Heart failure is a major public health problem that affects a large number of individuals and is associated with high mortality and morbidity. This study aims to estimate the probable scenario for HF prevalence and its consequences in the short-, medium- and long-term in Portugal.
MethodsThis assessment is based on the EPICA (Epidemiology of Heart Failure and Learning) project, which was designed to estimate the prevalence of chronic heart failure in mainland Portugal in 1998. Estimates of heart failure prevalence were performed for individuals aged over 25 years, distributed by age group and gender, based on data from the 2011 Census by Statistics Portugal.
ResultsThe expected demographic changes, particularly the marked aging of the population, mean that a large number of Portuguese will likely be affected by this syndrome. Assuming that current clinical practices are maintained, the prevalence of heart failure in mainland Portugal will increase by 30% by 2035 and by 33% by 2060, compared to 2011, resulting in 479921 and 494191 affected individuals, respectively.
ConclusionsIn addition to the large number of heart failure patients expected, it is estimated that the hospitalizations and mortality associated with this syndrome will significantly increase its economic impact. Therefore, it is extremely important to raise awareness of this syndrome, as this will favor diagnosis and early referral of patients, facilitating better management of heart failure and helping to decrease the burden it imposes on Portugal.
A insuficiência cardíaca é um problema grave de saúde pública que atinge um elevado número de indivíduos e está associada a mortalidade e morbilidade elevadas. O presente estudo tem como objetivo estimar o cenário provável no que respeita à prevalência de IC em Portugal e respetivas consequências a curto, médio e longo prazo.
MétodosA presente avaliação tem por base o projeto EPICA (EPidemiologia da Insuficiência Cardíaca e Aprendizagem) desenhado para obter estimativas de prevalência de insuficiência cardíaca crónica em Portugal continental, em 1998. Foram feitas estimativas de prevalência de insuficiência cardíaca, para indivíduos com idade superior a 25 anos, distribuídos por faixa etária e por sexo, recorreu-se aos dados do Censo 2011, desenvolvido pelo Instituto Nacional de Estatística.
ResultadosBaseados nas alterações demográficas esperadas, associadas a um envelhecimento marcado da população, iremos encontrar um número muito elevado de portugueses afetados por essa síndrome. Assumindo a manutenção das práticas clínicas atuais, estima-se que a prevalência de insuficiência cardíaca em Portugal continental aumente em cerca de 30% em 2035 e 33% em 2060, relativamente a 2011, com um número de 479921 e 494191 indivíduos afetados para 2035 e 2060, respetivamente.
ConclusõesPara além do elevado número de doentes esperado, estima-se que as hospitalizações e a mortalidade associadas à síndrome aumentem significativamente o impacto económico da IC. Nesse sentido, revela-se de extrema importância a consciencialização para a síndrome, o que facilitará o diagnóstico, a referenciação precoce de doentes e uma melhor gestão da insuficiência cardíaca, diminuindo o peso da doença em Portugal.
Heart failure (HF) is a serious public health problem that, despite advances in both pharmacological and non-pharmacological treatment and in the management of the condition, affects a significant number of people and is associated with high mortality and morbidity.1,2 It is a clinical syndrome characterized by symptoms and signs caused by objective cardiac dysfunction.1
The main risk factors predisposing to HF among the general population include coronary artery disease, hypertension, hypercholesterolemia, diabetes, smoking and obesity.3 The presence of multiple comorbidities is one of the main determinants of both prognosis and quality of life.4–6
Several studies have been published on the prevalence of HF. However, due to differences in populations and in the criteria used for both defining and diagnosing HF, the results obtained are divergent and there is a lack of agreement on estimates of prevalence and incidence of the syndrome.1,4
Nevertheless, the prevalence of HF in developed countries is estimated to be around 2% in the adult population, and the incidence data suggest that HF affects 5-10 people in every 1000 per year. Various studies have indicated that both frequency measures rise with advancing age.2,5 In Portugal, the EPICA (Epidemiology of Heart Failure and Learning) study suggested that the overall prevalence of chronic HF in the adult population was 4.36%, reaching 12.67% in those aged 70-79 years and 16.14% in those aged 80 and over.5 The syndrome has a significant economic impact; in developed countries, the direct costs of HF account for about 2% of total healthcare budgets.3 Globally, it is estimated that this figure amounted to 102 billion euros in 2012, in a sample that included 92.4% of all countries and 98.7% of the world's population at the time.7
With the aging of the Portuguese population, together with the increased survival of patients with coronary artery disease, the impact of the syndrome is expected to increase substantially.8 This publication aims to assess and forecast the most likely prevalence scenario and the associated consequences if no measures are taken to reduce the impact of the syndrome in the coming years.
