Heart failure is a syndrome with high prevalence, morbidity and mortality, but awareness of the disease is poor among the general public and policy makers. This document, which was prepared by a group of experts consisting of cardiologists, internists and general practitioners, aims to set out in detail the problem of heart failure in Portugal at several levels: burden of the disease, diagnosis, treatment and monitoring. To this end, different aspects of the management of the various stages of the disease are identified and discussed in detail, covering both outpatients and hospitalized patients. In order to optimize the medical care provided to these patients, various short-, medium- and long-term solutions and strategies are put forward that have the potential to improve the integration and use of available resources. The intention is to highlight strategies that are not based on a single model but can be adapted to different regional circumstances, in order to increase awareness and improve management of heart failure in Portugal.
A insuficiência cardíaca é uma síndrome com elevada prevalência, morbilidade e mortalidade, sendo, no entanto, pouco reconhecida junto dos cidadãos e decisores políticos. O presente documento foi elaborado por um conjunto de peritos constituído por médicos especialistas em cardiologia, medicina interna e medicina geral e familiar, e pretende expor detalhadamente o problema da insuficiência cardíaca em Portugal a vários níveis: peso da síndrome, diagnóstico, tratamento e acompanhamento dos doentes. Para tal, são identificados e discutidos em detalhe os diferentes aspetos inerentes ao manejo da síndrome durante o processo assistencial, nas várias fases da doença e que incluem doentes hospitalizados e em ambulatório. De modo a otimizar a assistência médica prestada a estes doentes, são apontadas diversas soluções e estratégias a curto, médio e longo prazo com potencial para melhorarem a articulação e utilização dos recursos disponíveis. Pretendeu-se desta forma destacar estratégias que, não se traduzindo num modelo único de melhoria, poderão ser adaptadas às diferentes especificidades regionais, de modo a aumentar o reconhecimento e a atenção prestada à insuficiência cardíaca em Portugal.
Heart failure (HF) is a syndrome with high prevalence, morbidity and mortality that represents a considerable economic and social burden. However, in Portugal awareness of the disease is poor among the general public and policy makers. In addition, there has been a lack of concerted efforts in the medical profession to organize the health care process more efficiently, which is essential to improve management of the syndrome and thus to have a positive effect on health indicators. In view of the current and future importance of HF – which is expected to increase in prevalence and incidence – it must be seen as a priority in health care in Portugal, and the National Health Service (NHS) should be given the necessary means to improve its performance in clinical terms as well as in its organizational and funding framework.
The present document aims to raise awareness of the urgent need to prioritize HF in the health agenda given its current prevalence and the increase expected in the near future, the associated high mortality and morbidity and the socioeconomic burden for patients, their families, and society. It also aims to help identify the main shortcomings in the management of HF and to propose solutions at different levels of care that will lead to improved integration between the different specialists involved in the diagnosis, treatment and monitoring of HF patients at the national level.
This analysis is intended for physicians, particularly those involved in the management of HF patients (cardiologists, internists, intensivists and general practitioners [GPs]), nurses, and health decision-makers, whose determinations may influence attitudes to HF. It is also intended to act as a guide for future initiatives aimed at raising awareness among the general public.
The authors of the present document, who are cardiologists, internists and GPs, work within the NHS, in hospitals (including emergency departments) and in primary health care. The opinions expressed here are based on their personal experience, both clinical and organizational, and are supported by the guidelines published by the European Society of Cardiology (ESC) and the American College of Cardiology/American Heart Association (ACA/AHA). This consensus statement is endorsed by the main medical societies and associations involved in the treatment of HF (Appendix 1).
Heart failure in the world and in Portugal: the burden of the syndromeHF is defined as a syndrome caused by a structural and/or functional cardiac abnormality, resulting in inadequate cardiac output for the metabolic needs of the organism at rest or during exercise.1 In most cases it is the final stage of a continuum initiated by cardiovascular risk factors, which begin earlier in life than previously thought and progress to cardiac dysfunction.2 It may be asymptomatic at first, with symptoms only appearing later. Typically, the syndrome develops in episodes of decompensation that weaken the patient's clinical condition, contribute to worsening HF and require urgent medical care. This continuum can be interrupted without warning, at any time, by sudden death or culminate in death due to pump failure.
