The aim of this study was to identify pulmonary dysfunction and factors associated with prolonged mechanical ventilation, hospital stay, weaning failure and mortality in patients undergoing coronary artery bypass grafting with use of intra-aortic balloon pump (IABP).
MethodsThis observational study analyzed respiratory, surgical, clinical and demographic variables and related them to outcomes.
ResultsWe analyzed 39 patients with a mean age of 61.2 years. Pulmonary dysfunction, characterized by mildly impaired gas exchange, was present from the immediate postoperative period to the third postoperative day. Mechanical ventilation time was influenced by the use of IABP and PaO2/FiO2, female gender and smoking. Intensive care unit (ICU) stay was influenced by APACHE II score and use of IABP. Mortality was strongly influenced by APACHE II score, followed by weaning failure.
ConclusionPulmonary dysfunction was present from the first to the third postoperative day. Mechanical ventilation time was influenced by female gender, smoking, duration of IABP use and PaO2/FiO2 on the first postoperative day. ICU stay was influenced by APACHE II score and duration of IABP. Mortality was influenced by APACHE II score, followed by weaning failure.
O objetivo deste estudo foi identificar a disfunção pulmonar e fatores relacionados ao tempo de ventilação mecânica e internação, insucesso da extubação e mortalidade em pacientes submetidos à cirurgia de revascularização de miocárdio, com uso de balão intra-aórtico.
MétodoEstudo observacional, no qual foram analisadas variáveis respiratórias, clínico-demográficas e cirúrgicas que, posteriormente, foram relacionadas com os desfechos.
ResultadosForam avaliados 39 pacientes, com idade média 61,2 anos. A disfunção pulmonar esteve presente do pós operatório imediato (POI) ao PO3, caracterizada por DTTG de grau leve. A ventilação mecânica apresentou influência do tempo de uso do balão intra-aórtico, PaO2/FiO2, sexo feminino e o tabagismo. A internação na UTI foi influenciada pelo APACHE II e uso de balão intra-aórtico. O óbito apresentou influência do APACHE II, seguido do insucesso da extubação.
ConclusãoA disfunção pulmonar esteve presente do POI até o PO3. O tempo de VM foi influenciado pelo sexo feminino, tabagismo, tempo BIA e PaO2/FiO2 no POI. O tempo de internação foi influenciado pelo APACHE II e uso do balão intra-aórtico. A mortalidade foi influenciada pelo APACHE II, seguido do insucesso de desmame.
Acute Physiology and Chronic Health Evaluation
body mass index
coronary artery bypass grafting
cardiac output
cardiopulmonary bypass
European System for Cardiac Operative Risk Evaluation
fraction of inspired oxygen
intra-aortic balloon pump
left ventricular ejection fraction
mechanical ventilation
partial pressure of carbon dioxide
partial pressure of oxygen
positive end-expiratory pressure
tidal volume
Even with technological advances and modern techniques, pulmonary function is still often impaired following cardiac surgery, and patients undergoing such procedures are more likely to develop pulmonary complications.1
In addition to the use of cardiopulmonary bypass (CPB), pulmonary dysfunction may be secondary to induction of anesthesia, surgical trauma,2–4 and factors present before surgery, such as age and smoking.3,4 About 20% of patients who develop pulmonary dysfunction require ventilatory support for more than 48 hours.5
Perioperative factors such as advanced age, female gender, low left ventricular ejection fraction (LVEF), low cardiac output (CO) syndrome, prolonged CPB time, and use of intra-aortic balloon pump (IABP) may delay weaning.6–8 Prolonged mechanical ventilation (MV) time is associated with longer stay in the intensive care unit (ICU) and higher mortality.9
The aim of this study was to identify respiratory dysfunction and perioperative factors associated with prolonged MV time, ICU stay, weaning failure and in-hospital mortality in patients undergoing elective coronary artery bypass grafting (CABG), with or without left ventricular reconstruction, using IABP in the peri- and postoperative period.
MethodsThis was an observational study of patients undergoing CABG and admitted to the ICU of the University Hospital of Campinas State University (UNICAMP), São Paulo, Brazil. The study was approved by the institutional research ethics committee of the School of Medical Sciences of UNICAMP, approval no. 296/2008.