MethodsTerminology and study populationThis assessment is based on the EPICA study,5 data from the 2011 census and population projections for 2018, 2035, 2060 and 2080, using data from Statistics Portugal (INE, the National Institute of Statistics).
The EPICA study was a cross-sectional observational study based on a sample of adult patients from health centers in mainland Portugal. The sample, which was representative of the population as a whole, was studied between 1998 and 2000.5 The primary objective was to estimate the overall prevalence of chronic HF, by age and gender, following the European Society of Cardiology's recommendations on the diagnosis of HF at that time: symptoms and signs compatible with HF and objective evidence of cardiac dysfunction. The following age groups were established for analysis: 25-49 years, 50-59 years, 60-69 years, 70-79 years, and 80 and over.
According to the predominant type of cardiac dysfunction, identified by echocardiogram, five HF subtypes were defined: HF due to left ventricular (LV) systolic dysfunction (LV shortening fraction <28% in the absence of wall motion abnormalities, equivalent to LV ejection fraction [LVEF] <45%); HF with preserved systolic function (LV shortening fraction ≥28%, equivalent to LVEF ≥45%); due to valvular disease; due to pericardial disease; and right HF. Other cases were classified as multifactorial.5
Statistical analysisThe EPICA study provided HF prevalence estimates for individuals aged over 25, distributed by age group and gender. Overall HF prevalence, as calculated in the EPICA study, was 4.36%. At the time, this meant 264000 people in Portugal suffered from the syndrome. More specifically, estimated HF prevalence by age group was as follows: 25-49 years, 1.36%; 50-59 years, 2.93%; 60-69 years, 7.63%; 70-79 years, 12.67%; 80 and over, 16.14%.
Data from the 2011 Census conducted by INE were used to calculate the resident population of mainland Portugal. The population projections for 2018, 2035, 2060 and 2080 were drawn from INE data, on the basis of provisional estimates of the resident population as at December 31, 2015. INE calculated resident population projections using the cohort component method. This involves formulating hypotheses for future fertility, mortality and migration levels.9
The central scenario was assumed, as were the central hypotheses for fertility and mortality and the optimistic scenario for migration. This set of hypotheses expresses the most likely population growth, given recent demographic developments. According to INE, the central fertility hypothesis presupposes a moderate recovery in fertility levels, with the total fertility rate (TFR) reaching a value midway between the pessimistic and optimistic hypotheses by 2080: 1.55 children per woman. The central mortality hypothesis presumes that the recent trend of lower mortality will continue, with life expectancy at birth in Portugal in 2080 reaching 87.38 years for men and 92.10 years for women. The optimistic hypothesis for migration considered the possibility of the migratory balances recovering to higher positive values, and reaching a positive migratory balance of 29892 in 2080.9
The estimated prevalence rates for each age group and gender were multiplied by the absolute values obtained in the 2011 Census and by the population projections for 2018, 2035, 2060 and 2080, in order to estimate the number of individuals with HF in the years in question.
The number of discharged patients and the in-hospital mortality rate were calculated on the basis of the 2011 prevalence estimates and data from the 2015 report from the National Program for Cerebro-Cardiovascular Diseases, published by the Directorate-General for Health.10
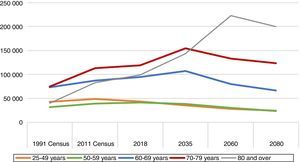
ResultsNumber of individuals affected by the syndromeThe present projection suggests that the numbers of HF patients in mainland Portugal will rise by around 7% in 2018, 30% in 2035 and 33% in 2060 compared to the 2011 figure, meaning 397805, 479921 and 494191 individuals, respectively, will be affected. The number of HF patients in 2080 is expected to be 437004, given that the country's population is forecast to fall from 10.3 to 7.5 million (Table 1).9Figure 1 details the estimates by age group.