Heart failure in the worldHF prevalence increases with age, particularly after the age of 65, mainly due to the greater incidence of hypertension and myocardial infarction (MI) after this age and to increased survival of patients after MI.3 HF affects 1-2% of the world's population and 6-10% of those aged over 65.3,4 Worldwide, around 26 million adults suffer from HF, on a par with the 32 million with cancer and the 34 million with HIV/AIDS.3 The most recent projections indicate that its prevalence will rise by 25% by 2030.5
Episodes of decompensation frequently require visits to the emergency department and hospitalization or rehospitalization. In developed countries, HF accounts for 1-4% of all hospitalizations,3 and is the leading cause of admission in individuals aged over 65 in Europe and the USA.1 Around a quarter of these patients are rehospitalized within a month of discharge.4,6
Each hospitalization represents a further worsening of HF, contributing to the decline in the patient's clinical condition, until death results. In Europe, in-hospital mortality from HF is 7-9%,7 a higher figure than for MI.8 Mortality can reach 27% at six months after hospitalization for HF9 and 50% at 12 months in those admitted with cardiogenic shock.10 Over 50% of HF patients die within five years of diagnosis, which represents a lower survival rate than some types of cancer, including breast, prostate and colon cancer and leukemia.3,11
The economic burden of HF is considerable worldwide, accounting for 1-3% of health budgets in the USA and Europe, where it has the greatest economic impact of all diseases.3 In the USA, spending on HF is more than double that of spending on all cancers combined.12 Furthermore, the costs of hospitalizations are considerable, direct medical costs accounting for 68% of the total costs of HF in the USA and Europe.13
Heart failure in Portugal: from cardiovascular risk factors to socioeconomic impactThere is a high prevalence of cardiovascular risk factors in Portugal: 24% of the population are smokers14 and 27.5% have metabolic syndrome.15 The country has one of the highest rates of increase in prevalence of overweight and obesity in Europe (53% in those aged between 18 and 64).16 In addition, three million Portuguese have diabetes or impaired glucose metabolism.17 Hypertension affects 42% of adult Portuguese18 and there are around 12000 cases of MI every year.8
The overall prevalence of chronic HF in Portugal was estimated at 4.36% in the EPICA study (1998–2000), ranging from 1.36% in those aged 25-49 to 16.14% in those aged over 80.19 Bearing in mind the aging of the population over the last 20 years, these figures are now undoubtedly higher; on the basis of the prevalence in each age-group in the EPICA study and data from the 2011 census, there may now be as many as 380000 cases of HF in Portugal.20
A report by the Portuguese Directorate-General for Health (DGS), “Cerebral and Cardiovascular Disease in Numbers 2015”,8 cites a principal diagnosis of HF as the second leading source of hospital production, accounting in 2014 for 182512 days of hospitalization (1.9 times more than MI) and 18588 patients discharged after admission for decompensated HF. Mean hospital stay for HF was 9.8 days in 2014. HF is responsible for the highest in-hospital mortality of all cerebral and cardiovascular disease in the country, reaching 12.5%.8
In addition, HF is often presented as a secondary diagnosis in medical records, so the actual number of patients hospitalized for HF is higher than reported.21 According to a report from medical consultants IASIST Portugal, “Impact of hospitalization of chronic patients on the NHS”, the number of HF admissions rose by 33% between 2004 and 2012,22 but this number is probably an underestimate, in view of shortcomings in the coding of a diagnosis of HF.21 The rate of hospitalization for HF in 2009 was 27.9/100000 population, similar to that for diabetes (30.0/100000), asthma (29.5/100000) and chronic obstructive pulmonary disease (COPD) (29.4/100000), some of the major epidemics of the 21st century.22,23 However, in 2012 the mortality rate for HF (12.9%) was higher than for diabetes (5.1%), asthma (0.8%) and COPD (7.5%), and the same trend was seen for rehospitalizations (14.6% for HF, 8.2% for diabetes, 5.1% for asthma and 14.0% for COPD).22
The readmission rate, particularly at 30 and 60 days, is increasing, which has serious economic and health care implications.22 Official data show that the cost of HF hospitalizations in Portugal in 1998 was approximately 24 million euros,24 similar to that of hospitalizations for COPD in the same year (23 million euros).25 Almost 20 years later, the growing prevalence of HF and the increasing sophistication of medical care mean that this figure is likely to be much higher.
