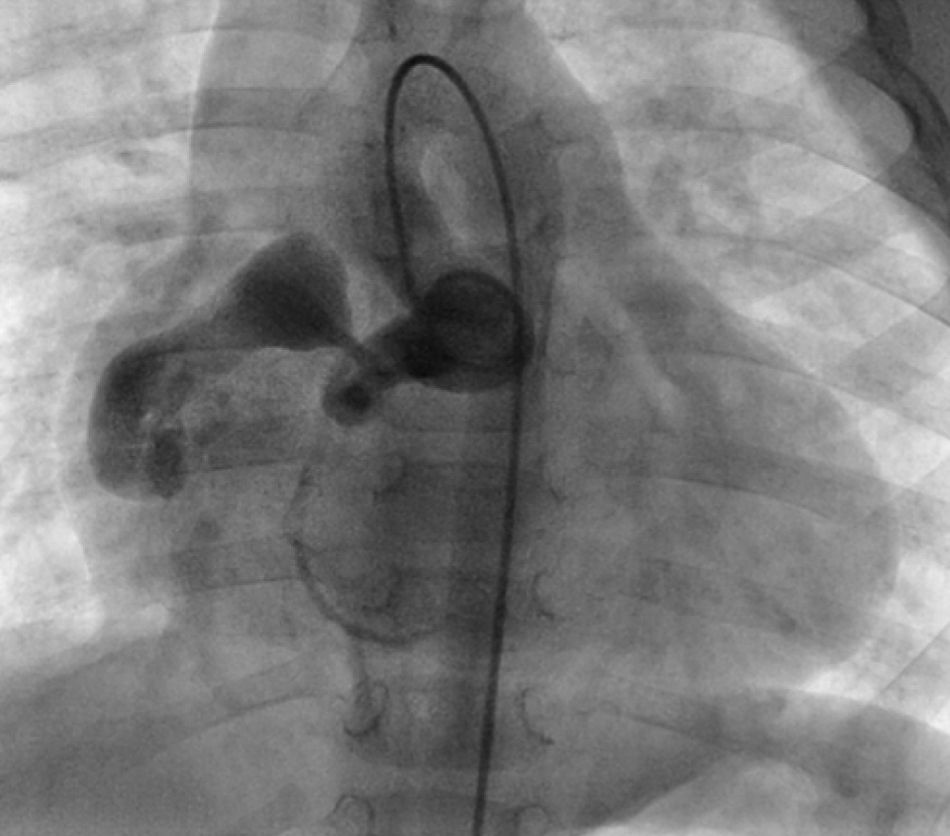
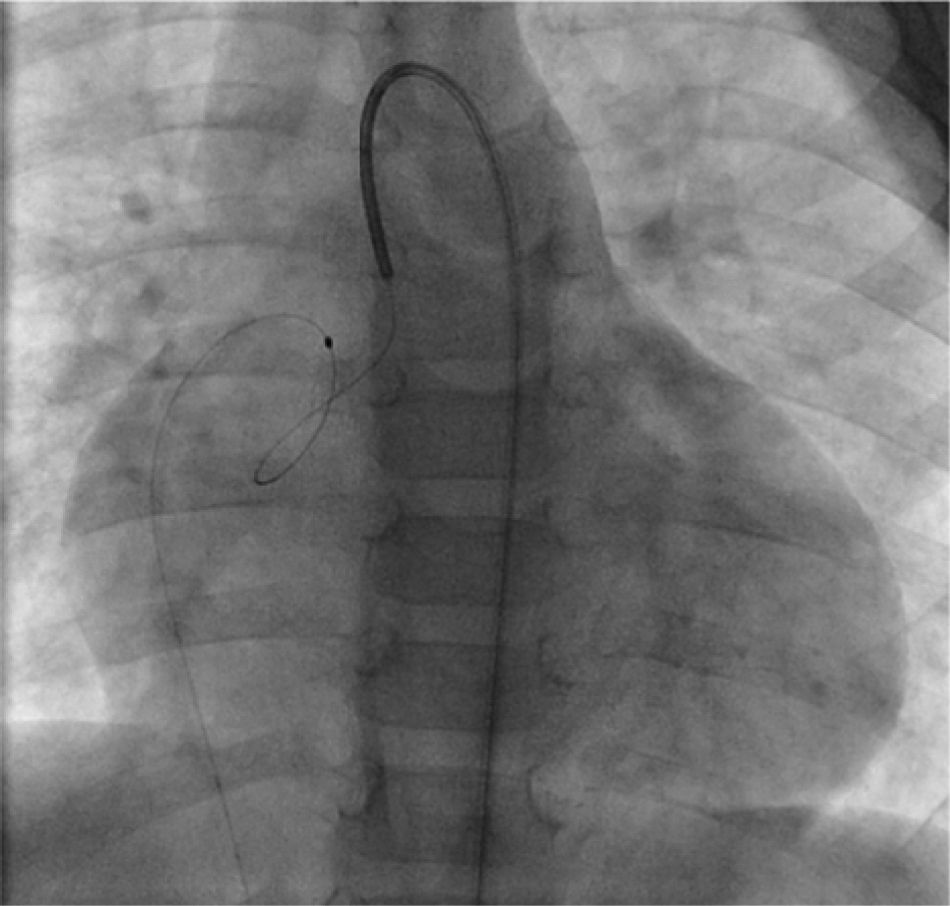
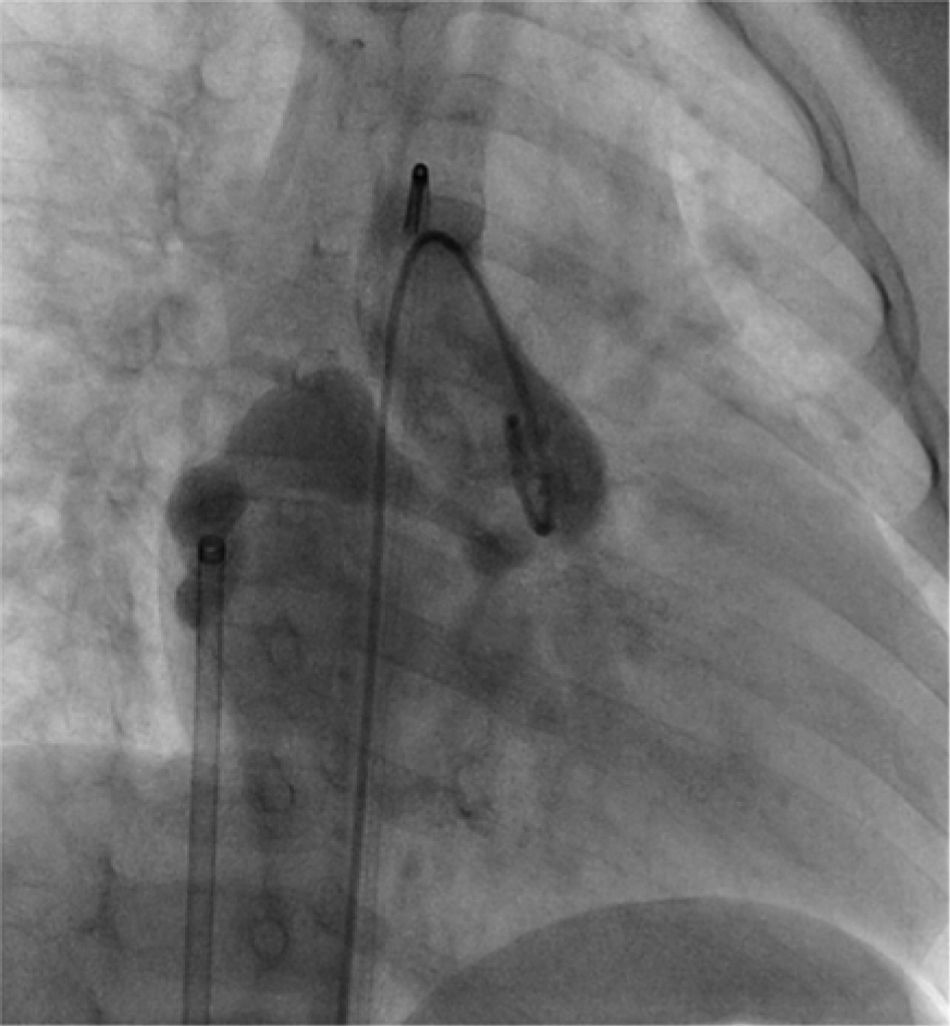
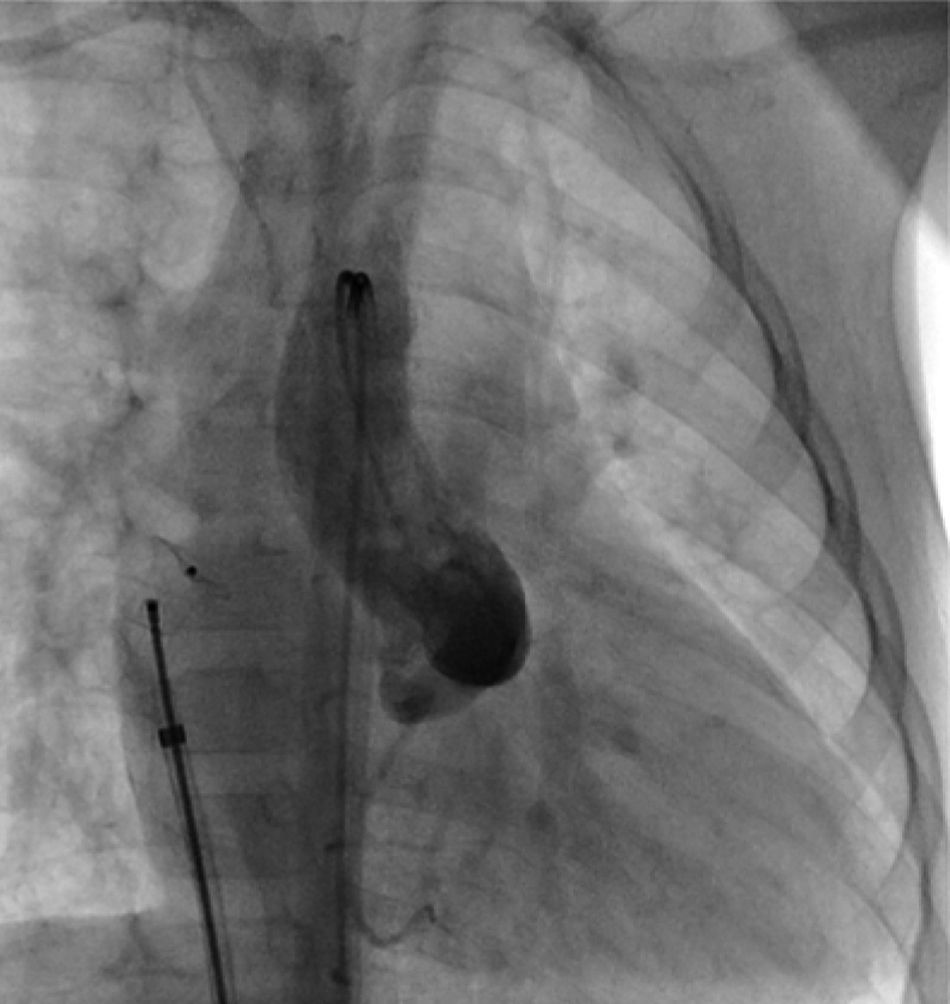
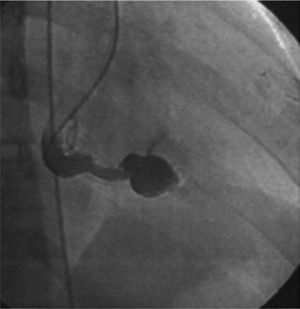
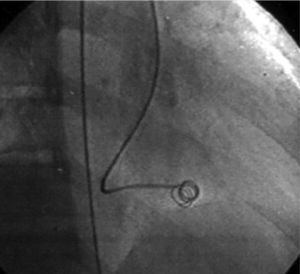
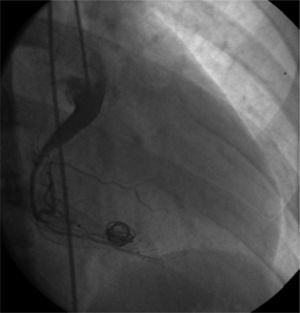
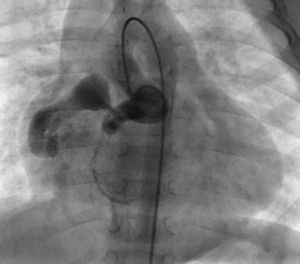
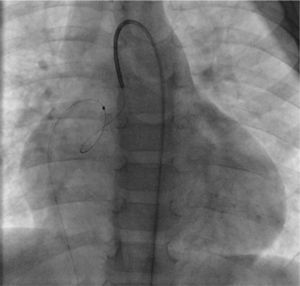
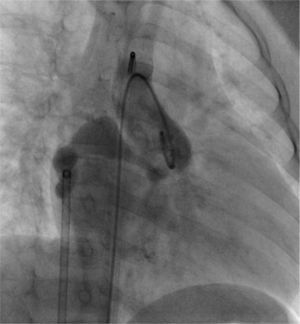
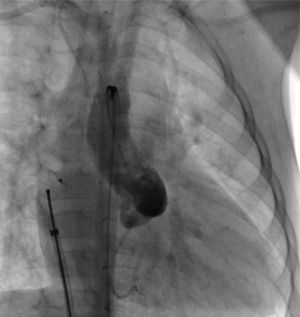
The most frequent symptoms were murmur and/or fatigue. All fistulas were congenital. Five patients (42%) had concomitant cardiac disease: pulmonary atresia with intact ventricular septum (1), patent ductus arteriosus (1), ostium secundum atrial septal defect (1), stenotic bicuspid aortic