In spite of high prevalences of hypertension and hypercholesterolemia, the majority of elderly patients admitted for aortic valve surgery due to calcific aortic valve disease (CAVD) do not have significant coronary artery disease (CAD).
ObjectiveTo evaluate the lipid profile (LP) of patients undergoing surgery for CAVD and to correlate this with coronary angiographic data and prior cardiovascular risk factor profile.
MethodsThis was a prospective observational cohort study of 264 consecutive patients aged >59 years (mean 72), 126 men (48%) and 138 women (52%). According to the angiographic presence (irregularities, moderate or significant lesions) or absence (normal angiogram) of significant CAD respectively, patients were divided into two groups: A (n=127, 48%) and B (n=137, 52%). A mean of 3.5 classical risk factors were identified in men and 2.6 in women. LP (obtained on admission, in the fasting state) included total cholesterol (TC), HDL, triglycerides (TG), LDL, and lipoprotein(a).
ResultsWith the exception of male gender, diabetes and HDL, the other factors studied – smoking, hypertension, TC, TG, LDL (in both statin-treated and non-statin-treated patients) and lipoprotein(a) – did not show significant differences between groups A and B; LDL was 116±40mg/dl in group A vs. 123±38mg/dl in group B, in non-statin-treated patients; significant CAD was identified in 64% of men vs. 26% of women (p<0.001); 43% of group A had diabetes vs. 27% of group B (p<0.01); HDL was 49±14mg/dl in group A vs. 59±16mg/dl in group B (p<0.001); HDL in group A was 49±14mg/dl in men vs. 49±13mg/dl in women (NS) and 45±13mg/dl in diabetic patients vs. 52±14mg/dl in non-diabetics (p<0.02); HDL in group B diabetic patients was 54±17mg/dl in men vs. 56±18mg/dl in women (NS), and HDL in group B non-diabetic patients was 55±13mg/dl in men vs. 63±17mg/dl in women (p<0.02). Multivariate analysis showed that only low HDL and diabetes (in women) were independent risk factors for significant CAD. The effect of male gender as a risk factor appears to be exerted mainly through lower HDL levels.
ConclusionsElevated HDL is the main negative risk factor for significant CAD in elderly high-risk but mildly dyslipidemic CAVD patients. HDL does not appear to have any protective effect in the pathophysiology of CAVD. In terms of long-term intervention, primary prevention of significant CAD should in the future be hybrid, focusing mainly on improving HDL function, but also on lowering LDL.
Apesar de apresentarem elevadas prevalências de hipertensão (HT) e hipercolesterolemia – colesterol total (CT)>190mg/dl – a maioria dos doentes (dts) idosos internados para cirurgia valvular por doença fibrocalcificante valvular aórtica (DFCVA) não tem doença coronária significativa (DCS).
ObjetivoAvaliação do perfil lipidémico (PL) de dts operados por DFCVA e sua correlação com os dados coronariográficos e o perfil de fatores de risco (FR) prévio.
Material e métodosEstudo observacional prospetivo, de coorte, de 264 dts com DFCVA, 126 homens (dts M) e 138 mulheres (dts F), com idade > 59 anos (idade média de 72), consecutivamente internados. PL: determinação (na admissão, em jejum) de CT, HDL, triglicéridos (TG), LDL e lipoproteína (a) (Lp(a)). Conforme a presença angiográfica (irregularidades, lesões moderadas ou graves) ou a ausência (coronárias normais) de DCS, os dts foram respetivamente divididos em 2 grupos (Gr): GrA (127 dts – 48% do total) e GrB (137 dts – 52%). FR clássicos (média): 3,5 nos dts M, 2,6 nos dts F.