All patients who underwent elective CABG between April 2008 and November 2012, with or without left ventricular reconstruction (LVR) and using an IABP, were included. In all cases the IABP was placed immediately after induction of anesthesia and remained in place after weaning from CPB.
Clinical and demographic information including age, gender, body mass index (BMI), smoking, presence of chronic obstructive pulmonary disease (COPD), diabetes or hypertension, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, EuroSCORE (European System for Cardiac Operative Risk Evaluation) II score, preoperative echocardiographic parameters including LVEF, type of surgery, duration of CBP, duration of MV and ICU stay, weaning failure and hospital mortality, and respiratory variables including oxygenation index (partial pressure of oxygen/fraction of inspired oxygen [PaO2/FiO2]) and partial pressure of carbon dioxide (PaCO2), were collected from the immediate post-operative period until the third postoperative day.
After admission to the ICU, all patients received ventilatory assistance using RAPHAEL (Hamilton Medical®, Switzerland) or Evita 4 Dura (Dräger®, Germany) mechanical ventilators with the following parameters: synchronized intermittent mandatory ventilation mode; respiratory rate (RR) 12 breaths per min; tidal volume (Vt) 6-8 ml/kg; FiO2 0.6; positive end-expiratory pressure (PEEP) 5 cmH2O and pressure support ventilation (PSV) 20 cmH2O.
Ventilatory support was withdrawn by direct extubation when the following minimum clinical and respiratory function parameters were achieved: Glasgow Coma Scale >10; hemoglobin >9 g/dl; absence of fluid, electrolyte or acid/base abnormalities; dopamine or dobutamine levels <5 μg/kg/min or noradrenaline <0.5 μg/kg/min; PSV mode; spontaneous RR between 10 and 20 breaths per min; spontaneous Vt ≥5 ml/kg; FiO2 0.4; PEEP 5 cmH2O and PSV 10 cmH2O; PaO2/FiO2 >200; and rapid shallow breathing index (calculated as RR/Vt) <105.10 Blood gas analysis was performed with an ABL 700® analyzer (Radiometer, Denmark).
The study investigators monitored patients’ respiratory function parameters and the need to return to MV.
Weaning failure was defined as the need for reintubation within 48 hours of extubation, using the following criteria: tachypnea for >35 s, apnea for >45 s, oxygen saturation <90%, heart rate >120 beats per min (or >20% change from baseline), agitation, sweating, low level of consciousness, paradoxical breathing, hemodynamic instability (systolic blood pressure >180 mmHg or <90 mmHg), or use of accessory muscles.
Statistical analysisA descriptive analysis was performed with frequency tables for categorical variables and measures of location and dispersion for numerical variables.
SAS for Windows release 9.2 (SAS Institute Inc., 2002-2008, Cary, NC, USA) was used for the statistical analysis. Repeated measures analysis of variance (ANOVA) with rank transformation was used to compare respiratory function parameters over time. Simple and multiple linear regression was used to identify factors associated with the outcomes of MV time and ICU stay, while Cox univariate and multivariate regression analysis was used to identify factors associated with weaning success and mortality. Variables were selected by a stepwise process. The level of significance adopted was 5%.
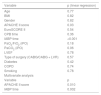
ResultsThe sample consisted of 39 patients with a mean age of 62±11.5 years, predominantly male (64.1%), who underwent elective CABG with or without LVR and using an IABP from induction of anesthesia to the postoperative period. Table 1 shows the clinical, demographic and surgical characteristics of the study population, while Table 2 shows the variables analyzed in the postoperative period.
Clinical, demographic and surgical characteristics of the study population.
| Gender | |
| Female | 14/39 (35.9%) |
| Male | 25/39 (64.1%) |
| Age (years) | 61.2±11.5 |
| BMI (kg/m2) | 25.9±4.1 |
| APACHE II score | 14.2±4 |
| APACHE II mortality score | 21±10.2 |
| EuroSCORE II | 18.5±17.6 |
| Smoking | |
| Yes | 15/39 (38.46%) |
| No | 24/39 (61.54%) |
| COPD | |
| Yes | 7/39 (17.95%) |
| No | 32/39 (82.05%) |
| Hypertension | 39 (100%) |
| Diabetes | |
| Yes | 20/39 (51.28%) |
| No | 19/39 (48.72%) |
| CPB time (min) | 94.7±32.6 |
| Type of surgery | |
| CABG | 19/39 (48.72%) |
| CABG + LVR | 20/39 (51.28%) |
| LVEF (%) | 39.5±11.36 |
| IABP time (days) | 4.46±2.17 |
| Isolated CABG without CPB | 1/39 (0.4%) |
APACHE II: Acute Physiology and Chronic Health Evaluation II; BMI: body mass index; CABG: coronary artery bypass grafting; COPD: chronic obstructive pulmonary disease; CPB: cardiopulmonary bypass; EuroSCORE: European System for Cardiac Operative Risk Evaluation; IABP: intra-aortic balloon pump; LVR: left ventricular reconstruction.