Patients hospitalized for HF consume large quantities of resources, due to the high cost of the complex diagnostic exams, drugs, medical devices and surgical procedures that are often required.23 The cost of health care for HF patients is estimated to be well above what is allocated to them by the NHS.
The physical and psychological effects of HF also have important psychosocial implications, such as social isolation, anxiety, frustration and depression, with negative effects on the quality of life of both patients and their caregivers.26 There are no data available for the effects of HF on absenteeism and loss of productivity in Portugal, but this is another important aspect of the burden of HF with repercussions not only for the health system but also for society and the economy.
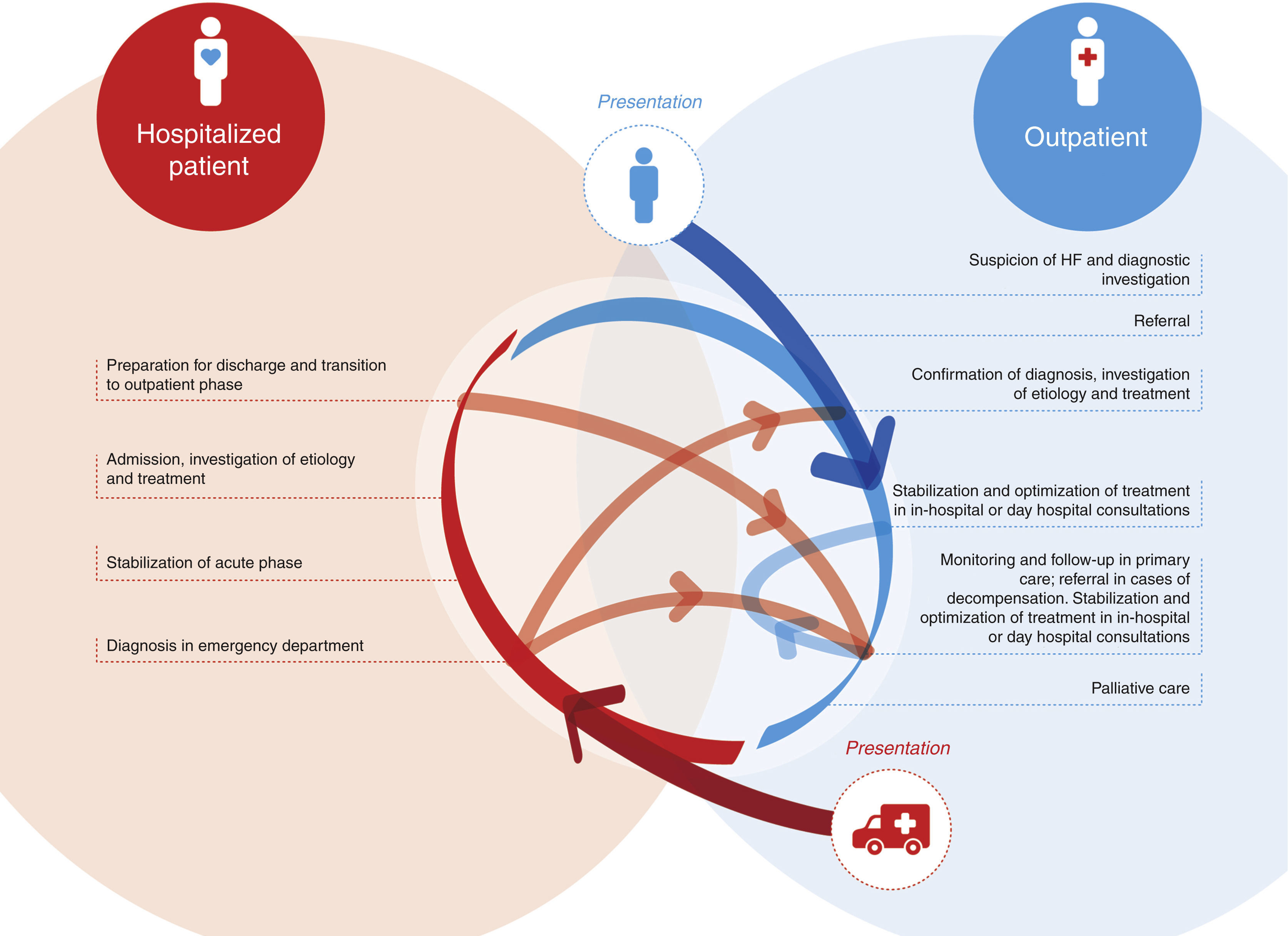
The problems with heart failure treatment in PortugalLack of awareness of the importance of heart failure and of an integrated approachThe basic problem with HF in Portugal is that there is no integrated approach on the part of those responsible for its management (Figure 1). The result is a lack of awareness of its importance and of its impact on the general population.