Resultados1) Com exceção do género masculino, diabetes e HDL, os restantes fatores (tabagismo, HT, CT, TG, LDL – tanto nos dts medicados com estatina como nos dts não medicados – e Lp(a)) não permitem discriminar os dts-GrA dos dts-GrB; LDL(mg/dl)- GrA 116 ± 40 versus GrB 123 ± 38, nos dts não medicados com estatina. 2) DCS: 64 dts M versus 26% dts F (p<0,001); diabetes – 43 no GrA versus 27% no GrB (p<0,01); HDL (mg/dl) – 49 ± 14 no GrA versus 59 ± 16 no GrB (p<0,001). 3) HDL (mg/dl) no GrA – 49 ± 14 nos dts M versus 49 ± 13 nos dts F (NS); 45 ± 13 em dts diabéticos versus 52 ± 14 em dts não diabéticos (p<0,02). 4) HDL (mg/dl) no GrB-diabéticos – 54 ± 17 nos dts M versus 56 ± 18 nos dts F (NS); HDL (mg/dl) no GrB-não diabéticos – 55 ± 13 nos dts M versus 63 ± 17 nos dts F (p<0,02). 5) Análise multivariada: revelou que apenas o HDL baixo e a diabetes (nos dts F) são FR independentes para o desenvolvimento de DCS. O papel do género masculino como FR parece exercer-se fundamentalmente por via da redução dos valores de HDL.
ConclusõesUm valor alto de HDL é o principal fator protetor contra a DCS no idoso com DFCVA, com risco elevado, mas com dislipidemia ligeira/moderada. O HDL não parece desempenhar qualquer ação protetora na etiopatogénese da DFCVA. Em intervenção a longo prazo, no futuro, a prevenção primária da DCS deverá tornar-se híbrida, focando-se fundamentalmente na melhoria da função do HDL, mas em associação com a redução do LDL.
Calcific valve disease, particularly calcific aortic valve disease (CAVD), has a similar pathophysiology to atherosclerotic vascular disease.1 The initiating event of CAVD is an atherosclerotic lesion1 and its evolution has a strong inflammatory component.1,2 The main risk factors for CAVD are the same as for atherosclerotic vascular disease, particularly coronary artery disease (CAD): hypertension, dyslipidemia, diabetes, male gender, smoking and advanced age.1,3–5 However, in spite of high prevalences of hypertension and dyslipidemia, the majority of elderly patients admitted for aortic valve surgery due to CAVD do not have significant CAD.3,6 The question arises as to why individuals with multiple cardiovascular risk factors reach the age of 70 or more with no evidence of significant CAD. The current epidemic of CAVD in the elderly means that this cohort can serve as a kind of natural laboratory for the study of CAD in this population, particularly those with CAVD, on which to base an analysis of different cardiovascular risk factors.
ObjectiveThe objective of this study was to evaluate the lipid profile of patients undergoing surgery for CAVD and to correlate this with coronary angiographic data (the presence or absence of epicardial CAD) and overall cardiovascular risk factor profile. The angiographic study can be seen as a retrospective cross-sectional evaluation of the consequences for the coronary arteries of chronic, and in some cases prolonged, exposure to a range of different risk factors.
MethodsThis was an observational cohort study with prospective recruitment over a period of 17 months (February 2006–July 2007) of 264 consecutive outpatients with CAVD, aged >59 years, referred for surgery and with a recent coronary angiogram. They included 126 men and 138 women, with a mean age of 72±6 years (72±6 in men and 73±6 in women).
CAVD was asymptomatic in 7% of the patients.
Classical risk factors were considered to be age (>59 years), male gender, smoking (active smoker or ex-smoker who quit less than 12 years previously), diabetes, hypertension and hypercholesterolemia (previous or current evidence of total cholesterol >190mg/dl). Obesity was not considered an independent risk factor due to its multifaceted and variable etiopathogenic characteristics (it is frequently linked to dyslipidemia, hypertension and diabetes).