Estimates of absolute numbers of different types of heart failure in the population of mainland Portugal aged over 25 years.
| HF subtype | Systolic dysfunction | Preserved systolic function | Valve disease | Pericardial disease | Right HF |
|---|---|---|---|---|---|
| EPICA prevalences | |||||
| 1998-2000 | |||||
| M (%) | 1.91 | 0.88 | 0.68 | 0.05 | 0.63 |
| F (%) | 0.75 | 2.42 | 0.70 | 0.03 | 0.28 |
| 2011 Census | |||||
| M | 66715 | 30738 | 23752 | 1746 | 22006 |
| F | 29933 | 96584 | 27937 | 1197 | 11175 |
| MF | 96648 | 127322 | 51689 | 2944 | 33181 |
| Central scenario | |||||
| 2018 | |||||
| M | 65408 | 30136 | 23287 | 1712 | 21574 |
| F | 29988 | 96762 | 27989 | 1200 | 11196 |
| MF | 95396 | 126898 | 51276 | 2912 | 32770 |
| 2035 | |||||
| M | 65441 | 30151 | 23298 | 1713 | 21585 |
| F | 30156 | 97303 | 28145 | 1206 | 11258 |
| MF | 95597 | 127454 | 51444 | 2919 | 32843 |
| 2060 | |||||
| M | 57769 | 26616 | 20567 | 1512 | 19055 |
| F | 26430 | 85282 | 24668 | 1057 | 9867 |
| MF | 84199 | 111898 | 45235 | 2569 | 28922 |
| 2080 | |||||
| M | 51381 | 23673 | 18293 | 1345 | 16948 |
| F | 22356 | 72134 | 20865 | 894 | 8346 |
| MF | 73737 | 95807 | 39158 | 2239 | 25294 |
F: female; MF: sum of male and female; HF: heart failure; M: male.
The projections indicate that the numbers of over-60s with HF will be 312649 in 2018, 405897 in 2035, 436506 in 2060 and 389130 in 2080.
Notably, there will be a considerable increase in the number of HF patients over the age of 80, particularly as from 2035, when this age group will begin to outstrip all the others. In 2011, an estimated 83019 HF patients were in this age group. This figure is expected to rise by 20% by 2018, by 73% by 2035 and by 168% by 2060.
According to the EPICA study, the most common form of HF is HF with preserved systolic function, followed by HF due to systolic dysfunction. It is estimated that 126898 patients will be suffering from HF with preserved systolic function in 2018. There will be a much higher prevalence among women, 96762 of whom will have this form of HF in that year.
Systolic dysfunction will be more prevalent among men, 65408, 65441, 57769 and 51381 of whom are likely to be affected by this type of HF in 2018, 2035, 2060 and 2080, respectively.
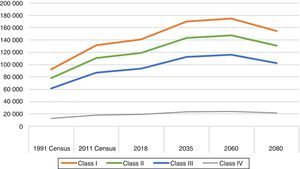
The number of individuals with HF according to the New York Heart Association (NYHA) classification was also estimated. Thus, it is expected that 122781 patients will be in NYHA class II in 2035, compared to over 136000 patients who will be classified as class III or IV (Figure 2).
Hospitalization and mortalityIn 2011, an estimated 371264 patients over the age of 25 suffered from HF. The 2015 report from the National Program for Cerebro-Cardiovascular Diseases revealed that a total of 15624 patients were discharged from hospital following an acute HF episode. On this basis, the projections for 2018, 2035, 2060 and 2080 indicate that the number of HF patients who will be discharged from hospital will be 16708, 20157, 20756 and 18354, respectively. If the in-hospital mortality rate remains at the 2014 level of 12.5%, it is estimated that the numbers of in-hospital deaths for patients admitted with acute HF in these years will be 2088, 2520, 2595 and 2294, respectively.
DiscussionAmong the various factors that contribute to the increase in the prevalence of HF, aging plays a central role. Resident population projections suggest Portugal's population will decline because of a decrease in the number of births. As a result, a fall in the number of HF patients would also be expected. However, the aging of the population works against this expectation, and the number of HF patients is likely to rise to 494141 by 2060. This projection indicates that, by 2018, the number of patients over the age of 60 (312649) will be greater than the figure previously estimated in the EPICA study for adults with HF of all ages (around 264000).5
Similar results were obtained by a study carried out in the USA that used a similar methodology to this analysis.11 The American study found that the number of HF patients in the country would be around eight million in 2030, corresponding to 46% more affected individuals than in 2012. In Portugal, the number of adult HF patients in 2035 is expected to be around 30% above the figure for 2011. Given the expected aging of the population in the USA, it is estimated that the number of patients over the age of 80 in 2030 will be 66% higher than in 2012.11 In Portugal, the increase between 2011 and 2035 for this age group is expected to be similar, at around 73%. Considering the above, demographic changes foreshadow a rapid increase in the number of HF patients.