Postoperative variables.
| Weaning on PO1 | |
| Yes | 24/39 (61.54%) |
| No | 15/39 (38.46%) |
| MV time (hours) | 94.4±314.9 |
| ICU stay (days) | 15.1±16.2 |
| Weaning failure | |
| Yes | 18/39 (46.15%) |
| No | 21/39 (53.85%) |
| Died | |
| Yes | 19/39 (48.72%) |
| No | 20/39 (51.28%) |
ICU: intensive care unit; MV: mechanical ventilation; PO1: first postoperative day.
ANOVA was used for descriptive analysis and comparison of the respiratory parameters PaO2/FiO2 and PaCO2, and showed no statistically significant differences between the immediate postoperative period and the third postoperative day (Table 3).
Comparison of respiratory parameters over time.
| Variable | PaO2/FiO2 (mmHg) | PaCO2 (mmHg) |
|---|---|---|
| iPO | 220.6±68.2 | 37.6±4.3 |
| PO1 | 214.4±58.2 | 38.4±5.7 |
| PO2 | 211.8±83.1 | 38.8±5.5 |
| PO3 | 221±77.4 | 37.4±6.2 |
| p | 0.89 | 0.81 |
FiO2: fraction of inspired oxygen; iPO: immediate postoperative period; PaCO2: partial pressure of carbon dioxide; PaO2: partial pressure of oxygen; PaO2/FiO2: oxygenation index; PO1: first postoperative day; PO2: second postoperative day; PO3: third postoperative day.
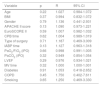
Univariate linear regression analysis shows that the variables that correlated significantly with MV time were use of IABP and PaO2/FiO2 in the immediate postoperative period, longer IABP duration and lower immediate postoperative PaO2/FiO2 being associated with longer MV (Table 4). In multivariate linear regression analysis the variables associated with MV duration were gender, smoking, duration of IABP use, PaO2/FiO2 in the immediate postoperative period and EuroSCORE.
Univariate and multivariate linear regression analysis to identify variables influencing mechanical ventilation time.
| Variable | p (linear regression) |
|---|---|
| Age | 0.45 |
| BMI | 0.84 |
| Gender | 0.12 |
| APACHE II score | 0.36 |
| EuroSCORE II | 0.11 |
| CPB time | 0.42 |
| IABP time | 0.03 |
| PaO2/FiO2 (iPO) | 0.01 |
| PaCO2 (iPO) | 0.14 |
| LVEF | 0.37 |
| Type of surgery (CABG/CABG + LVR) | 0.98 |
| Diabetes | 0.13 |
| COPD | 0.12 |
| Smoking | 0.10 |
| Multivariate analysis | |
| Variable | p |
| Gender | 0.0036 |
| Smoking | 0.002 |
| IABP time | 0.023 |
| PaO2/FiO2 (iPO) | <0.001 |
| EuroSCORE | 0.028 |
APACHE II: Acute Physiology and Chronic Health Evaluation II; BMI: body mass index; CABG: coronary artery bypass grafting; COPD: chronic obstructive pulmonary disease; CPB: cardiopulmonary bypass; EuroSCORE: European System for Cardiac Operative Risk Evaluation; FiO2: fraction of inspired oxygen; IABP: intra-aortic balloon pump; iPO: immediate postoperative period; LVEF: left ventricular ejection fraction; LVR: left ventricular reconstruction; PaCO2: partial pressure of carbon dioxide; PaO2: partial pressure of oxygen; PaO2/FiO2: oxygenation index.
Of the variables influencing duration of ICU stay, higher APACHE II score and longer IABP use were associated with longer ICU stay (Table 5).