The patients’ lipid profile, assessed from samples obtained on admission after 12hours fasting and with the patient seated for at least 30minutes, consisted of total cholesterol, HDL cholesterol and triglycerides (by enzymatic colorimetric methods), LDL cholesterol (measured indirectly using the Friedewald formula), and lipoprotein(a) (by nephelometry). In two patients LDL cholesterol could not be determined due to extremely high triglyceride levels (>350mg/dl).
The angiographic presence of irregularities, moderate (stenosis not exceeding 50% of lumen diameter) or significant lesions (over 50% stenosis) was considered diagnostic of significant CAD, while a normal angiogram was taken to indicate absence of significant CAD, since it is highly unlikely that a patient would present only lesions with positive remodeling, i.e. significant lesions with outward expansion and preserved luminal diameter.7
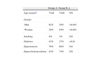
The baseline prevalences of classical risk factors in the overall population is shown in Figure 1. There were a mean of 3.5 risk factors in men (range 2–6) and 2.6 in women (range 1–5).
The patients were divided into two groups: A (with significant CAD, n=127, 48%) and B (without significant CAD, normal angiogram, n=137, 52%). CAD was considered subclinical, being an angiographic finding only, in 60% of group A.
Fifty-six percent of the patients were chronically medicated (more than 4 weeks) with lipid-lowering agents (55% with statins), corresponding to 68% of group A (mean dose 22mg/day, in the proportion of 9:3:2 for simvastatin/rosuvastatin/atorvastatin) and 42% of group B (mean dose 20mg/day, in the proportion of 8:2:1 for simvastatin/rosuvastatin/atorvastatin).
The lipid profile obtained on admission was taken to represent the patient's long-term lipid status and considered relatively stable, at least in terms of HDL cholesterol, although it should be borne in mind that statin therapy will have led to changes over recent months or years in a significant number of patients. Possible seasonal variations in lipid parameters8 were not considered to have a significant effect on the overall results, since they would have affected patients with and without CAD, and the study period was nearly 18 months. The influence of medication, particularly on HDL cholesterol due to the action of beta-blockers and benzodiazepines,8 was considered negligible, since the few patients taking these drugs were distributed evenly between groups A and B.
Statistical analysisThe Student's t test (for unpaired samples) was used for quantitative variables and the chi-square test with Yates’ correction for qualitative variables. Multivariate logistic regression analysis was performed using SPSS version 15.0. A p value of ≤0.05 was considered statistically significant.
ResultsFigure 1 shows the clinical characteristics of the overall population. The slight predominance of women (52%) and the high prevalences of diabetes (more than a third of patients), hypertension (over 70%) and hypercholesterolemia (over three-quarters) should be noted.
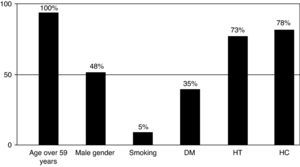
Table 1 presents the differences between groups A and B in terms of prevalence of risk factors. The association between significant CAD and CAVD was significantly more frequent in male (p<0.001) and diabetic patients (p<0.01). Smoking (with a low prevalence in this elderly population) and hypercholesterolemia were more common in patients with significant CAD, but without reaching statistical significance. There was no significant difference in age between the two groups.
Coronary artery disease and prevalence of risk factors.
| Group A | Group B | p | |
| Age (years)a | 73±6 | 72±6 | NS |
| Gender | |||
| Men | 62% | 38% | <0.001 |
| Women | 36% | 64% | <0.001 |
| Smoking | 9% | 3% | NS |
| Diabetes | 43% | 27% | <0.01 |
| Hypertension | 76% | 69% | NS |
| Hypercholesterolemia | 83% | 74% | NS |
Table 2 shows lipid profile compared between groups A and B. There were no differences with regard to LDL cholesterol in either statin-treated or non-statin-treated individuals. However, HDL cholesterol was significantly lower (p<0.001) in patients with significant CAD (49±19mg/dl vs. 59±16mg/dl). Since low-dose statins (with the exception of rosuvastatin, which was infrequently prescribed) have little or no effect on HDL cholesterol, this was not assessed separately in statin-treated and non-statin-treated individuals. There were no differences between the groups in terms of total cholesterol or triglycerides, while levels of lipoprotein(a) were slightly higher in group A (mean 45±41mg/dl vs. 36±34mg/dl in group B), with 52% of patients exceeding 30mg/dl vs. 40% in group B, but the differences were not significant.