An analysis of the projections by HF subtype indicates that by 2018 there will be 126898 individuals with HF with preserved systolic function, most of whom will be elderly and female, in agreement with the existing literature.12 Given the population trends identified by INE, the prevalence of this HF subtype is expected to increase. It should be noted that there is less consensus, and therefore more of a challenge, regarding the diagnostic criteria for HF with preserved LVEF. Furthermore, there is still no treatment capable of objectively reducing mortality in this entity, unlike HF with reduced LVEF.2 An epidemiological change in HF is probably underway, given that various studies have found that HF with preserved LVEF is on the rise. This is at least partially attributable to the aging factor and to the increase in the risk factors and comorbidities that accompany and contribute to the development of HF, and also to a lower prevalence of HF with reduced LVEF.13
The NYHA functional classification is one of the strongest independent prognostic predictors for HF.2,4 By 2035, the number of outpatients in NYHA class III and class IV is expected to be over 136000. These more serious stages of the disease are associated with more complex patient management and a greater impact on the national health system (NHS), as a consequence of increased hospitalizations and rises in morbidity and mortality. The available data show that hospitalization accounts for up to 80% of the costs of the syndrome. Furthermore, the number of patients in class IV was probably underestimated by the EPICA study, given that the study focused on outpatients, and is probably much higher, since patients at this stage of the disease are more likely to be treated in a hospital setting.
A number of studies that examined trends in HF hospitalization over the years have found that, for the elderly, hospitalizations reached a peak in the 1990s but have since fallen off. Factors that contribute to fewer hospitalizations include reduced and/or improved medical control of risk factors such as hypertension and smoking, a decrease in the incidence of acute myocardial infarction, the establishment of multidisciplinary HF management programs, and an increase in the number of patients who are diagnosed earlier and receive treatment through the primary healthcare system.4,14,15
Nevertheless, the fact that HF is the major cause of hospitalization in the over-65s attests to the impact of this syndrome in developed countries.16,17 In Portugal, a study using the national database of Diagnosis Related Groups (DRG) assessed trends in HF hospitalization between 2000 and 2015 and found that the number of patients hospitalized for HF doubled, particularly in the 66-80 and over-81 age groups. There was a strong correlation between these figures and the attendant risk factors.18 Given, also, that the Portuguese population is aging, there is likely to be a significant rise in the number of hospitalizations and in the direct medical costs of HF treatment, unless specific preventative steps are taken and practices altered. In view of the 2015 report on Cerebro-Cardiovascular Diseases, this projection is very much in line with expectations for 2018, 2035, 2060 and 2080, when the numbers of patients discharged after an acute HF episode are projected to be 16708, 20157, 20756 and 18354, respectively.10 The same report also shows that in-hospital mortality due to HF fell by 9.90% between 2010 and 2014.10 Schmidt et al. assessed the trend for HF hospitalizations and mortality rates over the last 30 years in a Danish cohort and found that one-year and one- to five-year mortality also declined consistently between 1983 and 2012, falling more than 40% overall.15 It should be noted that, in its calculation of HF hospitalizations, the report on Cerebro-Cardiovascular Diseases, which made use of the DRG coding base, only took into account the DRG code for the main diagnosis (ICD-9-CM: 428). As HF hospitalizations may be coded by more than one identifier and as the HF code may appear as a secondary diagnosis if the main reason given for hospitalization arose from the acute episode itself (infection or arrhythmia, for example), this report is unlikely to accurately reflect the actual number of hospitalized HF patients, which is very likely higher.10,19
Moreover, there are no data available regarding the total number of HF hospital admissions in Portuguese emergency departments. Readmissions are a significant factor in HF management. Hospitalization is followed by readmission 30 days later in around 24% of cases,20 and this rises to 50% after six months.21 There is thus a critical need to assess this indicator in Portugal, since a reduction in readmission rates could lead to lower costs and improved healthcare provision and is an important focus in performance indicators for both public and private payers.22
Given the data presented above, there is a firm conviction that the prevention and early diagnosis of HF, based on an understanding of its epidemiology, could have a significant effect in terms of improving quality of life and mortality and simultaneously reducing healthcare costs.8,17,23
It is also important to optimize the therapeutic approach to HF patients with reduced LVEF. The ESC Heart Failure Long-Term Registry, maintained by the European Society of Cardiology, shows that between 2011 and 2013, despite the widespread usage of the disease-modifying pharmacological treatments recommended in the guidelines, only a third of patients received the maximum tolerated dosage deemed appropriate.24 The European SHAPE study on perceptions of HF found that general practitioners had low levels of understanding of the syndrome and of the treatment options.25 Furthermore, the general public appeared to be largely unaware of the nature, seriousness, therapeutic options and associated costs of HF. Thus, it is unlikely that either the general public or healthcare professionals will pressure the health authorities to take appropriate action.25
The importance of heart failure is also somewhat underestimated in Portugal, by both health professionals and decision-makers. This is reflected in the lack of definition of HF care flows and structures at various levels of the NHS, and also in the lack of communication between the various parties involved in HF treatment.8
The difficulty that the general public and patients have in recognizing both the symptoms and the seriousness of the syndrome means that there are often delays before medical advice is sought. HF awareness needs to be improved, particularly regarding identification of the syndrome and recognition of its etiology. This would then encourage patients to change their lifestyles and help bring down risk.