Univariate and multivariate linear regression analysis to identify variables influencing duration of intensive care unit stay.
| Variable | p (linear regression) |
|---|---|
| Age | 0.77 |
| BMI | 0.82 |
| Gender | 0.82 |
| APACHE II score | 0.03 |
| EuroSCORE II | 0.54 |
| CPB time | 0.36 |
| IABP time | <0.001 |
| PaO2/FiO2 (iPO) | 0.18 |
| PaCO2 (iPO) | 0.06 |
| LVEF | 0.78 |
| Type of surgery (CABG/CABG + LVR) | 0.57 |
| Diabetes | 0.42 |
| COPD | 0.74 |
| Smoking | 0.78 |
| Multivariate analysis | |
| Variable | p |
| APACHE II score | 0.010 |
| IABP time | 0.002 |
APACHE II: Acute Physiology and Chronic Health Evaluation II; BMI: body mass index; CABG: coronary artery bypass grafting; COPD: chronic obstructive pulmonary disease; CPB: cardiopulmonary bypass; EuroSCORE: European System for Cardiac Operative Risk Evaluation; FiO2: fraction of inspired oxygen; IABP: intra-aortic balloon pump; iPO: immediate postoperative period; LVEF: left ventricular ejection fraction; LVR: left ventricular reconstruction; PaCO2: partial pressure of carbon dioxide; PaO2: partial pressure of oxygen; PaO2/FiO2: oxygenation index.
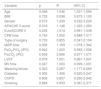
Table 6 presents the results of analysis of variables that could be associated with weaning failure, which shows that none of the variables analyzed had a significant influence.
Univariate and multivariate linear regression analysis to identify variables influencing weaning failure.
| Variable | p | R | 95% CI |
|---|---|---|---|
| Age | 0.22 | 1.027 | 0.984-1.072 |
| BMI | 0.37 | 0.994 | 0.832-1.072 |
| Gender | 0.79 | 1.136 | 0.441-2.931 |
| APACHE II score | 0.13 | 1.090 | 0.973-1.221 |
| EuroSCORE II | 0.59 | 1.007 | 0.982-1.032 |
| CPB time | 0.62 | 1.004 | 0.989-1.019 |
| Type of surgery | 0.71 | 1.187 | 0.469-3.009 |
| IABP time | 0.13 | 1.127 | 0.963-1.318 |
| PaO2/FiO2 (iPO) | 0.66 | 0.998 | 0.991-1.005 |
| PaCO2 (iPO) | 0.32 | 0.949 | 0.854-1.054 |
| LVEF | 0.29 | 0.976 | 0.934-1.021 |
| MV time | 0.32 | 1.000 | 1.000-1.001 |
| Diabetes | 0.91 | 1.053 | 0.418-2.652 |
| COPD | 0.45 | 1.750 | 0.402-7.611 |
| Smoking | 0.65 | 1.250 | 0.469-3.330 |
APACHE II: Acute Physiology and Chronic Health Evaluation II; BMI: body mass index; CABG: coronary artery bypass grafting; CI: confidence interval; COPD: chronic obstructive pulmonary disease; CPB: cardiopulmonary bypass; EuroSCORE: European System for Cardiac Operative Risk Evaluation; FiO2: fraction of inspired oxygen; IABP: intra-aortic balloon pump; iPO: immediate postoperative period; LVEF: left ventricular ejection fraction; LVR: left ventricular reconstruction; PaCO2: partial pressure of carbon dioxide; PaO2: partial pressure of oxygen; PaO2/FiO2: oxygenation index.
It can be seen in Table 7 that age, APACHE II score, duration of IABP use and weaning failure were associated with increased mortality in the study population.
Cox regression analysis to identify variables influencing mortality.