Coronary artery disease and lipid profile.
| Group A | Group B | p | |
| Total cholesterol | 186±47 | 195±43 | NS |
| LDL cholesterol | |||
| Statin-treated | 110±44 | 98±31 | NS |
| Non-statin-treated | 116±40 | 123±38 | NS |
| HDL cholesterol | 49±14 | 59±16 | <0.001 |
| Triglycerides | 134±73 | 112±60 | NS |
| Lipoprotein(a) | 45±41 | 36±34 | NS |
Values in mg/dl (mean±standard deviation). Group A: patients with significant coronary artery disease; Group B: patients without coronary lesions.
Multivariate analysis of variables that univariate analysis revealed to be risk factors for the development of significant CAD in patients with CAVD – male gender, diabetes and low HDL – strongly suggests that only diabetes and low HDL are independent risk factors. The influence of male gender appears to be explained mainly by lower HDL levels in men. Tables 3–6 present various aspects of the relationship between gender, HDL and diabetes and the presence or absence of significant CAD in patients with CAVD. Diabetes was significantly associated with CAD (p<0.05) in women, with a more than 70% increase in risk (Table 3). In individuals with normal angiogram, women had significantly higher HDL than men (p<0.02), but the presence of diabetes reduced this difference (Table 4). Among those with significant CAD, HDL levels were significantly lower than in those without CAD but with no difference between the sexes. Diabetic patients with CAD had even lower HDL levels, the difference compared to non-diabetics being statistically significant (Table 4). Of diabetic patients with CAVD, 40% had angiographically normal coronaries and relatively high HDL levels (Table 5).
HDL cholesterol profile: comparison between patients with and without coronary artery disease.
| Group A | Group B | p | |
| Overall population | 49±14 | 59±16 | <0.001 |
| Men | 49±14 | 55±14 | <0.05 |
| Women | 49±13 | 61±17 | <0.001 |
| Diabetic | 45±13 | 55±17 | <0.01 |
| Non-diabetic | 52±14 | 59±18 | <0.01 |
Values in mg/dl (mean±standard deviation). Group A: patients with significant coronary artery disease; Group B: patients without coronary lesions.
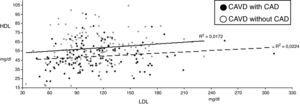
The linear association between LDL and HDL cholesterol is weak (r=0.126, p=0.04). There was no significant negative correlation between LDL and HDL, either in group A (r=0.150, p=0.10) or in group B (r=0.131, p=0.14) (Figure 2).
DiscussionAlthough male gender is a risk factor for CAVD, with a 2:1 ratio of men to women being reported in series of patients with symptomatic aortic stenosis,9,10 in populations aged >70 this difference tends to disappear, and actually reverses in patients aged over 75.11,12 Our study population – mean age 72 years, most with symptomatic CAVD and with slightly more women (52% vs. 48%) – is thus close to the expected profile. Women's longer life expectancy, which gives more time for CAVD to develop and means that the absolute number of elderly women is greater, has been put forward as the main reason for the reversal of the gender ratio among elderly individuals with symptomatic aortic stenosis.10,12 Thus, the age profile of our patients and the demographics of the Portuguese population (with a ratio of 1.4:1 women to men aged over 65) will tend to diminish the importance of male gender as an undeniable risk factor. The greater prevalence of severe comorbidities (particularly cardiac, cerebrovascular, respiratory and renal) in elderly men with symptomatic CAVD, and hence less likelihood that they will be referred for valve surgery, has been proposed as another reason for the predominance of women in series of older patients with CAVD. Nevertheless, although in the last two decades of the 20th century fewer than 60% and in some cases fewer than 20% of eligible elderly patients with severe CAVD underwent surgery,3 the marked reduction now seen in operative risk of isolated or combined aortic valve surgery means that a considerable number of elderly men with severe comorbidities are operated; on the other hand, a growing number of elderly Portuguese women have severe comorbidities (particularly obesity, chronic respiratory disease, musculoskeletal changes and complicated diabetes), greatly increasing the risks of valve surgery. However, despite these developments, the predominance of women in surgical series of elderly or very elderly patients with CAVD has not changed, which suggests that any bias in the selection of patients for surgery has no significant effect on gender distribution.