A key priority, therefore, must be proper management of the patient and the disease through the National Health Plan, if we are to turn these projections around and reduce the associated burden.8,17,26
Study limitationsThese projections are based on the prevalences estimated almost 20 years ago in the EPICA study. No additional recent studies of HF prevalence have been carried out in Portugal, which is why we made use of the EPICA prevalence figures and INE population estimates.
Bearing in mind that this analysis is based on the EPICA data, the limitations of that study also pertain here. Prime among these was the fact that the sample consisted of patients followed through the primary healthcare system and not the population in general. Given that such patients will tend to be less well than the population in general, it is plausible to assume that they will suffer from more serious heart disease. Furthermore, it is probable that the number of patients in NYHA class IV has been underestimated, given that such patients usually receive in-hospital treatment and the EPICA study looked at outpatients only. Moreover, as the population in general was not assessed by the EPICA study, the numbers obtained are presumably lower than the real figures.
Finally, it should be noted that INE projections are constrained by the structure and composition of the population at the starting point and also by the different fertility, mortality and migration patterns used in each of the hypotheses. It should also be borne in mind that the longer the projection period, the greater the associated uncertainty.
ConclusionsHF is one of the main causes of morbidity and mortality. It primarily affects the elderly and has a significant impact on the patient and on society in general.13,17
The demographic changes that are expected to ensue from the marked aging of the population suggest that a considerable number of Portuguese will be affected by the syndrome in the coming years. The actual number may double from current levels to around half a million by 2035. The real prevalence of HF in Portugal today is unknown, which is why it is so important to arrive at an estimate that is based on epidemiological data. This is crucial to healthcare decision-making and resource allocation.17
In addition to the large number of patients expected, hospitalizations and mortality associated with this syndrome are likely to significantly increase the economic impact of HF. It is critically important to raise awareness of the syndrome, to facilitate early diagnosis and patient referral. This will result in better HF management and consequently improved patient lifestyles and lower disease management costs.
The possibility of forecasting, as accurately as possible, the expected increase in the number of patients with HF and its consequences in the short, medium and long term is crucial to a proper understanding of the burden and costs of the disease and the development and implementation of strategies that could reverse these trends to some degree and thus significantly reduce the anticipated epidemic.
Conflicts of interestCândida Fonseca is a consultant for Novartis, Orion, OM Pharma, Bayer and Servier (companies that develop and market treatments for heart failure and its associated comorbidities) and sits on the executive and scientific committees of clinical research studies run by Novartis, Servier, Orion, Bayer and OM Pharma. She has also received fees for speaking on heart failure from Novartis, Servier and Orion. Inês Araújo has received speaker fees from Servier, Novartis and Orion. She is also a co-investigator for HF clinical studies run by Servier, Novartis and Bayer. Fátima Ceia has no conflicts of interest to declare. Daniel Brás is employed by Novartis Farma S.A., Porto Salvo, Portugal.
Novartis Farma – Produtos Farmacêuticos S.A. provided financial support for the scientific editorial work. We would like to thank Marta Maia (W4Research, Lda.) for her scientific and editorial support.
Please cite this article as: Fonseca C, Brás D, Araújo I, et al. Insuficiência cardíaca em números: estimativas para o século XXI em Portugal. Rev Port Cardiol. 2018;37:97–104.