Health care flows for the treatment of heart failure, showing the need for multidisciplinary teams to ensure the integrated management of the syndrome and provide health care in accordance with the international guidelines.1 HF: heart failure.
Official data on HF in Portugal are also limited and do not fully characterize the real course and management of the syndrome. The only study to date on the prevalence of heart failure in Portugal was published nearly 15 years ago,19 and there are no current data on changes in its prevalence and, more importantly, in its diagnosis and treatment. There are also gaps in the information on HF in the National Program for Cerebral and Cardiovascular Disease of the DGS, which does not provide numbers of rehospitalizations or of emergency department admissions for HF. In addition, the hospital production described in the DGS report is based on the coding of diagnosis-related groups (DRGs), which, as stated above, does not always reflect the real number of patients hospitalized for HF.21
Lack of a structural debate on heart failure within and between specialtiesUnderstanding of the actual importance of heart failure in the medical profession is patchy and there is little or no discussion of the role of the different specialties that deal with the condition. There is thus a need to organize the health care flows and to clearly define responsibilities, in order to ensure that optimal support is provided from the beginning to the end of the patient's journey through the health system.
The main players in the management of HF are GPs, cardiologists, internists, intensivists and nurses, but HF patients frequently present multiple comorbidities and therefore other specialists also have an important role in clinical management of the syndrome.
Since different specialists will be involved in the management of an individual patient, effective communication and collaboration between them and between the various levels of health care are essential. It has been shown that HF patients are better treated in integrated management programs and by specialized multidisciplinary teams (Figure 1).1,27
However, despite the existence of the online Health Data Platform (PDS), there are weaknesses in the flow of information between the different levels of health care. Communication between primary care centers and hospitals, particularly the cardiology and internal medicine departments, as well as between hospital departments, is clearly in need of improvement.
Lack of an integrated health care process for the management of heart failure and deficiencies throughout the patient's journey through the health systemThe lack of a properly organized integrated health care process for the management of heart failure is reflected in a wide range of deficiencies throughout the patient's journey through the health system (Figure 1).
DiagnosisIn Portugal, HF is often diagnosed late, frequently at the time of the first hospitalization, instead of being suspected and diagnosed early by the patient's GP. This is largely due to a lack of awareness of the disease and failure to recognize the characteristic symptoms and signs.
A suspected diagnosis of HF on the basis of symptoms and signs, and an electrocardiogram and/or chest X-ray, should be confirmed by objective evidence of cardiac dysfunction, and so other diagnostic exams are needed, such as B-type natriuretic peptide (BNP) or N-terminal BNP (NT-proBNP) measurement and/or imaging studies, of which echocardiography is the most accessible.1,27
GPs do not have easy access to BNP or NT-proBNP measurements, which are not reimbursed by the NHS for outpatients. Due to their high negative predictive value, low BNP/NT-proBNP levels can avoid false-positive diagnoses of HF and unnecessary use of echocardiography, which is considerably more costly. Making tests of natriuretic peptide levels available to GPs would improve health care by enabling earlier diagnosis and would reduce costs by avoiding repeat exams, incorrect diagnoses and inappropriate referral for hospital services.
An additional problem is that while echocardiography is now more widely available, the lack of standardization of echocardiographic reports means they are frequently incomplete or inconclusive for confirming or excluding a diagnosis of HF.