Two other factors appear to be more important: more rapid development of CAVD in older women, and the greater probability that it will become symptomatic. European and American studies have shown that the prevalence of CAVD in elderly women rises steeply from the age of 70, overtaking the figure for men at the age of 75–80.11,13 Age-related physiological changes in the aortic valve due to wear and tear are well known,14 and it is possible that in women they may lead to greater vulnerability to the combined effects of risk factors for CAVD. The results of our study suggest that rapid progression of CAVD may begin earlier in Portuguese women than in Finnish11 or American13 women. Furthermore, the response of the left ventricle to the pressure overload resulting from aortic stenosis leads to differences in remodeling between the sexes: in women there is a greater degree of wall hypertrophy and more resistance to dilatation, the chamber often remaining small, resulting in worse diastolic dysfunction but preserving normal or high ejection fraction.12,15 Although it has been suggested that much of the difference between the sexes in ventricular remodeling disappears when corrections are made for body surface area (smaller in women),12 greater wall thickness, higher intraventricular pressure and greater transvalvular gradients during exercise, and worse diastolic dysfunction12,15 are more likely to lead to rapid development of symptoms, particularly angina and paroxysmal manifestations of moderate left ventricular failure. Hence, as a diagnosis of symptomatic CAVD is a strong indication to refer the patient for surgery, more women are likely to be referred and sooner.
Although there are many complex reasons for the predominance of women in series of CAVD surgery, including in the present study, they do not appear to have any effect on the etiopathogenic relationships between risk factors for CAD and the development of significant CAD in patients with CAVD.
Diabetes, hypertension, smoking and hypercholesterolemia are risk factors for both CAVD and atherosclerotic CAD. However, only diabetes has a significantly higher prevalence in patients with CAD associated with CAVD. This supports the idea that diabetes is a major risk factor for CAD. Furthermore, in our study the association between diabetes and the pathophysiology of CAVD was revealed through the higher prevalence of diabetes in patients with CAD (43%, compared to around 30% in unselected populations with acute coronary syndrome16), which was not seen in those with normal angiogram, in whom its prevalence was similar to that of the general population aged over 60 in the VALSIM17 and PREVADIAB18 studies. However, the importance of diabetes as the main risk co-factor for CAVD has recently been confirmed.19
There are similarities between calcific disease of the native aortic valve and degeneration of bioprosthetic valves, particularly in aortic position.20,21 The fact that diabetes, especially when combined with the metabolic syndrome, is significantly associated with more rapid deterioration of bioprostheses21 supports the existence of a causal relation between diabetes and the pathophysiology of CAVD.
Analysis of the lipid profile of our study population shows that HDL cholesterol is the only lipid factor that distinguishes group A from group B, with significantly lower levels in the former, and frequently below 50mg/dl. With regard to LDL cholesterol, most patients had mild to moderate dyslipidemia, with values of 115–125mg/dl in non-statin-treated patients. This picture was to be expected given that a significant proportion of this elderly population came from the rural interior (Beira Interior and Alentejo regions), where smoking rates are very low and a Mediterranean diet is still prevalent, even though over 50% are obese or overweight.6 Symptomatic CAD is found in only 20% of this population, and the rate of premature CAD (with clinical manifestations before the age of 60) is extremely low (2%). In this cohort, pathological changes in the coronary arteries leading to CAD in the second half of life do not appear to be significantly affected by LDL levels. Hypertriglyceridemia (>150mg/dl) was identified in 23%, but severe hypertriglyceridemia (>200mg/dl) was rare (10%, of whom half were diabetic; 12% in group A and 8% in group B), and was not a significant risk factor for CAD. The results for lipoprotein(a), which is considered a risk factor for both CAD and CAVD, were not unexpected, with a non-significant tendency for higher values (>30mg/dl) in those with CAD, and thus lipoprotein(a) was not shown to be a decisive risk factor for CAD.
