We present the case of a 46-year-old woman with episodes of chest pain with ST-T segment elevation and paroxysmal high-degree atrioventricular block and syncopal episodes. Coronary angiography revealed no significant atheromatous lesions. The patient was treated with nitrates and calcium channel blockers but syncopal episodes with atrioventricular block persisted. A DDD-R pacemaker was implanted and 4-month follow-up was uneventful.
Apresentamos o caso de uma mulher de 46 anos com episódios frequentes de dor precordial e síncope associados a elevação do segmento ST e períodos de bloqueio aurículo-ventricular de alto grau transitórios. A coronariogafia excluiu lesões significativas e a doente foi tratada com nitratos e antagonistas do cálcio. Verificou-se persistência da sintomatologia associada a períodos de bloqueio aurículo-ventricular sintomáticos, refractários a otimização terapêutica.Implantação de pacemaker DDD-R. Follow-up de 4 meses sem intercorrências.
A 46-year-old woman, premenopausal, was referred for a cardiology consultation due to recurrent typical chest pain unrelated to exertion, with occasional syncope during these episodes. Her cardiovascular risk factors were dyslipidemia and smoking (48 pack-years).
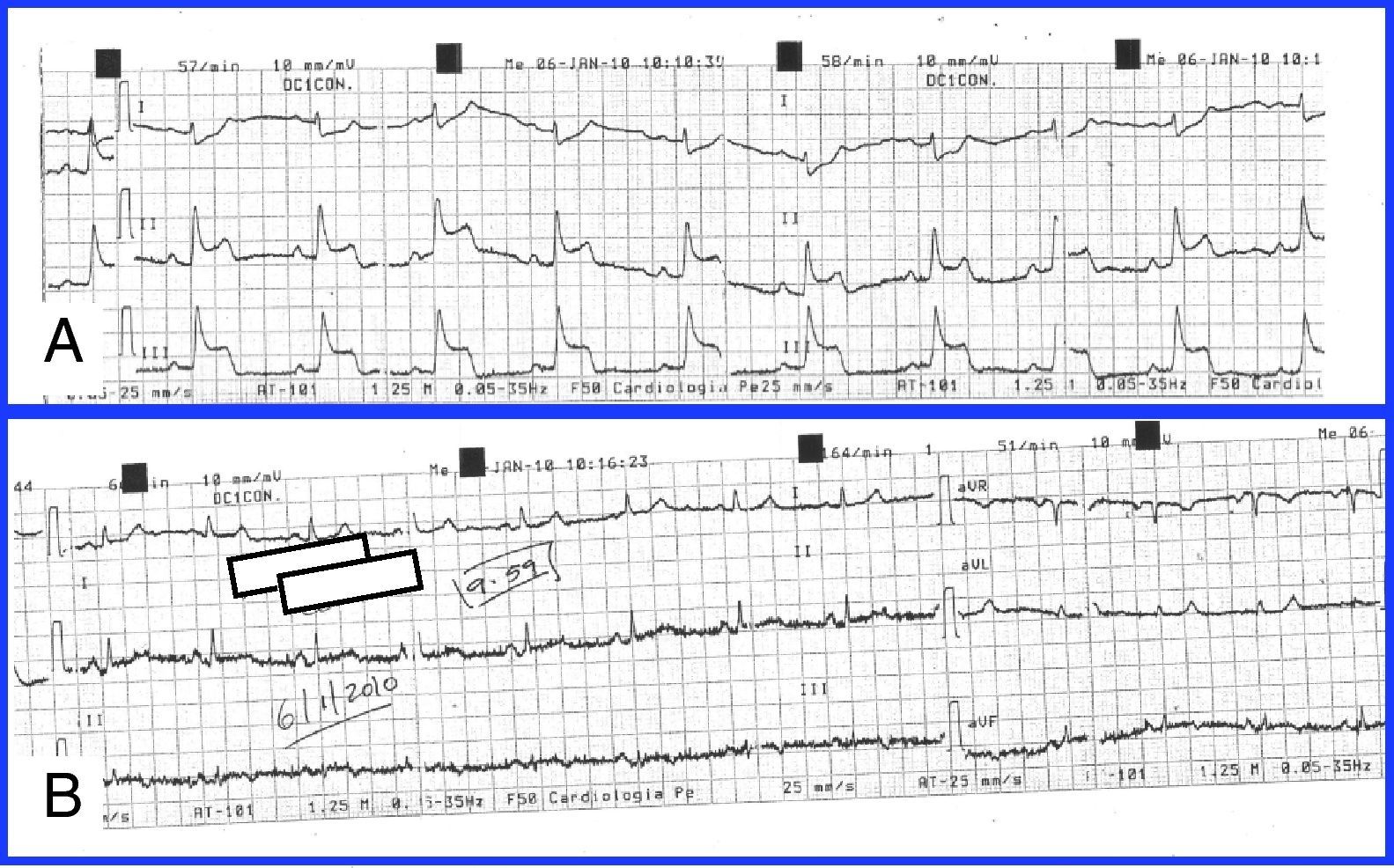
During the consultation she experienced a similar episode of chest pain. The electrocardiogram (ECG) showed sinus rhythm with ST-segment elevation in the inferior leads (Fig. 1A). Clinical and electrocardiographical normalization was seen 6min after administration of 5mg of sublingual nitroglycerine (Fig. 1B).
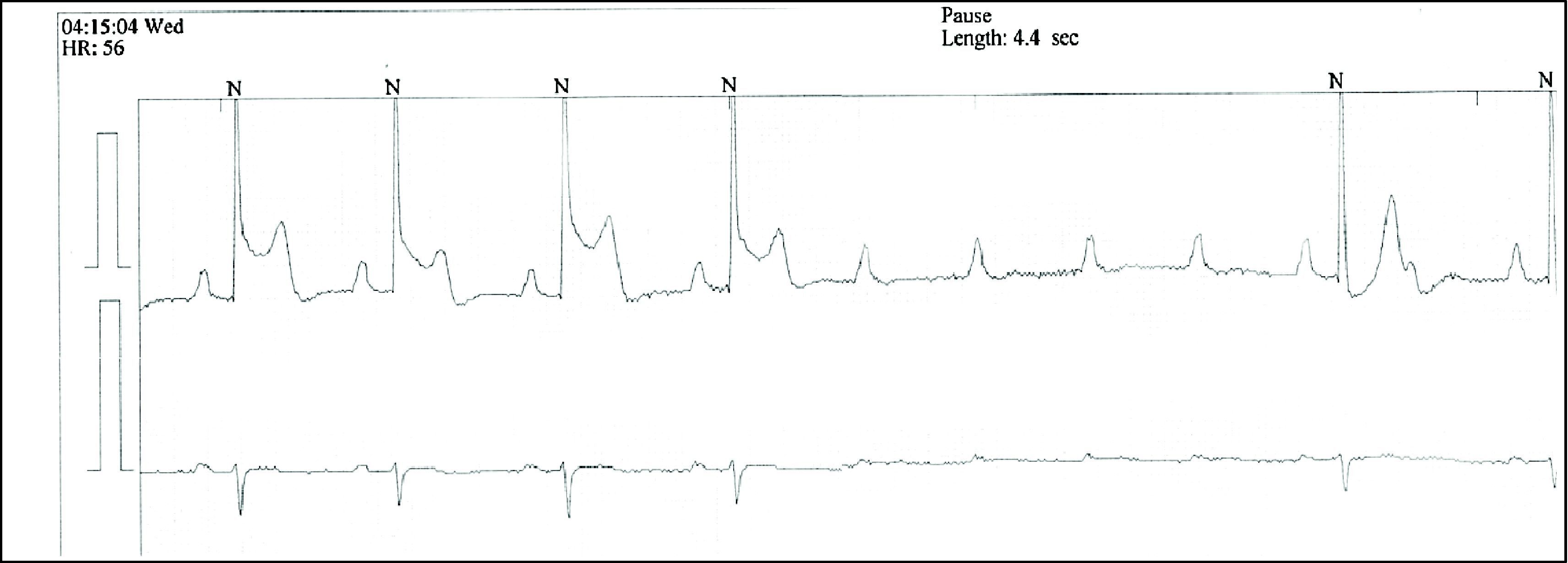