| Variable | p | R | 95% CI |
|---|---|---|---|
| Age | 0.046 | 1.046 | 1.001-1.094 |
| BMI | 0.733 | 0.098 | 0.873-1.100 |
| Gender | 0.573 | 1.299 | 0.522-3.229 |
| APACHE II score | 0.018 | 1.146 | 1.023-1.283 |
| EuroSCORE II | 0.238 | 1.014 | 0.991-1.038 |
| CPB time | 0.740 | 1.002 | 0.988-1.017 |
| Type of surgery | 0.733 | 0.855 | 0.347-2.104 |
| IABP time | 0.026 | 1.169 | 1.018-1.342 |
| PaO2/FiO2 (iPO) | 0.942 | 1.000 | 0.993-1.006 |
| PaCO2 (iPO) | 0.509 | 0.966 | 0.871-1.071 |
| LVEF | 0.979 | 1.001 | 0.961-1.041 |
| MV time | 0.347 | 1.000 | 0.999-1.001 |
| Weaning failure | 0.023 | 3.267 | 1.177-9.069 |
| Diabetes | 0.565 | 1.306 | 0.525-3.247 |
| COPD | 0.806 | 0.857 | 0.250-2.942 |
| Smoking | 0.884 | 0.933 | 0.367-2.371 |
APACHE II: Acute Physiology and Chronic Health Evaluation II; BMI: body mass index; CABG: coronary artery bypass grafting; CI: confidence interval; COPD: chronic obstructive pulmonary disease; CPB: cardiopulmonary bypass; EuroSCORE: European System for Cardiac Operative Risk Evaluation; FiO2: fraction of inspired oxygen; IABP: intra-aortic balloon pump; iPO: immediate postoperative period; LVEF: left ventricular ejection fraction; LVR: left ventricular reconstruction; PaCO2: partial pressure of carbon dioxide; PaO2: partial pressure of oxygen; PaO2/FiO2: oxygenation index.
Most of the study population were male and aged under 65 years. This is in agreement with the literature which shows that ischemic heart disease is more prevalent in individuals aged under 65 years and of male gender, both in Brazil10 and in developed countries.11
Surgery, most often CABG,12 is a common intervention in the modern treatment of heart disease. As CABG is increasingly indicated for older patients with more comorbidities, complications are also becoming more frequent, particularly those related to low CO.13 Among the causes of low CO syndrome is left ventricular dysfunction (LVEF <50%),14–17 and in such cases the use of an IABP is indicated. This is the most frequently used circulatory assist device in various types of cardiac surgery, increasing CO by enhancing myocardial perfusion and reducing left ventricular afterload.16
In our study population (n=39), 19 patients (48.72%) underwent CABG and 20 (51.28%) underwent CABG associated with LVR. In a recent study of different types of cardiac surgery in which an IABP was used, 37.5% were CABG and 5% were CABG associated with left ventricular aneurysm repair.16
Randomized trials and cohort studies have associated preoperative IABP placement with better outcomes in high-risk patients undergoing CABG. The definition of high risk varies between these studies, including advanced age, low LVEF, symptomatic heart failure, left main disease, redo CABG, and urgent or emergent surgery.14
Regarding comorbidities in our study population, all patients were hypertensive, 15 (38.46%) were smokers, 7 (18%) had been diagnosed with COPD and 20 (51.28%) had type 2 diabetes. In a 1998 study of patients requiring IABP following cardiac surgery, 18.8% were smokers and 31.8% were diabetic.15
Recent studies have concluded that smoking does not affect early mortality following CABG but is associated with increased incidence of complications such as pneumonia and multiple organ failure, as well as with worse long-term survival.16
The proportion of patients with COPD following CABG varies. This condition is often considered a risk factor for morbidity and mortality and is associated with respiratory infections, mediastinitis and need for prolonged MV. Manganas et al.18 analyzed postoperative outcomes in patients undergoing CABG and divided them into three groups according to results of spirometry: controls (normal spirometry), mild to moderate COPD, and severe COPD. They found no association between the presence or severity of COPD and mortality, but the incidence of respiratory infections and prolonged hospital stay was significantly higher in patients with severe COPD.19
Diabetes is a common comorbidity in cases of coronary artery disease, but its reported incidence in patients undergoing CABG is variable. It has been described as a risk factor for in-hospital mortality20 and prolonged hospital stay.10
The APACHE II score is used to classify the clinical severity of ICU patients.21 The mean APACHE II score of patients in the present study was 14±4, and predicted mortality score was 21±10.2. Similar results were found by Rodrigues et al., with a mean APACHE II score of 12.8±4.2 and predicted mortality of 17.9±9.5, which correlated with the occurrence of severely impaired gas exchange (p=0.0001) and confirmed the ability of APACHE II to evaluate the severity of patients following cardiac surgery.22 Kellner et al. confirmed this ability in a comparison of scoring systems including APACHE II for predicting mortality, including in patients treated with IABP.21
The EuroSCORE was developed on the basis of data from 130 centers in eight European countries in order to predict morality in patients undergoing cardiac surgery (valve surgery as well as CABG). EuroSCORE II classifies patients as having very high risk of mortality with values between 4.14% and 47.60%.23 The mean EuroSCORE II in our study was 18.5%, which according to the literature makes our population a high-risk one. This high score may be related to left ventricular dysfunction, elevated creatinine, or other preoperative factors, as indicated in other studies.23
Nineteen (48.72%) of our patients underwent CABG and 20 (51.28%) underwent CABG combined with LVR. In another Brazilian study of patients treated with IABP intraoperatively and postoperatively, 37.5% underwent CABG and 5% underwent CABG associated with LVR,16 while in an older study with postoperative use of IABP, 54.3% underwent CABG and 6.6% CABG associated with LVR.15
Mean duration of CPB in the present study was 94.7 min, a similar figure to that of a study by Nozawa et al.6 in which IABP was not used, but shorter than in another study by Nozawa's group7 in which IABP was used during and after cardiac surgery, in which CPB time ranged between 127.5 and 140 min. These studies indicate that prolonged CPB time (>120 min) is associated with higher surgical risk.
