Hypersensitivity reactions to nonsteroidal anti-inflammatory drugs are common and five types of reactions have been defined. The prevalence of such reactions in patients with myocardial infarction is unclear, and so antiplatelet therapy in this population is a challenge. Various desensitization protocols have been developed but there are no specific guidelines for their use. The authors present the case of a patient with acute coronary syndrome and aspirin hypersensitivity referred for urgent coronary angiography.
Aspirin desensitization therapy is safe and successful in many patients, but more randomized trials are needed to confirm its benefits in coronary artery disease patients.
As reações de hipersensibilidade aos anti-inflamatórios não-esteroides são comuns na população em geral, estando definidos cinco tipos de reações. A prevalência desta reação adversa em doentes com enfarte agudo do miocárdio é incerta, constituindo a antiagregação plaquetária um desafio terapêutico nestes doentes. Atualmente existem vários protocolos de dessensibilização, contudo não existem orientações específicas para a sua utilização. Os autores apresentam o caso de um doente com síndrome coronária aguda e hipersensibilidade à aspirina, com necessidade de coronariografia urgente. A dessensibilização à aspirina é eficaz e segura na maioria dos doentes, contudo são necessários mais estudos aleatorizados em doentes com doença coronária para evidenciar os seus benefícios.
acute coronary syndrome
bare-metal stent
coronary artery disease
cyclooxygenase
circumflex artery
electrocardiogram
heart rate
myocardial infarction
nonsteroidal anti-inflammatory drugs
percutaneous coronary intervention
right coronary artery
Hypersensitivity reactions to nonsteroidal anti-inflammatory drugs (NSAIDs) are common in the general population, accounting for 21-25% of adverse drug reactions, of which 0.5-1.9% are due to aspirin.1
In the past, these reactions were related to aspirin, which for decades was the only NSAID available on the market, but most are now observed with other drugs in this class, and so hypersensitivity to NSAIDs is now the preferred term.1
Hypersensitive reactions to NSAIDs are classified based on clinical manifestation, the presence of an underlying disease, and cross-reactivity with other cyclooxygenase (COX)-1 inhibitors.1
The Position Paper on NSAIDs Hypersensitivity published by the European Academy of Allergy and Clinical Immunology Task Force in 2013 defines five types of reaction1:
- 1.
NSAIDs-exacerbated respiratory disease
- 2.
NSAIDs-exacerbated cutaneous disease
- 3.
NSAIDs-induced urticaria/angioedema
- 4.
Urticaria/angioedema or anaphylaxis induced by a single NSAID or by several NSAIDs belonging to the same chemical group
- 5.
Delayed reactions to a single NSAID or to several NSAIDS belonging to the same chemical group.
The first three types are associated with COX-1 inhibition and subsequent activation of mast cells and eosinophils, and are found with various NSAID chemical classes. The putative immunological mechanism of type 4 is immunoglobulin E-mediated, while type 5 is mediated by hypersensitivity at the cellular level.1
Dual antiplatelet therapy with aspirin and ticagrelor, prasugrel or clopidogrel is a class I recommendation, level of evidence A, in treating acute coronary syndrome (ACS).6
The prevalence of aspirin hypersensitivity in patients with myocardial infarction (MI) is unclear but has been estimated at 1.5%, and so antiplatelet therapy in these patients is a challenge.2
One treatment option is desensitization, in which progressively higher oral doses of aspirin are administered until the therapeutic dose is reached in order to increase tolerance.2–4
Patients with type 1 or 3 hypersensitivity reactions can undergo a desensitization protocol, which has been shown to be safe and effective. The procedure is controversial for type 2 reactions and there are no data for type 4 reactions.1
There are currently various desensitization protocols, but guidelines on their use are not supported by randomized trials (level of evidence B or C), and there have been few studies on patients with ACS.2–5 The protocol of Wong et al. (Table 1) is the most widely used in the context of unstable coronary artery disease (CAD), since it enables rapid desensitization.4