The patient was admitted to the coronary care unit for surveillance and urgent cardiac catheterization. The results of the complementary exams that she had brought to the consultation were analyzed, including 24-h Holter monitoring, which showed basic sinus rhythm with periods of first-degree atrioventricular block (AVB) and multiple periods of high-degree AVB, some asymptomatic, including complete block, with prolonged ventricular pauses lasting up to 4.4s. Multiple periods of ST-segment elevation were also recorded. There was concordance between the pattern of ST-segment elevation and the periods of high-degree atrioventricular conduction disturbance, mainly at night (Fig. 2).
Coronary angiography excluded significant coronary artery disease and echocardiography showed good left ventricular function and no wall motion abnormalities. Serial markers of myocardial necrosis were negative.
Therapy with oral nitrates, nifedipine 30mg and simvastatin 40mg was begun. Holter monitoring was repeated on the 3rd and 7th days of hospital stay, and showed no alterations.
The patient was discharged on the 8th day under the above medication and was advised to quit smoking.
She continued to be followed in cardiology consultations, which, despite compliance with medication and smoking cessation, showed persistence of symptoms and of the ECG alterations documented by Holter, with significant pauses, some asymptomatic. Nifedipine was replaced by verapamil 120mg/day, without success. Catheterization was repeated, which confirmed the absence of significant lesions; the passage of the catheter triggered spasm of the left main coronary artery, which resolved with intracoronary administration of isosorbide dinitrate.
The patient was referred for pacemaker implantation in May 2010. Recent 24-h Holter monitoring showed sinus rhythm alternating with periods of DDD pacing. She still experiences episodes of chest pain, but without syncope.