Pulmonary dysfunctionPostoperative pulmonary dysfunction may occur in most patients undergoing cardiac surgery. Its etiology is multifactorial, but it results mainly from the association of anesthesia, MV, surgical trauma and CPB.
In the present study, the respiratory parameters PaO2/FiO2 and PaCO2 did not change significantly over time, with mean PaO2/FiO2 rising from 211 to 221 from the first to the third postoperative day, suggesting the presence of mildly impaired gas exchange. PaCO2 changed from 37.4 to 38.8 mmHg from the first to the third postoperative day, showing that ventilatory parameters remained within normal values.
The criteria for a diagnosis of acute respiratory distress syndrome (ARDS), reflecting impaired gas exchange, have recently changed and are now based on the degree of hypoxemia. Mild ARDS is defined as PaO2/FiO2 of >200 and ≤300 mmHg, moderate ARDS as PaO2/FiO2 of >100 and ≤200 mmHg, and severe ARDS as PaO2/FiO2 of ≤100 mmHg, together with four ancillary factors for severe ARDS: refractory hypoxemia, radiographic severity, respiratory system compliance, and positive end-expiratory pressure.24
This syndrome may be present following CABG due to anesthesia, which reduces functional residual capacity and leads to atelectasis of dependent lung regions and alterations in diaphragm movement. In addition, CPB, surgical trauma, heparin-protamine complexes, and lung damage arising from MV can contribute to the development of impaired gas exchange and hence of ARDS.24
Hemodynamic instability in the peri- and postoperative period may also be a factor in the development of ARDS in CABG patients, especially when associated with low LVEF. Left ventricular dysfunction, particularly reduced left ventricular compliance, raises end-diastolic pressure, which is transmitted retrogradely to the pulmonary venous microcirculation, increasing hydrostatic pressure and leading to extravasation of liquid into the alveolar space,25 impairing gas exchange and increasing the likelihood of ARDS.
In such cases, the positive pressure provided by MV improves pulmonary compliance due to recruitment of collapsed alveoli, reducing hypoxemia as well as ventricular pre- and afterload and increasing CO.26 These benefits could result in greater dependence on MV in these patients.
Duration of mechanical ventilationThe mean MV time in the present study was 94.4 hours, longer than in studies of patients undergoing elective CABG without IABP.27 Predictors of longer MV time in the present study were female gender, high EuroSCORE, longer IABP time, lower PaO2/FiO2 in the immediate postoperative period, and smoking.
The best time for weaning from MV following CABG with use of IABP is still the subject of debate, but it is agreed that complications of MV such as atelectasis, barotrauma and pneumonia are directly related to duration of endotracheal intubation and ventilatory support and that following CABG, patients should therefore be weaned as early as possible.10 Previous studies have shown that patients weaned within six hours of ICU admission have shorter total length of stay, reducing costs and use of hospital and ICU resources.27
Liu et al., comparing MV combined with IABP and IABP alone, found higher rates of pulmonary infection and renal insufficiency in the IABP + MV group. However, pulmonary infection and renal insufficiency were risk factors for all-cause in-hospital mortality in both groups.28
Weaning failureThe rate of weaning failure in the present study was 46%, and none of the variables analyzed significantly affected this outcome. By contrast, Suematsu et al.29 found that advanced age (>70 years) and heart failure were associated with prolonged MV, while according to Nozawa et al.,6,7 LVEF <50% contributed to weaning failure. Similarly, Cislaghi et al.30 showed that LVEF <30%, CPB time over 91 min and age over 80 years were associated with delayed weaning.