The following reactions can occur during the desensitization protocol: bronchospasm, ≥20% reduction in forced expiratory volume in 1 s, and naso-ocular (lachrymation, peri-orbital edema, rhinorrhea and nasal congestion) and cutaneous symptoms. In the presence of a reaction, directed therapy should be begun and the protocol should be maintained or discontinued depending on response and clinical severity.4
Patients must continue to take aspirin on a daily basis after successful desensitization in order to prevent resensitization given that the refractory period lasts from 2 to 5 days.1,2,4
According to the few studies in the literature, in emergent or urgent situations (ST-elevation ACS or non-ST-elevation ACS with high risk criteria [refractory angina, heart failure or cardiogenic shock, ventricular arrhythmias, and symptomatic or silent dynamic ST-segment or T-wave alterations]) in which desensitization is not possible before percutaneous coronary intervention (PCI), the suggested therapeutic options include direct thrombin and glycoprotein IIb/IIIa inhibitors during the procedure, even with the use of stents (Figure 1).4
Decision algorithm for patients with coronary artery disease and NSAID sensitivity. CAD: coronary artery disease. Adapted from Gollapudi et al.4
In order to minimize the duration of dual antiplatelet therapy, balloon angioplasty or bare-metal stents (BMS) are the best treatment options for PCI.4
The WARIS II trial found that warfarin was superior to aspirin in preventing the combined endpoint of death, nonfatal reinfarction and stroke, although it was associated with more bleeding complications; warfarin is thus an option in the acute phase and for long-term therapy.3
Case reportAS, a 78-year-old man, an ex-smoker, had a history of hypertension, dyslipidemia, hyperuricemia, benign prostatic hypertrophy, peptic disease, nasal polyposis and asthma, under bronchodilator therapy. He also had a documented history of hypersensitivity reactions to NSAIDs, notably aspirin, following a positive provocation test with naso-ocular symptoms and wheezing at a cumulative aspirin dose of 460 mg.
He had been asymptomatic until one week before admission, when he began suffering episodes of angina (Canadian Cardiovascular Society class II) and consulted his family doctor. He was referred for exercise testing, which was positive for ischemia, with severe clinical (angina) and electrocardiographic criteria (2.2 mm ST elevation in the inferior leads) after six minutes. The patient experienced symptom relief after the test was terminated and sublingual nitroglycerin was administered, with normalization of the electrocardiogram (ECG) after five minutes. In the light of the exercise test result, he was immediately transferred to the emergency department.
At admission he was asymptomatic, with no relevant findings on physical examination. Laboratory tests revealed positive biomarkers of myocardial necrosis (troponin I 1.65 μg/l [cut-off 0.04 μg/dl]) and the ECG showed sinus rhythm with a heart rate (HR) of 70 bpm, with no Q waves or ST-segment alterations.
A diagnosis of non-ST elevation MI was made with indication for coronary angiography during hospitalization, after aspirin desensitization. The patient presented a GRACE score of 125 (intermediate risk) at admission.
Anti-ischemia and antiplatelet therapy with ticagrelor was begun, as well as anticoagulation with fondaparinux.
On the following day, he suffered a recurrence of angina at rest, which was not relieved by sublingual nitroglycerin, only by intravenous isosorbide dinitrate. The ECG showed HR of 60 bpm, sinus rhythm, new-onset Q waves and deep negative T waves in the inferior leads (Figure 2), while transthoracic echocardiography revealed inferior wall akinesia and preserved biventricular function, with no significant valve changes, and laboratory tests showed elevated biomarkers of myocardial necrosis (peak troponin I 5 μg/l).
In the light of the patient's worsening clinical condition and of the changes on diagnostic exams, urgent invasive treatment was considered necessary, and an aspirin desensitization protocol was immediately begun. This consisted of oral administration of increasing doses at intervals of 15 min of 100 mg of aspirin in 100 ml of 0.9% saline solution, resulting in a cumulative dose of 323.4 mg aspirin, in accordance with Table 1,3 preceded by pre-treatment with an antihistamine (hydroxyzine 25 mg).
The patient remained in the coronary care unit in the cardiology department during the protocol, under constant electrocardiographic and blood pressuring monitoring by medical and nursing staff.