DiscussionPrinzmetal angina, also known as vasospastic angina, is characterized by episodes of chest pain at rest associated with ECG alterations caused by transient coronary artery spasm. The most common ECG feature is ST-segment elevation.1 In 25% of cases these alterations are followed by various types of arrhythmia, including ventricular extrasystoles, ventricular tachycardia, ventricular fibrillation (rare), AVB or supraventricular arrhythmias.1–3
Ventricular arrhythmias are more often associated with ST-segment elevation in the anterior leads, and bradyarrhythmias when located in the inferior leads. Transient high-degree AVB is frequently associated with hypotension and syncope.4
Although some of these arrhythmias can be fatal, the appropriate treatment for vasospastic angina in the absence of significant coronary stenosis is with nitrates and calcium channel blockers, and is associated with good short- and long-term prognosis. Smoking cessation is essential, as smoking can trigger vasospasm. Few cases in the literature have required implantation of a pacemaker or cardioverter-defibrillator, although this option should be considered whenever there are arrhythmic episodes that are refractory to optimal medical therapy. Beta-blockers, especially if non-selective, can trigger or prolong episodes of coronary artery spasm and should therefore be avoided.5
In the case presented an attempt was made to control coronary spasm, and consequently the episodes of AVB. The patient's failure to respond to increasing doses of calcium channel blockers and nitrates led to pacemaker implantation five months later. This is a last-resort treatment and should not be considered for several months, as cases of late response to medication have been reported.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ferreira, F. Bloqueio auriculo-ventricular de alto grau induzido por angina de Prinzmetal. Rev Port Cardiol 2012. doi:10.1016/j.repc.2012.01.001.