Outpatient treatment and referralThere is still uncertainty among GPs as to when to prescribe disease-modifying drugs to treat HF and at what doses. Hospital referral is also subject to certain constraints, and, conversely, communication between hospitals and GPs is limited when patients are returned to primary care after an acute event. There are relatively few HF specialists in Portugal or specialized structures that can provide local health care for HF patients and ensure early treatment of episodes of decompensation. Cardiac rehabilitation programs for HF patients are equally scarce.27
Acute phase and hospitalizationAs with MI, it is essential that acute HF should be treated as rapidly as possible. However, the guidelines are unclear as to the approach to adopt given the lack of solid evidence in this area, relying mostly on the experience of the individual physician.1 There is no standard and systematically applied treatment protocol in Portugal, nor are there adequately trained multidisciplinary teams to implement such a protocol in most emergency, internal medicine or even cardiology departments.
Pre-discharge and vulnerable phasesThere is no organized transition care for HF patients in Portugal. Planning for discharge should include guidance for patients and caregivers, prescription and appropriate titration of all drugs that can modify the course of the disease, sharing of information and scheduling of reassessment consultations within two weeks of discharge, in order to reduce the risk of rehospitalization or death during this vulnerable phase.11 It is also recommended that high-risk patients should be referred for integrated multidisciplinary management programs and cardiac rehabilitation programs.1
Referral for integrated multidisciplinary management programsHF clinics are increasingly important in the care of these patients. Such clinics have multidisciplinary teams made up of specialists in HF (cardiologists, internists, GPs and nurses) and other health professionals, pharmacists, dieticians, physiotherapists, psychologists and social workers, who together provide a systematic approach to HF. These teams have been shown to be cost-effective and to improve patients’ quality of life and reduce hospitalizations and mortality.1
Patients and caregivers need to be educated about the importance of adherence to drug and non-drug therapy and early recognition of decompensation in this phase. This is usually done by nurses, who should also be specialized in HF.
Another essential factor is accessibility to these programs, to enable early treatment of decompensation in day care centers, which will avoid rehospitalization and/or visits to the emergency department and thus reduce costs. Telemedicine for management of outpatients is another promising possibility, although further research is needed.
However, the fact is that these facilities are in short supply in Portugal, as is specialized HF training for nurses.
Cardiac rehabilitationAlso limited, in fact virtually nonexistent, are cardiac rehabilitation programs for HF patients in Portugal, despite their proven benefits, unequivocal recommendations for referral, and the appeal by the Portuguese Society of Cardiology for more action in this area in a document published on the Society's website.28
Palliative and end-of-life careThere is also a need to develop strategies for provision of palliative and end-of-life care for HF patients, which is rarely included in health care planning.
Strategies to improve medical care for heart failure patients in PortugalBelow are suggestions for short, medium and long-term measures required to improve medical care for HF patients.
Short-term measures- 1.
The most urgent measure to improve the current situation would be to bring the different players together to form an alliance dedicated to making HF a health priority and improving its management. This alliance should include:
- •
regulatory and political bodies, especially the Health Commission of the Portuguese Parliament and the Ministry of Health, particularly the DGS and the Program for Cerebral and Cardiovascular Disease;
- •
scientific societies, particularly the Portuguese Societies of Cardiology, Internal Medicine, and Intensive Care;
- •
the Portuguese Medical Council and the Colleges of the various specialties involved in HF treatment;
- •
the Portuguese Nursing Council;
- •
HF patient groups;
- •
the media, as a means of informing and educating the population;
- •
the pharmaceutical and medical device industries, as partners in improving health care.
- •
- 2.
A national plan is needed for training health professionals in HF, particularly physicians and nurses, to encourage specialization in this area. HF should be included in the National Health Plan and clinical guidelines should be drawn up based on the ESC guidelines. The guidelines should be appropriate to the Portuguese context and should take into account the expected increase in HF prevalence in the coming years.
- 3.
HF should be a priority in the next edition of the National Program for Cerebral and Cardiovascular Disease and in local health programs.
- 4.
Diagnosis of HF should be improved by implementing digital diagnostics, and measurement of NT-proBNP should be made available in primary care and be reimbursed by the NHS.
- 5.
A ‘Heart Failure Record’ should be introduced through which clinical information on each HF patient is recorded and can be accessed by all those involved in the care of HF patients.
- 6.
Sharing of best practices should be encouraged between the facilities treating HF patients (cardiology and internal medicine departments and GPs).
- 1.