valve (1), and critical pulmonary stenosis operated in the neonatal period (1). Selective angiography was performed to delineate the anatomy of the fistula(s), which were embolized in the most distal part, sparing all the collateral branches. In one patient an arteriovenous loop was formed through the fistula, embolizing the terminal part of the fistula from the right atrium. The patients were heparinized (100UI/kg in children and 5000UI in adults) and were subsequently monitored by assessing activated coagulation time. Three patients had two fistulas, while the others had a single lesion. All fistulas were hemodynamically significant. They originated in the territory of the right coronary (10), left coronary (3) and circumflex (2), draining into the right ventricle (5), pulmonary artery (6), right atrium (2) coronary sinus (1) and left ventricle (1). Embolization materials included 15 standard coils in three patients, a Jackson® coil in one patient (Figures 1–3), 27 microcoils in 11 patients (18 standard microcoils in seven patients and nine GDC microcoils in four patients), and an Amplatzer® duct occluder in one patient (Figures 4–7). The GDC microcoils, both standard and complex, deserve particular mention, as release of these devices is controlled by electrolysis. The procedure is thus reversible up to the last stage of release, following confirmation of correct positioning. An Amplatzer® cardiac plug was tested in one patient but was not released due to its unsuitability for the lesion.
Embolization was achieved in all patients. There was no mortality. One patient with a large fistula and a very small right coronary artery distally to the origin of the fistula had a right ventricular infarction. In three patients there were minor complications: inadvertent coil embolization, recovered in the same procedure (1), transient arrhythmia (1) and femoral pseudo-aneurysm (1).
In a mean follow-up of 4.9 years (1 month to 14 years), there were no procedure-related complications. Echocardiographic and/or angiographic control showed complete and permanent occlusion in ten patients and minimal residual flow in two patients through small collaterals, with no hemodynamic significance.