The lack of a correlation between HDL and LDL levels cannot be explained by the action of lipid-lowering therapy, taken by over half of the study population, but may in part reflect the complexity of interactions between various proatherogenic and antiatherogenic factors in a population with multiple risk factors, in whom LDL appears to have a secondary role compared to the greater importance of HDL.
The antiatherogenic and vasculoprotective role of HDL cholesterol results from various effects: promotion of reverse cholesterol transport, mediating efflux of cholesterol from macrophages and hence inhibiting the formation of foam cells; inhibition of LDL cholesterol oxidation; reduction of endothelial dysfunction; and anti-inflammatory action.22–24 HDL metabolism is regulated by a complex system of proteins and enzymes,22,23 and imbalances due to proatherogenic or vasculoprotective factors can arise at various points in the system.22,23 Furthermore, absolute HDL values measure the cholesterol content of particles that are designated as high-density lipoproteins, but these are structurally and functionally heterogeneous and consist of a variety of subclasses.24 What counts is the relative proportions of these subclasses, which are rarely quantified in laboratory tests; for example, HDL's protective effect is linked to the proportion of HDL-2, and particularly the HDL-2b fraction.22,25 From a clinical standpoint, routine laboratory quantification of HDL probably only reflects one of its functions – cholesterol transport.24 Although it is generally accepted that HDL levels are a good indicator of the efficiency of reverse cholesterol transport, the antiatherogenic role of HDL also depends heavily on the action of various proteins and lipids associated with HDL particles24; high HDL levels do not necessarily reflect a strong protective effect, nor do low levels always mean the opposite.
The heterogeneous composition of HDL in our population may be one reason for the fact that 6% of patients with CAD had HDL levels of over 70mg/dl and 7% of those with normal angiogram had levels below 40mg/dl; it may also partly explain the lack of correlation between LDL and HDL values. It should be noted that a third of those without CAD and with low HDL levels had incipient or evident cardiac cachexia (with very low HDL and low LDL); in these patients wasting disease is likely to be the main cause of low HDL.
In our study, the factors indicating that an elderly patient with CAVD was significantly likely also to have CAD were male gender, diabetes and low HDL. On multivariate analysis only low HDL and diabetes (particularly in women) were independent risk factors for CAD in patients with CAVD. The effect of male gender as a risk factor appears to be exerted mainly through lower HDL levels and hence reduced antiatherogenic potential. The fact that elderly women with angiographically normal coronaries had significantly higher HDL levels than men (20 years or more after menopause) suggests that the effect of male gender as a risk factor has a more complex genetic basis than sex hormones alone.26
The fact that diabetes was a stronger risk factor for CAD in women in our population is compatible with epidemiological data, since diabetes increases the risk for ischemic events and death from cardiac cause more in women than in men, even pre-menopause.26 The mechanisms through which CAD develops in diabetic individuals are multifactorial and complex: besides the involvement of other classical risk factors, particularly dyslipidemia, they include a series of metabolic, biochemical and structural alterations directly related to diabetes – hyperglycemia, insulin resistance, excessive production of advanced glycation end-products (AGEs), increased oxidative stress, endothelial dysfunction, chronic inflammation, fibrosis, prothrombotic states, hyperhomocysteinemia, and neurohormonal activation.27 Among other interactions, the combination of intensified LDL oxidation, due to the combined action of oxidative stress and excess AGEs, and significant reductions in HDL cholesterol, may play an important role in the formation and progression of atheromatous lesions. The finding that in our study population 40% of elderly diabetic patients with CAVD had no angiographic evidence of CAD and also had high HDL levels suggests that these patients – who were similar in terms of age and duration of diabetes to those with CAD – were protected against the development of CAD by the presence and persistence of high HDL. This apparent resistance to reduction in HDL levels in the presence of multiple metabolic changes triggered by diabetes may be genetically determined, although there may also be an environmental component.