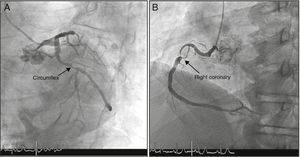
Desensitization was performed without complications and the patient underwent coronary angiography two hours later. This revealed a 90% lesion in the proximal segment of the circumflex artery (Cx) and an extensive lesion in the proximal segment of the right coronary artery (RCA), causing severe subocclusive stenosis, with TIMI 3 flow. Angioplasty of the proximal RCA was performed with placement of two BMS and of the proximal Cx with one BMS (Figure 3).
Anticoagulation was discontinued after the procedure and dual antiplatelet therapy with aspirin and ticagrelor was begun. Hospital stay was uneventful, with no angina or symptoms of aspirin resensitization.
The patient was discharged on the fifth day, under dual antiplatelet therapy (aspirin 100 mg and ticagrelor 90 mg, twice daily) and referred to the angioplasty clinic and the immunology and allergy clinic.
The patient remains under dual antiplatelet therapy with aspirin and ticagrelor after six months of follow-up, and has shown no signs of resensitization to date.
DiscussionIn the case presented, the patient's worsening clinical condition meant that urgent coronary angiography was indicated, as well as dual antiplatelet therapy. His history of nasal polyposis, rhinitis and aspirin-associated bronchospasm suggested NSAIDs-exacerbated respiratory disease, a situation in which desensitization can be performed.
Although there were therapeutic alternatives, notably warfarin, in view of the need for urgent invasive intervention and the positive experience reported by others using desensitization in this context, it was decided to opt for aspirin desensitization.
There are various desensitization protocols available but some take more than 24 hours and are therefore not suitable in cases of unstable CAD.
The protocol of Wong et al. was chosen for its speed, enabling coronary angiography to be performed after approximately two hours. According to the literature, this protocol has a low incidence of adverse events and a high rate of success, although most studies have been in patients with aspirin-induced urticaria and angioedema.4
BMS were used in the case presented in order to minimize the risk associated with early discontinuation of dual antiplatelet therapy in view of possible failure of desensitization or the patient discontinuing aspirin therapy during follow-up.
Aspirin desensitization was shown to be safe and effective in our patient, with no complications, as demonstrated by other groups.
The maintenance aspirin dose required to prevent resensitization is unknown, but on the basis of recent studies, a cardioprotective dose of 100 mg in patients taking ticagrelor is sufficient to keep these patients desensitized.2,4
Desensitization in patients with ST-elevation ACS is not indicated since this would delay coronary reperfusion. There have been few studies on such cases, but a loading dose of a thienopyridine and unfractionated heparin have been proposed. The preferred approach is balloon angioplasty or BMS implantation, together with direct thrombin and glycoprotein IIb/IIIa inhibitors, but this is not consensual. We found no mention in our literature review of a periprocedural pharmacological protocol that included antihistamine or corticosteroid therapy. After an invasive procedure, a desensitization protocol should be considered once the patient has stabilized. In most published studies, desensitization was performed within 24 h of PCI.4,7,8
ConclusionHypersensitivity to NSAIDs is relatively common and constitutes a therapeutic challenge in patients with CAD.
Aspirin desensitization appears to b-e effective and safe in most CAD patients, as in the case presented. However, more randomized trials are needed to clarify the risks and benefits. At present, its use should be considered on a case-by-case basis.
Desensitization protocols should be established that are appropriate for different situations based on analysis of data from clinical experience, with a view to facilitating decision-making and application.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Duarte T, Gonçalves S, Sá C, et al. Hipersensibilidade à aspirina e coronariografia urgente: desafio terapêutico. Rev Port Cardiol. 2016;35:619.e1–619.e5.








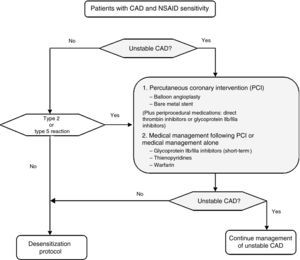 CAD: coronary artery disease. Adapted from Gollapudi et al.4'/>
CAD: coronary artery disease. Adapted from Gollapudi et al.4'/>