In a study of CABG patients, congestive heart failure, low preoperative PaO2 and postoperative anemia were found to be independent risk factors for MV dependence.30
Duration of intensive care unit stayAs a result of advances in surgical and intensive care management, high-risk patients, previously contraindicated for cardiac surgery, are now being referred fro such procedures, resulting in a higher proportion of patients with prolonged ICU stay. In the present study, mean ICU stay was 15.1 days, well above the figures in previous studies on cardiac surgery patients (4.2 days in two Brazilian studies and 7.87 in an international study in which the mean ICU stay was less than three days.10,31 In our study, APACHE II score, IABP time and MV time were positively correlated with ICU stay in univariate analysis, and in multivariate analysis only APACHE II and IABP time were risk factors for longer ICU stay.
Laizo et al.10 identified COPD, pulmonary congestion, delayed weaning from MV, diabetes, infection, renal insufficiency, stroke and hemodynamic instability as complications that increased ICU stay after cardiac surgery, while Tekumit et al.32 identified low CO syndrome and respiratory failure as the main causes of prolonged ICU stay.
In-hospital mortalityIn the present study, the factors that strongly influenced in-hospital mortality were APACHE II score and weaning failure, the latter increasing risk of death three-fold. This is in agreement with previous studies that reported increased morbidity, especially respiratory infections resulting from reintubation, after weaning failure.6,7
Nineteen (48.72%) of our 39 patients died in the ICU. Mortality in the study by Tekumit et al.32 was 38.7% (n=137); these authors also reported that weaning failure was an important factor in this outcome, as well as diabetes, postoperative renal dysfunction, postoperative use of IABP and prolonged MV. Further corroboration is provided by Pivatto Júnior et al.,16 who observed 53.8% in-hospital mortality in patients requiring IABP. According to these authors, these patients are at very high risk for morbidity and mortality, and mortality in this group ranges from 21% to 73%. These rates have remained relatively stable over the past 10 years, despite improvements in surgical techniques, better myocardial protection and other technological advances; this is largely due to the increasing age of patients undergoing surgery, the frequency of reoperation and emergent procedures, and the worsening clinical status of those referred for surgery. Complications associated with IABP use are common, with a reported incidence of 8-18%, and mortality directly related to the device of 0-2.6%.16 Kellner et al. also found a high mortality rate of 44% in patients with myocardial infarction complicated by cardiogenic shock; 34% of these individuals were treated with IABP.21
The mean LVEF in the present study was 39.5%. In the study by Pivatto Júnior et al.16 of patients receiving IABP following cardiac surgery, 35% had LVEF of 30-50% and in 6% it was less than 30%. Although LVEF was not a risk factor for in-hospital mortality in our study, Oliveira et al.33 observed increased in-hospital mortality in patients undergoing CABG with LVEF <50%, as did O’Connor et al.,34 in patients with LVEF <40% compared to those with LVEF >60%. Moderate to severe left ventricular dysfunction (LVEF >30%) is a common finding in cardiac surgery patients in general, and those with low LVEF are at high risk for postoperative complications and mortality.35
ConclusionThe results of the present study show that pulmonary dysfunction, characterized by mildly impaired gas exchange, was present from the immediate postoperative period to the third postoperative day.
The variables that influenced MV time were duration of IABP use and PaO2/FiO2 on the first postoperative day, and in multivariate analysis the same parameters remained, together with female gender, EuroSCORE and smoking.
Length of ICU stay was influenced by APACHE II score and duration of IABP. Mortality was influenced by age, APACHE II score, duration of IABP use, and weaning failure.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Amaral Gonçalves Fusatto H, Castilho de Figueiredo L, Ragonete dos Anjos Agostini AP, Sibinelli M, Dragosavac D. Fatores associados à disfunção pulmonar em pacientes revascularizados e com uso de balão. Rev Port Cardiol. 2018;37:15–23.