There is an apparent paradox in the association between CAVD and CAD13: although the two diseases share the same risk factors and the initial lesions are similar, most patients with severe CAVD do not have significant CAD, and, even in regions where there is a high incidence of CAD, fewer than 50% of patients undergoing aortic valve replacement have sufficiently severe coronary lesions to justify combining myocardial revascularization in the same operation.13 Given this difference in the development of the two diseases, it has been suggested that the process common to both is not an atherosclerotic lesion but endothelial dysfunction, the subsequent evolution of which is modulated by other factors, genetic and/or environmental, with different pathological and clinical consequences.28 At the same time, various genetic factors have been identified that predispose to the development of CAVD,1 as well as a process conducive to the ectopic differentiation of bone tissue in the aortic valves of patients with CAVD, a process probably activated by a lipid pathway.1 However, in our study population, the fundamental difference between patients with and without CAD appears to result from the different behavior of HDL cholesterol. In these patients, sufficiently high HDL levels helped prevent the development of CAD, but did not affect the pathophysiological processes that, although triggered and/or modulated by the same risk factors, take place in valve structures subject to many years of wear and tear. Despite the pathophysiological similarities with CAD, for reasons that remain unclear the process of valve degeneration – which has a strong inflammatory component and appears to be induced by hypercholesterolemia1 – is not the subject of any negative modulation by HDL, which seems to be a “bystander”, even in individuals with high plasma HDL levels. Preliminary clinical trials with statins in patients with CAVD have shown that sufficiently large reductions in LDL cholesterol in individuals in whom aortic valve calcification is not too advanced slow the progression of aortic stenosis.1 The growing evidence for the role of dyslipidemia in the pathophysiology of CAVD makes the apparent lack of involvement of HDL in this process even stranger, especially as oxidized LDL has been found in the aortic valves of patients with CAVD, those with a higher valvular oxidized LDL score presenting higher indices of valve inflammation and more rapid hemodynamic progression of aortic stenosis.29 This paradox thus needs to be thoroughly investigated. One suggestion is that macrophages involved in the aortic valve inflammatory process, which appear to have a different cellular origin from those found in vascular atherosclerosis,30 present differences or abnormalities with regard to the cell transporters ABCA1 and/or ABCG1, which would hinder reverse cholesterol transport from the aortic valve.