DiscussionPercutaneous closure of coronary fistulas is among the most complex of percutaneous interventions, with the risk of embolization of normal coronary branches, migration of closure devices to the cardiac chambers or great arteries, or rupture of the fistula itself. Thorough assessment of the morphology and course of the fistula is essential in order to decide the best site for embolization and to select the most suitable device. Advances in CT angiography of the coronary arteries enable the course and communications of coronary fistulas to be accurately delineated, making it extremely useful in diagnosis and planning the optimum strategy for closure.9,10
The traditional therapeutic approach is surgical closure. In a 1997 review by Mavroudis et al. of surgical closure of coronary fistulas in 17 children aged between 6 weeks and 16.5 years (mean 5.5 years) between 1968 and 1996, surgical closure was 100% effective and there were no deaths; the authors concluded that surgery was the treatment of choice, with percutaneous closure being reserved for a small number of selected patients.11 However, as early as 1991 percutaneous closure of seven coronary fistulas had been described in patients aged between 2 and 67 years (mean 17 years), with successful closure in six out of seven fistulas and no complications in a follow-up of 4 months to 4 years.12 These authors highlighted the advantages of percutaneous closure, including the ability to detect additional fistulas that only become apparent after the percutaneous closure of larger lesions. Although the procedure is technically more demanding, large fistulas draining into the right atrium or right ventricle can be closed by a venous approach using Amplatzer® duct occluders or plugs, correct device positioning being monitored by selective retrograde contrast injection into the coronary artery, as described by Pedra et al. in 2000.5
Armsby et al.7 described the transcatheter closure of 35 fistulas in patients aged between 8 months and 68 years (mean 8 years), with a mean follow-up of 2.8 years. Closure was achieved in only 33 cases (85%) and was effective in 27 (82%); there were no deaths. These results are similar to those for surgical closure in terms of efficacy, morbidity and mortality. Alekyan et al.,13 also in 2002, described the transcatheter closure of 15 coronary fistulas in patients aged between 11 months and 44 years (mean 7 years) and a follow-up of between 6 months and 13 years; closure was effective in 13 cases, but there was one death, of a four-year-old due to renal failure following femoral artery thrombosis. In 2007, Collins et al. reported the percutaneous closure of 14 fistulas in adults with a mean follow-up of 2.6 years; the procedure was successful in 11 patients and there were no deaths.14 The authors concluded that the technique was safe and effective in treating symptomatic fistulas in adults.
Particular mention should be made of the most serious complication in our series, a right ventricular infarction. In this patient, the very dilated (around 1cm in diameter) proximal right coronary artery continued into a large fistula, but distally to the origin of the fistula the artery was very small. After embolization, flow in the proximal right coronary became extremely slow. Slow flow in an enlarged vessel can be at high risk of proximal progression of thrombi from the embolized fistula, and so effective anticoagulation is essential in such patients.
Two cases of coronary fistulas successfully closed by an antegrade approach using the Amplatzer® vascular plug were recently described in children aged 1 and 4 years, with a follow-up of 12 and 18 months respectively, with no deaths.15 Finally, in 2010 Bruckheimer et al.16 reported a series of 10 patients aged between 0.5 and 52.2 years (mean 2.6 years) and a mean follow-up of 1.7 years. All the fistulas were large and were closed using Amplatzer® duct occluders and vascular plugs, successfully in nine of the ten cases, with no mortality or significant complications. However, there have as yet been no multicenter studies of this therapeutic approach.
In conclusion, despite the complexity of this technique and the rarity of the condition, therapeutic embolization represents an effective form of treatment for selected coronary fistulas in specialized centers.
Ours is the first series described in Portugal on percutaneous closure of coronary fistulas, all hemodynamically significant and some very large, one closed with an Amplatzer® duct occluder, and seven performed in children (between 1 and 14 years of age). There were no deaths or significant complications except for infarction in one patient with a large fistula and a very small coronary artery distally to the fistula. Overall, percutaneous closure of coronary fistulas was shown to be a safe and effective procedure in selected patients, even at pediatric ages.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Silva M, et al. Embolização percutânea de fístulas coronárias – experiência de um centro. doi 10.1016/j.repc.2011.10.005.