An information and awareness campaign should be launched directed at the general population, patients, nurses and physicians. This could be linked to initiatives of the ESC and the Heart Failure Association, and of the Portuguese Society of Cardiology via its Working Group on Heart Failure. The campaign should include information on the European Heart Health Charter and the HeartFailureMatters website, aimed at patients and caregivers.
- 2.
An integrated health care process for the management of HF should be established that is codified and applicable throughout the country, beginning with the creation of protocols designed to promote better integration between primary care and hospitals. This will require the setting up of a national network of multidisciplinary teams for the integrated treatment of HF patients. We also suggest the establishment of HF day hospitals and increasing the availability of cardiac rehabilitation programs for HF patients.
- 3.
Performance indicators should be introduced for the medical care of HF patients, for both outpatient and inpatient care, and applicable to hospital departments and GPs. The performance measures recommended by the ESC and the ACC/AHA could be used for this purpose.29,30
- 4.
The definition of HF and its associated costs in the relevant DRG tables, as well as those of HF day hospital sessions, should be revised.
- 5.
Echocardiographic reports need to be standardized at national level in order to improve the quality of information available to physicians.
- 6.
An effective palliative care network that includes HF patients should be implemented.
- 1.
Electronic systems for sharing clinical information need to be improved, particularly the Health Data Platform (PDS).
- 2.
Data collection should be systematized in order to update epidemiological data on HF, which will enable the progress of the disease to be monitored. Such data should include information on quality of life, using standardized questionnaires, and on the impact of the syndrome in terms of absenteeism of patients and caregivers.
HF is a major public health problem in Portugal due to its high prevalence, morbidity and mortality and its considerable economic impact.
Given the wide variations in the country in health care provision for HF patients, at both primary care and hospital level, this document does not suggest a single model for improvement. On the contrary, it is necessary to define and implement strategies that take account of regional differences, in order to optimize existing resources and the links between them.
There is a strong desire for change among Portuguese health professionals who deal with HF. This document, prepared by a group of experts, sets out to analyze the problem, identify deficiencies and propose solutions in order to increase awareness of the need to prioritize the management of HF in the interests of public health care in Portugal.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The present work was supported by an unconditional grant from Novartis.
Endorsed by the Working Group on Heart Failure of the Portuguese Society of Cardiology, the Heart Failure Nucleus of the Portuguese Society of Internal Medicine, the College of General Practitioners of the Portuguese Medical Council, the Cardiovascular Disease Nucleus of the Portuguese Association of General Practitioners, and the Nursing Nucleus of the Portuguese Society of Cardiology.
| Working Group on Heart Failure of the Portuguese Society of Cardiology |
| Cândida Fonseca (coordinator) |
| Dulce Brito |
| Susana Costa |
| Heart Failure Nucleus of the Portuguese Society of Internal Medicine |
| Paulo Bettencourt (coordinator) |
| César Lourenço |
| Inês Araújo |
| Irene Marques |
| Joana Pimenta |
| Jorge Mercier |
| Pedro Morais Sarmento |
| Nursing Nucleus of the Portuguese Society of Cardiology |
| Manuel Belo Costa (coordinator) |
| Madalena Carvalho |
| Susana Quintão |
| Marisa Serrano |
| Ana Catarina Bastos |
| College of General Practitioners of the Portuguese Medical Council |
| José Maria da Silva Henriques (President) |
| Anabela Pimentel Lopes Cunha Vaz |
| Ângela Maria de Oliveira Teixeira |
| António Nelson Gomes Rodrigues |
| Lénia Isabel de Gouveia Olim |
| Maria de Lourdes Sousa Tavares Da Silva |
| Maria Luciana Gomes Domingues Couto Carvalho |
| Maria Pacheu Catanho Patrício |
| Noélia Rubina Correia Sousa Costa |
| Pedro Camilo de Araújo Lima de Vasconcelos |
| Cardiovascular Disease Nucleus of the Portuguese Association of General Practitioners |
| Maria Helena Febra (coordinator) |
| Maria Teressa Libório |
| Maria Helena Oliveira |
| Carolina Resende |
| Paula Oliveira |
Please cite this article as: Fonseca C, Brito D, Cernadas R, Ferreira J, Franco F, Rodrigues T, et al. Pela melhoria do tratamento da insuficiência cardíaca em Portugal – documento de consenso 2017;36:1–8.