High HDL levels are mainly the result of genetic factors, but environmental factors also play a part. In view of this fact, from the standpoint of long-term primary prevention of CAD, our results suggest that measures designed to raise HDL levels may have an important prophylactic role in individuals with multiple risk factors and low or intermediate HDL levels. To date, primary prevention of CAD has been based on non-pharmacological (lifestyle modification) and pharmacological measures (in practice, statins alone or combined with ezetimibe, both intended to modify various risk factors and to reduce LDL cholesterol.31 However, the various interventions available to clinicians designed to raise HDL cholesterol have only mild to moderate effects, whether used in isolation or in combination. The most powerful drug currently available for raising HDL is sustained-release nicotinic acid (niacin), which at high doses results in moderate rises in HDL, but the therapeutic regimen required to prevent side-effects, particularly flushing, is complex and inconvenient. The association of niacin with laropiprant, a selective inhibitor of the DP1 receptor of vasodilatory prostaglandins (particularly PGD2) in cutaneous vessel walls, now allows the use of high doses of nicotinic acid with much less likelihood of flushing.32 At high doses, niacin has been shown to have promising antiatherogenic properties,22,23 but its use in diabetic patients, considered to be its main target, has been slow in gaining widespread acceptance.33
New and more powerful HDL-raising drugs with different effects on HDL metabolism are being investigated.22,23 Around five years ago, the most thoroughly researched drug was torcetrapib (a CETP inhibitor that led to rises of 40–100% in HDL cholesterol), but a large phase III randomized clinical trial (ILLUMINATE) was terminated due to an excess of mortality and cardiovascular events in the torcetrapib arm.23 The deaths and events, which were preceded by a rise in blood pressure, can be explained by torcetrapib's stimulation of aldosterone production that was independent of its effect on CETP.32 Torcetrapib's induction of aldosterone release, which is not seen in other, structurally different CETP inhibitors such as dalcetrapib,34 acts through a different pathway from that used by angiotensin II; it appears to be mediated by l-type calcium channels and is inhibited by nifedipine.34 Despite rises of over 70% in HDL, torcetrapib's adverse cardiovascular effects meant that it failed to halt or slow the progress of atherosclerosis in most patients, although those with the greatest increases in HDL had the lowest rates of adverse cardiovascular events.32
This incident highlights a key point: more important than raising absolute HDL levels is to enhance the effects of the most protective subclasses without triggering adverse effects, and thus increase their antiatherogenic potential. Nicotinic acid has been shown to have an antiatherogenic effect by raising the HDL-2 fraction of HDL and by significantly reducing the small and dense fractions of LDL, but torcetrapib did not show positive clinical results despite being associated with an increase in the average size of HDL particles.25 Furthermore, individuals with the ApoA-I Milano mutation in apolipoprotein A-I, which is associated with very low HDL, are highly resistant to the development of CAD22; experimental studies and a small clinical trial with parenteric administration of recombinant ApoA-I Milano have shown very promising antiatherogenic effects.22,23,27 Other research is continuing into peptides that mimic apolipoprotein A-I, with the aim of improving HDL function without necessarily raising plasma HDL levels.23,32 Similar lines of research are focusing on the development of more powerful selective agonists of liver X receptor and PPAR alpha than currently used fibrates.32
It is hoped that in the near future drugs that substantially improve HDL function will be available in clinical practice. If so, therapeutic strategies for long-term primary and secondary prevention of CAD should undergo a radical change and become hybrid, focusing mainly on improving HDL function, in association with measures to lower LDL. Improving HDL function will probably consist in achieving effective but appropriate rises in plasma HDL levels.24
ConclusionsElevated HDL is the main protective factor (negative risk factor) for CAD in elderly CAVD patients.
Although it is involved in the dyslipidemia associated with valve degeneration, HDL does not appear to have any protective effect in the pathophysiology of CAVD.
In elderly high-risk patients with mild to moderate dyslipidemia, elevated HDL is the main negative risk factor for CAD. Therapeutic strategies for long-term primary and secondary prevention of CAD should undergo a radical change in the near future and become hybrid, focusing mainly on improving HDL function by achieving effective but appropriate rises in plasma HDL levels, in association with measures to lower LDL.
Conflict of interestDr. A.D.B. Bordalo has given unpaid lectures sponsored by Laboratórios Pfizer, Abbott, Merck Sharp & Dohme, Merck Serono, Novartis, and Medinfar. The other co-authors have no conflicts of interest to declare.
We are grateful to Dr. Nilza Gonçalves (KeyPoint, Consultoria Científica) for her assistance with the statistical analysis.
We thank Merck Serono for the grant that funded the statistical analysis.
Please cite this article as: Bordalo, ADB. Um valor elevado de HDL é o principal factor protector contra a doença coronária no idoso com doença fibrocalcificante valvular aórtica. Rev Port Cardiol 2012. doi:10.1016/j.repc.2011.12.018